Angina pectoris 2 FC is a subacute malnutrition of cardiac structures with death of the muscle layer (one of the forms of coronary artery disease).
Externally, necrosis is manifested by intense chest pain, shortness of breath and rhythm disturbances. Attacks occur in response to physical or emotional stress and occur with varying frequency, but rarely last more than 30 minutes.
This is not the initial stage. Its formation takes from 2 to 5 years on average. Plus or minus.
A complete cure cannot be achieved, but with a competent course of therapy, the quality and length of life will not be affected.
How does pathology develop?
Normally, the heart, including muscle fibers, is supplied with blood, nutrients and oxygen through the coronary arteries.
During certain pathological processes, stenosis (narrowing) or occlusion (blockage) of these vessels occurs. Dystrophy of anatomical structures occurs, which ends with attacks of myocyte necrosis of varying frequency and intensity.
Then the contractility of the heart decreases, and both general and local hemodynamics are disrupted. Blood circulation in the heart suffers even more.
It turns out to be a vicious circle. The pathology worsens in a cyclical, independent manner. Starting from the second functional class, spontaneous regression should no longer be expected.
Angina pectoris differs from other forms by a provoking factor.
An episode of pain and symptoms develops due to intense physical activity or a strong emotion (negative most often, but possibly positive). Stress in general with an average manifestation of affect also has an effect.
The etiological aspects are somewhat different. In this regard, angina is a secondary process.
The primary ones are cardiac changes and vascular diseases. Often a person himself is the creator of his own condition. Patients who smoke and drink are especially at risk. Heredity plays a big role.
According to the classification, there are four functional classes (abbreviated FC). Each subsequent one imposes great restrictions on the patient’s physical activity (more details here).
At the last, fourth stage, attacks occur in a state of rest, and there are no prospects for cure.
Diagnosis of the disease
Basically, this type of disease is diagnosed based on the following examinations:
- examination and questioning of the patient;
- research in the laboratory;
- research using special equipment.
In the first case, after listening to the patient’s complaints, he compares them with symptoms characteristic of IHD. The basis of the examination is auscultation, thanks to which the doctor identifies heart rhythm disturbances and cardiac murmurs.
Laboratory tests include a coagulogram and a lipid profile, since only these two examinations can provide the necessary information for selecting the correct therapeutic treatment.
The list of instrumental studies includes such procedures as:
- coronary angiography;
- echocardiography;
- electrocardiography.
Using the above methods for diagnosing IHD, it is possible to identify not only the exact form of the disease, but also to establish a disability group.
Why is angina pectoris FC 2 dangerous?
The main threat is to cardiac structures.
An approximate list of complications:
- Heart failure. As a result of acute malnutrition, or as a result of prolonged ischemia. With stable angina, FC 2 occurs in 15% of cases. For progressive (unstable) forms - up to 30%.
- Heart attack. Avalanche-like myocardial necrosis. This is the only difference between the phenomena under consideration. It is the final stage of coronary artery disease and coronary insufficiency in general.
- Stroke. Death of nerve tissue of cerebral structures. Leads to the development of a permanent defect. Which one depends on the location of the lesion.
- Ischemia of the lower extremities, secondary atherosclerosis with the prospect of developing gangrene.
- Vascular dementia.
All conditions are potentially fatal and carry a risk of disability. Preventing dangerous consequences is one of the key goals of therapy.
Causes
We need to talk about three groups.
- The former act as provocateurs of angina attacks.
- The latter determine the pathological process at a fundamental level, making anatomical deviations possible.
- Still others increase the risk of developing the condition. If it already occurs, progression is accelerated.
Among the first
- Anger. The strongest negative emotion. As the affect increases, a large amount of corticosteroids is released. They provoke a narrowing of blood vessels, including the coronary arteries. Against the background of existing pathologies, this leads to the formation of an attack.
- Stress. The intensity of the affect may vary. If it is at a moderate level, “compensation” is achieved through duration. At high intensity, one episode is enough.
- Little physical activity. With FC 2, an attack is possible by simply moving up the stairs to 1-2 floors. Running, gym classes, and swimming are excluded. All activities lead to risk. At the second stage, it is not recommended to strain the body at all; this can end badly.
- Hypothermia affects. The only exception to the presented range of factors.
Second group of reasons
Etiological points:
- Atherosclerosis of the coronary arteries. It develops in almost every third person on the planet (according to American scientists).
The essence of the process is the deposition of cholesterol plaques on the walls of large vessels. As a result, the lumen narrows, blood passes through with great resistance, and blood pressure rises.
