Indapamide
Undesirable drug combinations
— Lithium preparations:
With the simultaneous use of indapamide and lithium preparations, as well as when following a salt-free diet, an increase in the concentration of lithium in the blood plasma may be observed due to a decrease in its excretion, accompanied by the appearance of signs of overdose. If necessary, diuretics can be used in combination with lithium preparations, and the lithium content in the blood plasma should be monitored and the dose of the drug should be adjusted accordingly.
Combinations of drugs requiring special attention
- Drugs that can cause aritis:
- class I A antiarrhythmic drugs (quinidine, hydroquinidine, disopyramide);
- class III antiarrhythmic drugs (amiodarone, sotalol, dofetilide, ibutilide);
- some neuroleptics: phenothiazines (chlorpromazine, cyamemazine, levomepromazine, thioridazine, trifluoroperazine), benzamides (amisulpride, sulpiride, sultopride, tiapride). butyrophenones (droperidol, haloperidol);
- others: bepridil, cisapride, difemanil, erythromycin (iv), halofantrine, mizolastine, pentamidine, sparfloxacin, moxifloxacin, vincamine (iv), astemizole.
Increased risk of developing ventricular arrhythmias, especially arrhythmias (hypokalemia is a risk factor).
It is necessary to determine the potassium content in the blood plasma and. if necessary, adjust it before starting combination therapy with indapamide and the above drugs. It is necessary to monitor the patient’s clinical condition, monitor the level of electrolytes in the blood plasma, and ECG indicators.
In patients with hypokalemia, drugs that do not cause ari should be used.
— Systemic non-steroidal anti-inflammatory drugs, including selective cyclooxygenase-2 (COX-2) inhibitors, high doses of acetylsalicylic acid (≥ 3 g/day):
The antihypertensive effect of indapamide may be reduced. There is a risk of developing acute renal failure due to a decrease in glomerular filtration rate. Patients need to compensate for fluid loss and carefully monitor renal function at the beginning of therapy.
— Angiotensin-converting enzyme (ACE) inhibitors:
Prescribing ACE inhibitors to patients with low sodium levels in the blood (especially patients with renal artery stenosis) is accompanied by a risk of sudden arterial hypotension and/or acute renal failure.
For patients with arterial hypertension
and, possibly, due to the reduced content of sodium ions in the blood plasma due to the use of diuretics, it is necessary to:
- 3 days before starting therapy with an ACE inhibitor, stop taking the diuretic. In the future, if necessary, the diuretic can be resumed;
- or start ACE inhibitor therapy with low doses, followed by a gradual increase in dose if necessary.
For chronic heart failure
Therapy with ACE inhibitors should be started with low doses, with a possible preliminary reduction in diuretic doses.
In all cases, in the first week of taking ACE inhibitors in patients, it is necessary to monitor renal function (plasma creatinine content).
— Other drugs that can cause hypokalemia: amphotericin B (iv), gluco- and mineralocorticosteroids when used systemically, tetracosactide, laxatives that stimulate intestinal motility:
Increased risk of hypokalemia (additive effect). Constant monitoring of potassium concentration in the blood plasma and, if necessary, its correction is necessary. It is recommended to use laxatives that do not stimulate intestinal motility.
- Baclofen:
There is an increase in the hypotensive effect. Patients need to compensate for fluid loss and carefully monitor renal function at the beginning of treatment.
— Cardiac glycosides:
Hypokalemia enhances the toxic effect of cardiac glycosides. With the simultaneous use of indapamide and cardiac glycosides, the content of potassium in the blood plasma, ECG parameters should be monitored and, if necessary, therapy should be adjusted.
Drug combinations requiring attention
— Potassium-sparing diuretics (amiloride, spironolactone, triamterene):
Combination therapy with indapamide and potassium-sparing diuretics is advisable in some patients, but the possibility of developing hypokalemia or hyperkalemia cannot be excluded (especially in patients with renal failure or in patients with diabetes mellitus).
