Cardiologist
Sokolov
Denis Vladimirovich
16 years of experience
Cardiologist of the first category, candidate of medical sciences, member of the Asute Cardiovascular Care Association (ASSA)
Make an appointment
Angina pectoris is a pathology that manifests itself in representatives of different age groups in the form of attacks of myocardial ischemia. Symptoms arise against the background of increased physical or emotional stress that the patient faces. People suffering from angina pectoris experience pain in the heart area and shortness of breath. Autonomic reactions develop as a result of exposure to unfavorable external factors on the body.
Reasons for the development of pathology
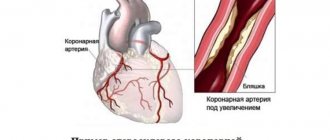
Often the symptoms of angina pectoris develop against the background of atherosclerosis of the coronary arteries. The lumen of the blood vessels narrows by 50-70%, which leads to the delivery of less oxygen to the heart muscle with constant consumption. Common causes of angina remain arterial hypertension, coronary spasm, aortic stenosis, and congenital anomalies of the coronary arteries. Pathology can become a complication in acute coronary thrombosis.
Risk factors include:
- systematic smoking;
- alcohol consumption;
- age over 55 years;
- obesity 3-4 degrees;
- early menopause;
- diabetes.
The risk group includes patients with pathologies of the cardiovascular system in a family history. Severe forms of anemia and hypoxia can complicate the course of the disease.
Doctor's advice
In addition to the generally accepted lifestyle interventions described above, I strongly encourage my patients to monitor their blood pressure and take appropriate medications regularly.
If a person suffers from diabetes, he should regularly check his blood glucose levels and periodically take a glycated hemoglobin test. This is important, since diabetes can worsen the course of angina several times and lead to complications.
Also, if you cannot eat fish often, you can take fish oil in the form of dietary supplements. They are available in any pharmacy. To argue for the benefits of fish oil, I would like to give the example of Japan, a country where heart disease rates are extremely low, and fish as a food product occupies the top positions.
Clinical case
I would like to provide an example from personal experience.
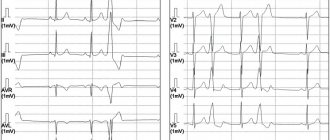
A 52-year-old man visited his local physician for an outpatient appointment with complaints of pressing pain in the heart area, which occurs when climbing the stairs to the 3rd floor and goes away a few minutes after resting. I began to notice the appearance of these pains about a month ago. Suffering from type 2 diabetes mellitus and hypertension. She takes Metformin 1000 mg 2 times a day and Lisinopril 10 mg 1 time a day. The therapist referred him to a cardiologist, who prescribed an ECG and VEM (veloergometry). At rest, when deciphering the ECG, there were no changes. When performing a VEM, an ECG revealed ST segment depression of 2 mm. The patient was sent to the cardiology hospital for further examination with a diagnosis of coronary artery disease, angina pectoris FC 2. Coronary angiography was performed, which revealed 70% stenosis of the right coronary artery. The damage to the remaining vessels was not critical, so the decision was made to install a stent. Drug therapy was also prescribed (Acetylsalicylic acid, Rosuvastatin, Bisoprolol). The patient noted a significant improvement in his condition in the form of cessation of pain attacks. Upon discharge, recommendations for lifestyle modifications were given.
In conclusion, I would like to note that angina pectoris is a serious disease that requires due attention from both the doctor and the patient. Ignoring attacks of pain can lead to an unfavorable prognosis in the form of myocardial infarction, disability and death. However, timely diagnosis and proper treatment can improve the quality and increase the life expectancy of a person.
Forms of pathology
Cardiologists distinguish three types of the disease: primary, stable and progressive. The first and second forms can transform into the third over time. A more extensive classification of angina pectoris is based on the patient's tolerance to physical activity. The intensity of the maximum permissible human activity allows us to distinguish four functional classes.
| Functional class (FC) | Description |
| I | Daily loads are tolerated without consequences. The attack develops against the background of unusual activity - running, climbing a large number of flights of stairs, lifting heavy objects. |
| II | Minor physical activity provokes the development of symptoms. Causes may include leisurely walking, climbing stairs to a height of more than one floor, emotional stress |
| III | The patient cannot tolerate minimal physical activity. An attack occurs when walking a distance of 50-100 meters. Climbing stairs is difficult |
| IV | Activity is significantly limited. Angina pectoris occurs when performing basic actions or while at rest |
Symptoms and signs
The main symptoms that determine exertional angina are attacks of heaviness in the chest, as well as burning or squeezing pain. These sensations can occur when a person is running, working out in the gym, or even just walking up the stairs.
The pain goes away if the load stops or the person takes Nitroglycerin in the form of a tablet/spray. This point is very important, it distinguishes more dangerous conditions - heart attack and unstable form of angina from this disease, since in them the pain is not relieved by Nitroglycerin.
Angina pain is characterized by specific irradiation - return to other parts of the body. This is mainly the lower jaw, neck, left arm and shoulder blade, and upper abdomen. Moreover, the place where the pain is applied is often felt much more strongly, and discomfort in the heart may go unnoticed. I often met patients who for a long time mistook attacks of angina for toothache and unsuccessfully underwent treatment for “pulpitis” or “periodontitis” at the dentist.