Tissue ischemia occurs, restoration is carried out using conservative methods. And in the case of deposition of calcium salts into lipid formations - through surgery.
Contrary to possible perception, not only elderly patients, but also young people, especially those who smoke and drink, are at risk of suffering from atherosclerosis. Not the least role is given to diet and nutritional errors.
- Endocrine diseases that provoke vasospasm. Hypercortisolism (excessive production of adrenal hormones), excessive synthesis of thyroid substances, diabetes mellitus as options. Recovery requires a long period of time. The likelihood of success depends not so much on the doctor himself, but on the patient’s willingness to follow all the specialist’s recommendations. In this case, the role of the patient as the creator of his own health is great.
- Vasculitis. Both primary, caused by viral and autoimmune causes, and secondary, developing as a result of systemic lupus erythematosus, rheumatism, and some forms of arthritis. The essence of the disease lies in inflammation of the vascular walls. Not selectively, but all in a row. The coronary arteries are also affected. Treatment is urgent, in a hospital. In the absence of competent assistance, the likelihood of complications increases. What consequences are possible? Vessel stenosis, closure of the lumen as a result of the formation of special strands. In such a situation, recovery is strictly surgical. Drugs are no longer enough.
- Arterial hypertension. Causes increased stress on the cardiac structures on one side. On the other hand, the root cause factor in the formation of the process plays a role. The release of angiotensin-II, renin, aldosterone, corticosteroids and others provokes a narrowing of the lumen of the coronary arteries. The dual mechanism leads to disruption of the normal functional activity of the heart. Angina pectoris is a clinical variant.
Attention:
In some cases, it is possible to develop an attack even at rest; a heart attack without preliminary symptoms is also typical.
- Congenital malformations of the coronary vessels. Anomalies lead to fusion, bends and other types of changes. Treatment is carried out surgically as necessary. But the connection between angina pectoris and abnormalities still needs to be confirmed. Because in reality they rarely turn out to be provocateurs of the disease.
- Compression of arteries by overgrown cardiac structures. As a result of hypertrophy of the ventricles, atria and other conditions. Removal is always surgical. The prospects are vague.
- Metabolic disorders. Usually we are talking about improper lipid metabolism in the body. Externally, the condition manifests itself as obesity. Increased body weight is not the only sign.
Note:
Despite the abundance of etiological causes, the basis is atherosclerosis. The mass fraction in the overall picture is 90-95%. Everything else is unimportant.
Diagnosis is also carried out with an eye to this condition, but if cholesterol deposition is excluded, further searches for atherosclerosis are indicated, which still require continued diagnosis. Perhaps we are talking about a system of factors.
Third group of reasons
Causes increased risks:
- Age 45+.
- Being male. According to various estimates, women suffer several times less often (m/f ratio is defined as 3-4:1). There is also a less aggressive course in the weaker sex.
- Smoking. Provokes persistent stenosis of arteries, including coronary ones. Over time, this reaction becomes stereotypical and does not require repeated stimulation. It is extremely difficult to cope with this option; even giving up a bad habit does not give full results.
- Caffeine abuse. All drinks are excluded: including tea, energy drinks.
- Excess alcohol. The amount of alcohol does not play a big role. It all depends on individual resistance and reaction to ethanol. For one a sip is enough, for another a bottle is not enough. Still others may drink alcohol their entire adult life and die from a cold. It’s not worth taking risks and experimenting on yourself. Alcohol has no place in the life of a healthy person.
- Burdened heredity. The genetic factor plays an important role.
- History of diabetes mellitus, hypertension, endocrine conditions.
- Obesity. Indirect risk factor.
All possible causes are taken into account in a comprehensive manner. Without this, there can be no talk of high-quality diagnosis, much less treatment.
Second FC of the disease and its features
Often, when a person is first diagnosed with coronary artery disease, angina pectoris has a second FC, because it is at this stage of the disease that the first signs of the disease begin to appear in a person.
The main parameters of decreased motor activity for angina pectoris FC 2 include the following factors:
- difficulty in climbing to the second floor and above;
- the maximum distance for walking does not exceed five hundred meters;
- stress, which is accompanied by overexcitation of an emotional and psychological nature.
When the patient begins to experience a load not exceeding the above, then symptoms appear.
Most often, the following symptoms appear with this disease:
- dyspnea;
- tachycardia;
- increased sweating;
- sudden jumps in blood pressure (blood pressure);
- interruptions in the heart;
- pain in the area of the cardiac projection or chest;
- fear of death.