It is necessary to monitor the potassium content in the blood plasma, ECG indicators and, if necessary, adjust therapy.
— Metformin:
Functional renal failure, which can occur against the background of diuretics, especially loop diuretics, with simultaneous administration of metformin increases the risk of developing lactic acidosis. Metformin should not be used if creatinine levels exceed 15 mg/L (135 µmol/L) in men and 12 mg/L (110 µmol/L) in women.
— Iodine-containing contrast agents:
In case of dehydration while taking diuretics, the risk of developing acute renal failure increases, especially when using high doses of iodine-containing contrast agents. Before using iodinated contrast agents, patients need to compensate for fluid loss.
— Tricyclic antidepressants, antipsychotics (neuroleptics):
Drugs in these classes enhance the antihypertensive effect of indapamide and increase the risk of orthostatic hypotension (additive effect).
— Calcium salts:
With simultaneous administration, hypercalcemia may develop due to a decrease in the excretion of calcium ions by the kidneys.
- Cyclosporine, tacrolimus:
It is possible to increase the creatinine content in the blood plasma without changing the concentration of circulating cyclosporine, even with normal fluid and sodium ion levels.
— Corticosteroid drugs, tetracosactide (for systemic use):
Reduced hypotensive effect (retention of fluid and sodium ions as a result of the action of corticosteroids).
Indapamide, 30 pcs., 2.5 mg, film-coated tablets
Undesirable combination of drugs
Lithium preparations
With the simultaneous use of indapamide and lithium preparations, an increase in the concentration of lithium in the blood plasma may be observed due to a decrease in its excretion, accompanied by the appearance of signs of overdose. If necessary, diuretic drugs can be used in combination with lithium drugs, and the dose of the drugs should be carefully selected, regularly monitoring the lithium content in the blood plasma.
Combination of drugs requiring special attention
Drugs that can cause aritis:
- class IA antiarrhythmic drugs (hydroquinidine (quinidine), disopyramide), class III antiarrhythmic drugs (amiodarone, dofetilide, ibutilide), sotalol;
- some neuroleptics: phenothiazines (chlorpromazine, cyamemazine, levomepromazine, thioridazine, trifluoroperazine), benzamides (amisulpride, sulpiride, sultopride, tiapride), butyrophenones (droperidol, haloperidol);
- others: bepridil, cisapride, difemanil, erythromycin (iv), halofantrine, mizolastine, pentamidine, sparfloxacin, moxifloxacin, astemizole, vincamine (iv).
Increased risk of ventricular arrhythmias, especially arrhythmias (risk factor: hypokalemia)
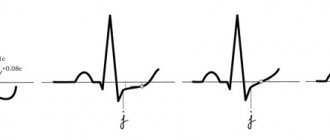
The potassium content in the blood plasma should be determined and, if necessary, adjusted before starting combination therapy with indapamide and the above drugs. It is necessary to monitor the patient’s clinical condition, monitor blood plasma electrolytes, and electrocardiogram (ECG) indicators.
In patients with hypokalemia, drugs that do not cause ari should be used.
Non-steroidal anti-inflammatory drugs (when administered systemically), including selective COX-2 (cyclooxygenase-2) inhibitors, high doses of salicylates (≥3 g/day)
The antihypertensive effect of indapamide may be reduced.
With significant fluid loss, acute renal failure may develop (due to a decrease in glomerular filtration rate). Patients need to compensate for fluid loss and carefully monitor renal function at the beginning of treatment.
Angiotensin-converting enzyme (ACE) inhibitors
Prescribing ACE inhibitors to patients with a reduced concentration of sodium ions in the blood (especially patients with renal artery stenosis) is accompanied by a risk of sudden arterial hypotension and/or acute renal failure.
