Drugs to prevent heart disease
Healthy heart
It is impossible to treat the heart or prevent problems with it in isolation from the whole organism. Yes, the heart is the most important organ that works throughout life and ensures blood circulation in our body. But for its normal operation, it is necessary to provide it with optimal operating conditions. The heart itself is a muscular organ. This means that to contract muscle cells (cardiomyocytes), oxygen, nutrients, and removal of metabolic products are required. The coronary vessels surround the heart muscle and supply it with blood.
For coordinated work with other organs, it is connected with them through the nervous system and hormones circulating in the blood into one whole. We run and our heart beats faster, but at night, on the contrary, it slows down. Blood viscosity and its quantity also affect the functioning of the heart. The condition of the arteries and veins also determines whether it is easy or difficult to pump blood. Even physical activity can help in its work. Thus, the muscles of the foot and lower leg can rightfully be considered a “second heart”, since their contractions when walking help overcome the force of gravity and return blood upward through the vessels.
The work of the parts of the heart themselves must be coordinated with each other. Full contractions of the ventricles and atria should alternate with periods of relaxation when the muscle “rests”.
How the disease develops
Our body has a large margin of safety against damage and the ability to adapt even if some of the mechanisms “break down”. That is, the disease does not appear immediately. Atherosclerosis is considered one of the main causes of heart problems. It leads to damage to the walls of blood vessels and a gradual narrowing of its lumen. These processes continue for many years and can proceed completely unnoticed. This means that when any symptom of problems with the heart or blood vessels appeared, the body stopped coping with them. It is impossible to predict in advance where an atherosclerotic plaque will grow in a coronary vessel, on the wall of the heart valve or in the arteries of the brain. It can also break away from the wall of the vessel and clog any narrow artery with the blood flow. In this case, could there be a “magic pill” that, by taking it, can “clean” blood vessels or cure the heart? Unfortunately no. After all, even after coronary artery bypass surgery there are no guarantees that this will not happen again.
Risk factors
It turned out that the presence or absence of risk factors plays a major role in the prevention of problems with the heart and blood vessels. The same ones that accumulate their potential for many years, and then “suddenly” are realized in the form of heart attacks and strokes.
Risk factors:
- Arterial hypertension
- Hypercholesterolemia
- Smoking
- Insufficient consumption of vegetables and fruits
- Excess body weight
- Excessive alcohol consumption
- Physical inactivity
It is these factors that act for many years that lead to irreversible changes. Only by eliminating them and replacing them with the opposite ones can effective prevention of heart disease be carried out. If we talk about hereditary predisposition, then they will play even more importance.
For those people who already have heart problems, secondary prevention is necessary to avoid a recurrence of the acute situation. It also involves eliminating risk factors. But it also adds treatment and control of existing diseases.
Prevention
In addition to lifestyle changes, nutrition, and physical activity, various medications can be used to prevent heart disease. The purpose of their use is to reduce risk factors if this could not be done without drugs. In practical medicine, a doctor cannot force a patient to quit smoking, eat less and move more; the person must do this himself. You can start taking medications only as prescribed by a doctor, after undergoing tests and studies, since each drug has contraindications, and their combinations can increase side effects. Compliance with the treatment regimen will help correct current problems that directly affect the risk of heart attacks and strokes:
- Arterial hypertension
- Arrhythmias
- Cardiac ischemia
- Atherosclerosis
- "High" cholesterol
- Diabetes
- Obesity
Drugs
Statins . Taking statins helps fight hyperlipidemia and prevents the development of atherosclerosis. Helps stabilize the surface of cholesterol plaques, which prevents the formation of blood clots. Taking these medications is necessary for life with periodic monitoring of biochemical blood tests for liver function. Therefore, before taking them, you should make every effort to correct your lipid profile first through diet. Some of the modern and studied statins are Crestor and Mertenil.
Antihypertensive drugs
- Angiotensin converting enzyme inhibitors Diroton, Prestarium A, Hartil
- Angiotensin receptor blockers Valsacor, Aprovel
- Beta blockers Concor, Betalok
- Calcium antagonists Verapamil, Normodipine
- Diuretics Hypothiazide, Arifon-retard
There are many groups of drugs with this effect. Their selection is made only by a specialist, since they may have additional effects on slowing heart rate when interacting with other drugs. Also, a combination of 2 several groups may be more effective. The bottom line is that even a decrease in pressure by only 5-10 mmHg. already reduces the risk of disaster.