The main symptom of IHD 2 FC is an attack of pain. The pain is most often sharp, burning, squeezing or stabbing in nature and lasts up to ten minutes.
The main location of pain is the heart area or the sternum. Often the pain can spread to the neck, left shoulder blade, lower jaw or left arm.
The main characteristic feature of this stage of the disease is the fact that it can be stopped quite easily by taking nitroglycerin and eliminating the factor that provoked the attack, for example, stress or physical fatigue.
Symptoms
Manifestations of FC 2 of exertional angina occur as a result of moderate physical and emotional activity and are quite pronounced.
If we translate abstract words into something concrete: it is impossible to climb to the 2-3 floor, sports are also no longer available. Even intensive walking is difficult.
The following manifestations occur:
- Chest pain of moderate intensity, not too pronounced, is the main characteristic symptom. It radiates to the shoulder blade and left arm, moving as if through the veins and reaching the hand. It does not intensify with movement or breathing, which distinguishes it from the discomfort caused by intercostal neuralgia. Treated with Nitroglycerin. Duration: 10-12 minutes, but no more than half an hour. Deviations towards intensification indicate a possible heart attack.
- Dyspnea. Increase in the number of movements per minute. In the second class of angina, it is already difficult not to notice it. Characterized by discomfort and dissatisfaction with inhalation. Accompanies moderate physical activity.
- Cyanosis of the nasolabial triangle, blue discoloration of the area around the mouth.
- Paleness of the skin.
- Panic attack. The patient becomes anxious and is in an inadequate state. Help Wanted.
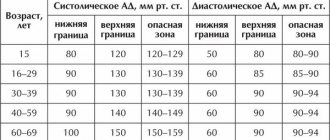
- Increase in blood pressure. Not always, but often. Within insignificant limits.
- Nausea, dizziness.
- Arrhythmias. By type of tachycardia, as a rule. The frequency of contractions remains normal, but the intensity of work is higher.
- Fainting is possible. Relatively rare. Indicate the involvement of cerebral structures in the pathological process.
At the end of the attack, the entire clinical picture disappears.
Attention:
If it lasts more than 30 minutes, there is a high risk of a heart attack. It is easy to confuse it with angina pectoris without experience. Mortality is many times higher. It is also possible to smoothly flow from one state to another.
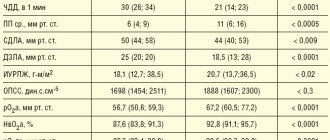
classification of heart failure in children
CLASSIFICATION OF HEART FAILURE IN CHILDREN.
Until now, the most convenient for determining the stage of CHF (CHF), taking into account right and left ventricular failure in children with clear clinical criteria, is the classification proposed by N.A. Belokon.
Isolated assessment of right and left ventricular heart failure is of particular importance in childhood, as it allows for a differentiated approach to the treatment of these patients.
When assessing the severity of CHF, 2 principles must be maintained: assessment of the stage (based on clinical manifestations) and the functional state of the patient.
Classification of heart failure in children according to N.A. Belokon (1987)
| stage | Left ventricular failure | Right ventricular failure |
| I | Heart failure is absent at rest and appears after exercise in the form of shortness of breath and tachycardia | |
| II A | The number of heart contractions is increased by 15-30% per minute. The number of respirations is increased by 30-50% | The liver protrudes 2-3 cm from under the edge of the costal arch |
| II B | The number of heart contractions is increased by 30-50% per minute. The number of respirations is increased by 50-70% Possible acrocyanosis, obsessive cough, moist fine rales | The liver protrudes 3-5 cm from under the edge of the costal arch; pastosity and swelling of the neck veins are possible |
| III | The number of heart contractions is increased by 50-60% per minute. The number of respirations is increased by 70-100% Clinical picture of pulmonary preedema | Hepatomegaly, edematous syndrome, hydropericardium, ascites |
The greatest difficulty in pediatric cardiology is determining the functional class of CHF, especially in children of early and preschool age. In Western studies, the Ross classification is used to determine the functional class of CHF in young children. The disadvantage of this classification is the assessment of hemodynamic overload only in the pulmonary circulation, without clear quantitative criteria.
of chronic heart failure according to Ross R. D. _ (1987)
| CLASS | INTERPRETATION |
| I | No symptoms |
| II | Slight tachypnea or sweating when feeding infants. Dyspnea during exertion in older children. |
| III | Severe tachypnea or sweating during feeding in infants. Extended feeding time, delay growth due to heart failure. Expressed dyspnea during exertion in older children. |
| IV | At rest, there are symptoms such as tachypnea, muscle retraction, “grunting,” and sweating. |
In school-age children and adolescents, the National Classification of CHF (2002), adopted by the All-Russian Scientific Society of Cardiologists (VNOK) and the Society of Heart Failure Specialists (OSHF), should be more widely used, which provides for the unification of the currently existing classification of stages of CHF (V.Kh. Vasilenko and N.D. Strazhesko) and FC (New York Heart Association (NYHA)) and determines the stages of the process and the functionality of the patient.