Patients with arterial hypertension and possibly reduced levels of sodium ions in the blood plasma as a result of taking diuretics should: stop taking diuretics 3 days before starting treatment with an ACE inhibitor. In the future, if necessary, diuretics can be resumed. Or start ACE inhibitor therapy with low doses, followed by a gradual increase in dose if necessary.
In chronic heart failure, treatment with ACE inhibitors should begin with low doses with a possible preliminary reduction in the doses of diuretics.
In all cases, in the first week of taking ACE inhibitors in patients, it is necessary to monitor renal function (plasma creatinine concentration).
Other drugs that can cause hypokalemia: amphotericin B (iv), gluco- and mineralocorticosteroids (if administered systemically), tetracosactide), laxatives that stimulate intestinal motility
Increased risk of hypokalemia (additive effect).
Regular monitoring of potassium levels in blood plasma is necessary; if necessary, its correction. Particular attention should be paid to patients concomitantly receiving cardiac glycosides. It is recommended to use laxatives that do not stimulate intestinal motility.
Baclofen
There is an increase in the antihypertensive effect.
Patients need to compensate for fluid loss and carefully monitor renal function at the beginning of treatment.
Cardiac glycosides
Hypokalemia enhances the toxic effect of cardiac glycosides.
With the simultaneous use of indapamide and cardiac glycosides, the content of potassium in the blood plasma, ECG indicators should be monitored, and, if necessary, therapy should be adjusted.
Combination of drugs requiring attention
Potassium-sparing diuretics (amiloride, spironolactone, triamterene, eplerenone (spironolactone derivative))
Combination therapy with indapamide and potassium-sparing diuretics is advisable in some patients, but the possibility of developing hypokalemia (especially in patients with diabetes mellitus and patients with renal failure) or hyperkalemia cannot be excluded.
It is necessary to monitor the potassium content in the blood plasma, ECG indicators and, if necessary, adjust therapy.
Metformin
Functional renal failure, which can occur against the background of diuretics, especially loop diuretics, with simultaneous administration of metformin increases the risk of developed lactic acidosis.
Metformin should not be used if the creatinine concentration exceeds 15 mg/l (135 µmol/l) in men and 12 mg/l (110 µmol/l) in women.
Iodinated contrast agents
Dehydration while taking diuretics increases the risk of developing acute renal failure, especially when using high doses of iodinated contrast agents.
Before using iodinated contrast agents, patients need to compensate for fluid loss.
Tricyclic antidepressants, antipsychotics (neuroleptics)
Drugs in these classes enhance the antihypertensive effect of indapamide and increase the risk of orthostatic hypotension (additive effect).
Calcium salts
With simultaneous administration, hypercalcemia may develop due to a decrease in the excretion of calcium ions by the kidneys.
Cyclosporine, tacrolimus
It is possible to increase the concentration of creatinine in the blood plasma without changing the concentration of circulating cyclosporine, even with normal fluid and sodium ion levels.
Corticosteroid drugs, tetracosactide (if administered systemically)
Decreased antihypertensive effect (retention of fluid and sodium ions as a result of the action of corticosteroids).
Clinical efficacy of indapamide in patients with hypertension
G
Hypertension (HD) is one of the leading causes of disability and mortality. A prolonged increase in blood pressure (BP) leads to target organ damage and the development of cardiovascular complications (heart failure, myocardial infarction, cerebral stroke and renal failure) [2, 3, 8].
Drugs for the treatment and prevention of complications of hypertension should have high therapeutic efficacy, a long-lasting antihypertensive effect throughout the day, and the absence of metabolic side effects [3, 4, 8].
The listed requirements are fully met by the drug belonging to the second generation of thiazide and thiazide-like diuretics, indapamide
. The mechanism of its antihypertensive action is associated with inhibition of sodium reabsorption in the distal convoluted tubules and the development of peripheral vasodilation [6]. Unlike hydrochlorothiazide, indapamide does not affect lipid and carbohydrate metabolism [7, 9]. One of the advantages of the drug is the ability to reduce the mass of hypertrophied left ventricular myocardium [5].