Antiplatelet agents . Help prevent the formation of blood clots and improve blood flow. Must be prescribed by a doctor, as they can lead to bleeding. Aspirin is most often prescribed. Curantil, Clopidogrel, Pentoxifylline can also be used.
Antianginal drugs . Helps cope with attacks of ischemic pain during angina attacks. The most famous drug is Nitroglycerin
Metabolic drugs. Not all drugs in this group have a broad evidence base, but are also used in practice. They are designed to improve metabolic processes in cells and protect them from ischemia. These include Preductal (trimetazidine), Mildronate, ATP, cocarboxylase, Neoton.
It is also necessary to effectively treat diabetes mellitus, as it provokes the progression of atherosclerosis.
Prevention can only be effective in combination, and medications only provide support where our efforts and the body’s capabilities are exhausted.
Literature:
PREVENTION OF CHRONIC NON-INFECTIOUS DISEASES. PRIMARY AND SECONDARY PREVENTION OF CARDIOVASCULAR DISEASES. Recommendations 2013
Clinical recommendations. Arterial hypertension in adults. Russian Society of Cardiology 2019
Possibilities and limitations of modern anti-ischemic therapy.
Oksana Mikhailovna Drapkina , professor, doctor of medical sciences:
– The next lecture by Professor Sergei Rudzherovich Gilyarevsky is “Possibilities and limitations of modern anti-ischemic therapy.” Professor Gilyarevsky became the editor-in-chief of the first online journal “Internist Forum”. Dear colleagues, please come in, because the content will be shaped by your activity.
Sergey Rudzherovich Gilyarevsky , professor, doctor of medical sciences:
– Dear colleagues, the problems of angina pectoris attract the attention of doctors around the world for two reasons. Firstly, angina pectoris significantly worsens the patient’s quality of life, and the second reason is that there are a lot of such patients. In the United States alone, today 10 million patients have angina and approximately 33 million people in this country are at high risk of developing coronary heart disease. Between the ages of 60 and 79, every fourth man has coronary heart disease and every sixth woman. There is ongoing debate about whether myocardial ischemia is a true risk factor influencing prognosis or a marker reflecting more severe coronary atherosclerosis. But it is obvious that such a connection exists.
The results of the MERLIN-TIMI 36 study showed that in women who suffered acute coronary syndrome, the presence of even one attack of myocardial ischemia significantly worsened the prognosis.
The results of observational studies also indicated that the presence of myocardial ischemia, even in the absence of coronary atherosclerosis in women, is accompanied by a deterioration - approximately 3 times - in the risk of developing complications of coronary heart disease compared with middle-aged and elderly women who did not have manifestations of ischemia myocardium.
Today, there is a lot of discussion about what is best for the treatment of angina: invasive interventions, stenting or bypass surgery of the coronary arteries, or drug therapy. It became obvious that these methods and these approaches cannot be opposed. But, if we talk about patients who do not have life-threatening coronary lesions, but only angina, the results of the meta-analysis indicate that skin interventions on the coronary arteries do not lead to a reduction in mortality in patients with chronic ischemic heart disease, respectively , angina pectoris and does not lead to a reduction in the risk of developing myocardial infarction, but still the anti-ischemic effect of revascularization is somewhat better than drug therapy alone. These data suggest that optimization of anti-ischemic therapy should be considered a very important approach to the treatment of patients with stable coronary artery disease.
We must not forget that the task of examining a patient with a stable course of coronary heart disease includes the mandatory identification of those lesions that threaten life. This is stenosis of the left main coronary artery, stenosis of three large cardiac arteries or the proximal part of the left anterior descending artery in combination with stenosis of another large artery. And revascularization is indicated in resuscitated patients in cases where it is assumed that coronary lesions were the cause of sudden death.
Speaking about drug therapy, it should be recalled once again that in all clinical recommendations, in the American recommendations of 2012, drugs that affect heart rhythm, in particular beta blockers, are classified as first-line drugs. That is, this emphasizes the importance of reducing heart rate as one of the important approaches to improving exercise tolerance and reducing angina attacks, since we remember that each patient develops an angina attack at a certain double product and, accordingly, reducing heart rate is an important approach to reducing the number of angina attacks.