National classification of CHF (OSSN, 2002)
| Stages of CHF | Functional classes of CHF | ||
| I | The initial stage of heart disease (damage). Hemodynamics are not impaired. Hidden heart failure. | I FC | There are no restrictions on physical activity: habitual physical activity is not accompanied by rapid fatigue, shortness of breath or palpitations. The patient can tolerate increased stress, but it may be accompanied by shortness of breath and/or delayed recovery. |
| II A | Clinically pronounced stage of the disease. Hemodynamic disturbances in one of the blood circulation circles, expressed moderately. | II FC | Slight limitation of physical activity: no symptoms at rest, usual physical activity is accompanied by fatigue, shortness of breath or palpitations. |
| II B | Severe stage of heart disease (damage). Pronounced changes in hemodynamics in both circulation circles, moderately expressed. | III FC | A noticeable limitation of physical activity: there are no symptoms at rest, physical activity of less intensity compared to usual exercise is accompanied by - due to the appearance of symptoms. |
| III | The final stage of heart damage. Pronounced changes in hemodynamics and severe (irreversible) structural changes in target organs (heart, lungs, blood vessels, brain, kidneys). | IV | Inability to perform any exercise without discomfort; symptoms are present at rest and worsen with minimal physical activity. |
First aid for an attack
Since the origin of the negative sensation is not clear, you need to call an ambulance immediately after the pain begins. There is no need to be shy, life is much more valuable.
The following is the algorithm:
- Measure blood pressure and heart rate. If both indicators are above normal, this is typical for the clinical picture.
- Take a Nitroglycerin tablet to relieve pain. Intense tachycardia is eliminated with Anaprilin (1 tablet); it is also possible to use Captopril (1/4 tablet) if blood pressure reaches critical values (over 180 per 100 mm Hg). However, this is a last resort.
- Open a window or vent to ensure adequate ventilation of the room. On the street, try to go into the nearest building; you cannot be in the cold, as this aggravates the general condition of angina pectoris.
- Sit down and relax. It is not recommended to lie down; shortness of breath may increase. There is no need to panic.
- Unfasten the collar and remove body jewelry from the neck. This will prevent the progression of symptoms against the background of a reflex reaction.
Wait for the medical team to arrive and tell about your complaints. Further, the issue is resolved at the discretion of the paramedic.
Treatment
2 FC angina pectoris is eliminated by conservative and, in extreme cases, surgical methods. The classic ABCDE scheme is used. The points. The total duration is about 3-4 months.
Initial list of actions:
- Restoring the rheological properties of blood. Aspirin-Cardio and analogues.
- Elimination of arterial stenosis. Using Carvedilol and Nitroglycerin in combination.
- Fighting excess cholesterol. Statins are used (Atoris and analogues).
- Diet for angina pectoris 2 FC: a minimum of fats and easily digestible (fast) carbohydrates. A topic for a separate conversation.
- Taking cardioprotectors, drugs to restore local metabolism in the myocardium. Riboxin, Mildronate and others.
Surgical intervention is undertaken when conservative tactics are ineffective.
Bypass surgery, ballooning, stenting or prosthetics are performed. All methods, one way or another, are aimed at restoring the anatomical lumen of the coronary artery or replacing the affected area with an artificial one.
Lifestyle correction
In the second phase, a major role is given to the following points:
- Quitting smoking, alcohol, drugs.
- Normal sleep pattern (at least 8 hours).
- Mastering relaxation techniques, control over the emotional background. This is a big problem for temperamental people.
- Salt no more than 7 grams per day.
Diet correction
The diet for angina pectoris FC 2 involves changing the proportions of substances in favor of protein. Less carbohydrates and fats. Treatment table No. 10 is shown.
Permitted products can be combined in other ways. It is important to eat small meals (5-6 times a day), a sufficient amount of liquid, and coarse fiber.
Cooking methods: boiling, stewing, baking.