Indapamide has high bioavailability (90–95%) and a long half-life (15–25 hours), which allows for a stable antihypertensive effect throughout the day [4].
The purpose of the study conducted in our clinic was to evaluate the effectiveness and safety of indapamide under conditions of 24-hour blood pressure monitoring (ABPM), studying central hemodynamics under the control of a number of parameters of the biochemical spectrum of blood.
The study included 30 patients (12 men and 18 women) with stage I and II hypertension (according to WHO classification). The average age of the group was 47.1±11.5 years, the duration of the disease was 8.0±7.05 years. 10 patients had mild and 20 had moderate arterial hypertension (AH). Patients with symptomatic hypertension, unstable angina, previous myocardial infarction or acute cerebrovascular accident in the last 6 months, a history of liver and kidney diseases, and intolerance to sulfonamides were excluded from the study. The duration of observation was 8 weeks.
After an introductory period, during which patients did not receive antihypertensive therapy, indapamide (Hemofarm, Yugoslavia) was prescribed at a daily dose of 2.5 mg, once in the morning. If monotherapy was ineffective for 1 month, enalapril (Hemofarm, Yugoslavia) was added at a daily dose of 5–20 mg. At baseline and after 8 weeks of treatment, antihypertensive efficacy using ABPM, the effect on central hemodynamic parameters, and levels of electrolytes and blood lipids were assessed in all patients.
ABPM was carried out using a portable recorder ABRM-04 from Meditech (Hungary), which records blood pressure and heart rate during the decompression phase using the oscillometric method. Measurements began at 9–10 am. The intervals between blood pressure and heart rate measurements were 15 minutes during the day and 30 minutes at night. Based on ABPM data, we analyzed the average indicators of systolic blood pressure (SBP), diastolic blood pressure (DBP), heart rate during periods of wakefulness, sleep and for the day as a whole, standard deviation to assess the variability of blood pressure and heart rate; degree of nocturnal reduction in blood pressure (SNS – percentage of reduction in blood pressure at night); percentage of blood pressure measurements exceeding the upper limit of normal in the total number of registrations; variability index. Blood pressure levels below 140/90 mmHg are considered normal. Art. during the day and below 120/70 mm Hg. Art. at night. Central hemodynamics were studied using an Acuson apparatus (USA).
Results and discussion
Before starting treatment, patients complained of headache (63%), dizziness (37%), pain in the heart of various types (27%), decreased performance (50%). 23% of patients had no complaints. According to ABPM data (Table 1), there was an increase in the average daytime, average nighttime and average daily values of SBP and DBP. The proportion of measurements that exceeded the norm, as well as the variability index, exceeded the permissible normative values, which indicated an increase in hypertensive load. The degree of nocturnal decrease (NNR) for SBP was 10.0±6.0%, for DBP – 13.0±7.5%, which corresponds to the “dipper” group. Initially, indicators of central hemodynamics (Table 2) such as average blood pressure per day and total peripheral vascular resistance (TPVR) were significantly increased.
After 8 weeks of therapy, clear positive dynamics were noted in the patients’ condition. The general well-being of the patients improved, dizziness decreased or disappeared (in 82%), headaches (in 58%), cardialgia (in 100%), and performance increased (in 80%). All patients had good tolerability of treatment, there were no side effects.
When assessing the data obtained, normalization of DBP (decrease to 90 mm Hg or lower) was considered a good result of treatment; a satisfactory result was a decrease in DBP by 10 mm Hg. Art. and more (but not to normal values), unsatisfactory - a decrease in DBP by less than 10 mm Hg. Art. or increased blood pressure. In 16 patients receiving monotherapy with indapamide, the antihypertensive result was assessed as good, in 2 patients - as satisfactory. Thus, 60% of patients achieved an effect during treatment with indapamide, which corresponds to the available literature data on the effectiveness of monotherapy [8].