In the 2013 European guidelines for the treatment of patients with stable coronary heart disease, drugs that reduce heart rate are considered first-line drugs and have a recommendation class of I. All other drugs are classified as second-line drugs and have a recommendation class of either II-A or II-B. It is believed that in some cases, second-line drugs may become first-line drugs if the patient does not tolerate standard anti-ischemic drugs.
Indeed, today it has become obvious that the hemodynamic actions of anti-ischemic drugs may not always be beneficial for a patient with coronary heart disease. Results from a secondary analysis of the very large INVEST study, which included patients with hypertension and coronary artery disease, indicated that a decrease in diastolic blood pressure of less than 70 millimeters of mercury significantly increases the risk of myocardial infarction. And thus, it became obvious that we cannot always use anti-ischemic drugs with a hemodynamic effect.
Today, those target blood pressure levels that have existed for a long time for patients with stable coronary heart disease have been revised, and now this bar, accordingly, is 140/90, and this also reflects the concern about the deterioration of perfusion with a decrease in blood pressure levels. Thus, we are not always able to give the patient the target dose of a beta blocker, the target dose of a calcium antagonist, which leads to a decrease in blood pressure.
Obviously, nitrates are also not optimal anti-ischemic drugs, nitrates taken for long-term prevention of angina attacks. This is due to the fact that the opinion about nitrates leads to a deterioration in endothelial function. You see the results of a study in which it was shown that while taking isosorbitol-5-mononitrate, there was a significant decrease in vasodilation of the brachial artery when administered acetylcholine (yellow bars in contrast to placebo - blue bars), which indicates that long-term use of nitrates leads to to deterioration of endothelial function, tolerance to the action of nitrates develops. This tolerance can be overcome by eccentrically taking the drug, but this increases the risk of developing myocardial ischemia at the end of the drug’s action, that is, one day before taking the next dose.
Be that as it may, experts believe that, in general, the evidence base for anti-ischemic therapy in patients with stable coronary heart disease is not very good. This is due to the fact that all studies were carried out evaluating old drugs, such beta blockers as propranolol, atenolol, metoprolol, calcium channel blockers - nifedipine, diltiazem and verapamil.
The evidence base for second-line drugs is, in general, no worse or better than first-line drugs. In particular, the TRIMPOLL II study clearly demonstrated that the addition of trimetazidine to metoprolol resulted in a significant improvement in exercise capacity.
In our country, trimetazidine remains a popular drug, and the emergence of generic versions of trimetazidine reflects the continued need for the use of this drug. Therefore, it is useful to answer the question - how different is the anti-ischemic effect of trimetazidine from the use of other anti-ischemic drugs that do not affect the heart rate.
A network meta-analysis was performed to answer this question. Network meta-analysis is considered to be the most advanced type of meta-analysis today because it can reduce the heterogeneity of the data included in the meta-analysis and evaluate the true role of the significance of the effectiveness of each drug studied, even in cases where different drugs were not compared in different studies. during the course of one study.
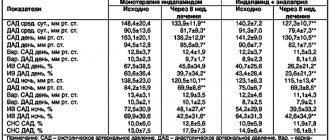
So, a network meta-analysis was performed in which they tried to answer the question of how the use of trimetazidine differs from standard anti-ischemic drugs that do not affect heart rate, compared to placebo, and compared to each other. These drugs were compared: dihydropyridine calcium antagonists, nitrates, nicorandil and ranolazine, and, accordingly, trimetazidine.
This was a fairly large meta-analysis, it included data on almost 20 thousand patients with stable coronary heart disease. The duration of exercise tolerance, the duration of exercise until the ST segment decreased by 1 millimeter, the duration of exercise before the development of an angina attack, the number of angina attacks, and the need to use short-acting nitrates to relieve an attack were assessed. That is, during this study, the evaluation criteria that we always use to evaluate anti-ischemic drugs were used.