There was a significant decrease in SBP per day, day, night by 14.5, 14.9 and 18 mm Hg. Art., respectively. Average daily, daytime, and nighttime DBP decreased by 8.8, 8.9, and 14.3 mmHg, respectively. Art. A significant decrease in the blood pressure variability index was revealed. Particularly noteworthy is the decrease in the absolute value of DBP and the DBP variability index, since changes in these indicators correlate with target organ damage [10]. During treatment, an unreliable increase in the SNS was noted, not exceeding 20%. The above indicates that a single dose of indapamide 2.5 mg is sufficient to maintain normal blood pressure throughout the day without affecting the physiological circadian rhythm of blood pressure.
When analyzing central hemodynamics during monotherapy with indapamide, a significant decrease in average blood pressure per day (p <0.01) and total peripheral resistance (p <0.05) was revealed, which largely explains the predominant effect of indapamide on DBP (Table 2). The dynamics of shock and cardio indices were statistically insignificant.
Twelve patients received combination therapy (indapamide 2.5 mg/day + enalapril 5–20 mg/day). At the same time, there was a significant decrease in SBP and DBP per day, day and night (Table 1), and the BP variability index. SNS increased slightly within the “dipper” group, that is, there was also no change in the circadian rhythm of blood pressure. According to echocardiography, there was a significant decrease in average blood pressure per day by 7.2% (p<0.01), peripheral vascular resistance by 13.3% (p<0.05), other indicators changed unreliably (Table 2). In 8 patients receiving combination therapy with indapamide and enalapril, the antihypertensive result was assessed as good, in 2 patients as satisfactory, in 2 patients as unsatisfactory, and therefore required the addition of verapamil at a dose of 120 mg per day. After 8 weeks of indapamide therapy, an insignificant decrease in the levels of sodium (from 142.4±2.9 to 140.4±2.3 mmol/l) and potassium (from 4.4±0.4 to 3.96±0.3) was noted mmol/l) in blood serum. Not a single patient had electrolyte levels (and, most importantly, potassium) that dropped below normal values. There were also no significant changes in the content of cholesterol and triglycerides compared to the initial level.
conclusions
1. Indapamide is a highly effective antihypertensive drug for the treatment of patients with mild and moderate forms of hypertension.
2. Considering the effect of indapamide on the peripheral vascular resistance, the drug can be prescribed primarily for diastolic hypertension.
3. The metabolic inertness of indapamide, unlike thiazides, makes it possible to recommend it to patients with hypertension in combination with metabolic disorders.
4. Adding enalapril to indapamide (if monotherapy is insufficiently effective) allows you to achieve the target blood pressure level.
Indapamide -
Indapamide (trade name)
(Hemofarm)
Literature:
1. Bulkina O.S., Dobrovolsky A.B., Britareva V.V., Marenich A.V., Karpov Yu.A. Ross. cardiol. magazine 1999; 1:39–42.
2. Gogin E.E. Hypertonic disease. M.; 1997.
3. Makolkin V.I., Podzolkov V.I. Hypertonic disease. – M.; 2000.
4. Sidorenko B.A., Preobrazhensky D.V. Diagnosis and treatment of arterial hypertension. Part two. Diuretics. M.; 2000.
5. Campbell DB, Brackman FJ Clin. Pharmacol. 1991; 31: 751–757.
6. Campbell DB, Moore R. Am. J. Hypertens. 1981; 57: 7–17.
7. FuJii S., Kaku K., Andou S., Nakayama H. et al. Clin. Ther. 1993; 15:6.
8. Hanson L., Hedner T. Hypertension Manual. 3rd ed., 2000.
9. Weidmann P., M. De Courten, P. Ferrari, Lorenz Bohlen. J. Cardiovasc. Pharmacol. 1993; 22(Suppl. 6): 98–105.
10. White WB, Dey HM, Schulman P. Am. Heart J 1989; 118:782–795.