It turned out that the use of trimetazidine has a statistically significant effect on exercise tolerance in the same way as other second-line anti-ischemic drugs and dihydropyridine calcium antagonists. Moreover, according to this meta-analysis, the effectiveness of trimetazidine was higher than the effectiveness of ranolazine. The last three lines are ranolazine, the first three lines are trimetazidine. It can be seen that according to some indicators, the use of trimetazidine was statistically significantly more effective.
Finally, in comparison with other anti-ischemic drugs, this tree graph shows that the use of trimetazidine did not differ in effectiveness from other second-line anti-ischemic drugs and dihydropyridine calcium antagonists.
It should be noted that trimetazidine is not available in all countries. In particular, another second-line drug, ranolazine, has become more widespread in the United States. But, nevertheless, in the latest version of the American recommendations, a whole paragraph is devoted to trimetazidine, where it is said that this drug has an anti-ischemic effect and is used quite widely in more than 80 countries around the world. Thus, I want to emphasize once again that the emergence of effective generics of trimetazidine reflects the popularity of this drug not only in our country, but also in many other countries.
Well, the last topic that I would like to discuss is the pleiotropic effects of trimetazidine. The fact is that the trimetazidine molecule attracted the attention of not only doctors, but also researchers. And at one time I was amazed by the results of a Finnish study that were published in the journal Circulation. This study included patients with traditional cardiomyopathy in whom coronary heart disease, coronary artery disease, and myocardial ischemia were strictly excluded.
In this study, extended-release trimetazidine was added to standard therapy for such severe patients with cardiomyopathy, or patients received placebo, also in combination with standard therapy. We observed for three months and after three months we got these results. It turned out that in the trimetazidine group there was a clear trend towards an increase in ejection fraction, while in the placebo group the ejection fraction continued to decrease against the background of the natural history of traditional cardiomyopathy.
These data suggest that trimetazidine has some effect that is responsible for the positive effect on ejection fraction. Not long ago, a meta-analysis was published in the Journal of the American College of Cardiology, which also assessed the effects of long-term use of trimetazidine, which were evaluated in more than ten clinical studies, and it turned out that they obtained the same results as in that one. small study. In general, taking trimetazidine leads to an increase in ejection fraction and a decrease in end-systolic size, end-diastolic size, that is, it causes a decrease in cardiac remodeling in patients with chronic heart failure.
A meta-analysis of 16 clinical trials showed that trimetazidine tended to reduce mortality and tend to reduce the need for hospitalization.
Moreover, the results of an earlier meta-analysis suggested that trimetazidine even leads to a reduction in mortality in patients with ischemic cardiomyopathy, but, however, a slightly smaller number of patients were included in this meta-analysis. In any case, the fact that trimetazidine is included in the latest version of the Russian recommendations for the treatment of heart failure as a drug that is recommended for use in patients with heart failure and against the background of coronary heart disease probably reflects these data.
Well, finally, there is evidence that suggests that long-term use of trimetazidine before the development of myocardial infarction leads to a decrease in reperfusion damage. This was a secondary analysis of an observational study that attempted to answer the question of what the prognosis would be for the development of myocardial infarction in patients with stable angina who received various anti-ischemic drugs before the infarction, including trimetazidine. And we received such interesting data. It turned out that the risk of developing an unfavorable outcome within 6 months after myocardial infarction was significantly lower if patients used trimetazidine before the heart attack.
With what it can be connected? Of course, this is the result of an observational study, especially a retrospective one, but, nevertheless, there is convincing experimental evidence that taking trimetazidine leads to a change in the functioning of the so-called mega pore. A mega pore is a formation that, under conditions of ischemia, causes the flow of calcium into the mitochondria. So, all approaches that reduce the permeability of the megapore, in particular the use of trimetazidine, can experimentally reduce reperfusion damage, since to a large extent these damages are associated with a large flow of calcium into the mitochondria when blood flow is restored. This is also interesting data that should be taken into account when prescribing trimetazidine in patients with chronic coronary heart disease.
In conclusion, I would like to recall the words of Ernest Rutherford, who said that there are three stages of recognition of truth: the first is “this is absurd,” the second is “there is something in it,” and the third is “it is common knowledge.” Today, the role of trimetazidine and data on its effectiveness have probably already entered the third stage - it is well known that it is an effective and safe anti-ischemic drug, and the emergence of effective generics allows for wider use of this drug in the treatment of patients with coronary heart disease.