In addition to physical work, pain can “overtake” a person under other circumstances. Depending on the factor provoking a painful attack, the following clinical forms of angina pectoris are distinguished:
- Early morning - exacerbation appears at approximately 5-6 o'clock in the morning. Associated with increased blood viscosity and an increase in the amount of cortisol and adrenaline. They cause increased heart rate and hypertension.
- Angina after eating - a large meal redistributes blood flow in favor of the digestive organs. As a result, the oxygen supply to the heart deteriorates.
- Supine angina - when a person lies down, the volume load on his heart increases, which provokes increased work of the organ and, as a result, an increase in its need for oxygenation.
- Cold - at low ambient temperatures, the superficial blood vessels of the skin narrow, which forces the heart to work harder.
- Tobacco – components of cigarette smoke, including nicotine, increase heart rate, constrict blood vessels and thicken the blood.
- Angina after stress – stress stimulates the release of adrenaline and cortisol into the blood.
- Static – when a person bends over to, for example, put on shoes, pressure increases inside the chest. This, in turn, increases the volume load on the heart in the same way as supine angina occurs.
In some groups of patients, the clinical course of angina has its own characteristics. These include:
- elderly people - approximately 50% of people over 65 years of age experience not pain, but sudden difficulty breathing (shortness of breath);
- women - in females, due to the predominance of the emotional component during an attack, in addition to the pain associated with angina pectoris, neurotic pain develops as a result of vasospasm. I often have to accept female patients in whom it is difficult to determine the severity of angina pectoris only by symptoms and to distinguish it from other forms of ischemia;
- diabetics – due to the long course of diabetes mellitus, nerve endings are damaged, including those that conduct pain impulses. Therefore, I often meet such patients with hidden or asymptomatic angina.
Symptoms of angina pectoris
Patients experience pain of varying intensity: from mild discomfort behind the sternum to severe pain in the heart muscle. The duration of a typical attack is 3-5 minutes, there are pronounced onset and end phases. The intensity of symptoms decreases when the provoking factor is eliminated. The pain of angina pectoris is radiating and can affect the jaw, shoulder blade, arm or neck.
During an attack, the patient feels weak, shortness of breath appears, and tachycardia and arrhythmia develop. Representatives of the older age group may experience a sharp increase or decrease in blood pressure. In rare cases, an atypical attack develops, accompanied by abdominal pain, nausea and vomiting.
The frequency of manifestations of angina pectoris varies. Patients may experience up to five attacks per day or experience a sharp increase in symptoms every few months. If left untreated, angina at rest may develop against the background of exertional angina.
Are you experiencing symptoms of angina pectoris?
Only a doctor can accurately diagnose the disease. Don't delay your consultation - call
Publications in the media
Stable angina pectoris is one of the main manifestations of coronary artery disease. The main and most typical manifestation of angina pectoris is chest pain that occurs during physical activity, emotional stress, when going out into the cold, walking against the wind, or at rest after a heavy meal.
Statistical data. Every year, angina pectoris is recorded in 0.2–0.6% of the population, with its predominance in men aged 55–64 years (0.8% of cases). It occurs in 30,000–40,000 adults per 1 million population per year, and its prevalence depends on gender and age • In the age group of the population 45–54 years, angina pectoris is observed in 2–5% of men and 0.5–1% of women , in the group of 65-74 years - in 11-20% of men and 10-14% of women (due to a decrease in the protective effect of estrogens in menopause) • Before MI, angina pectoris is observed in 20% of patients, after MI - in 50% of patients.
Etiology • In most cases, angina pectoris occurs due to atherosclerosis of the coronary arteries. Although the correlation between the degree of atherosclerotic narrowing, its extent and the severity of the clinical manifestations of angina is insignificant, it is believed that the coronary arteries must be narrowed by at least 50–75% before a discrepancy between the myocardial oxygen demand and its delivery appears and the clinical picture of the disease arises • Other causes (relative coronary insufficiency) •• Aortic stenosis •• Hypertrophic cardiomyopathy •• Primary pulmonary arterial hypertension •• Severe arterial hypertension •• Aortic valve insufficiency.
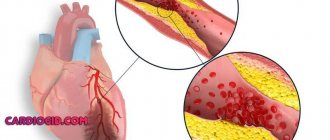
Pathogenesis • As a result of a discrepancy (imbalance) between the myocardial need for oxygen and its delivery through the coronary arteries due to atherosclerotic narrowing of the lumen of the coronary arteries, the following occur: •• Myocardial ischemia (clinically manifested by chest pain) •• Violations of the contractile function of the corresponding part of the heart muscle •• Changes biochemical and electrical processes in the heart muscle. In the absence of a sufficient amount of oxygen, cells switch to an anaerobic type of oxidation: glucose breaks down to lactate, intracellular pH decreases and energy reserves in cardiomyocytes are depleted • Subendocardial layers are primarily affected • The function of cardiomyocyte membranes is disrupted, which leads to a decrease in the intracellular concentration of potassium ions and an increase in intracellular concentration of sodium ions • Depending on the duration of myocardial ischemia, changes can be reversible or irreversible (myocardial necrosis, i.e. infarction) • Sequences of pathological changes during myocardial ischemia: impaired myocardial relaxation (impaired diastolic function) - impaired myocardial contraction (impaired systolic function ) - ECG changes - pain syndrome.
Canadian Cardiovascular Society Classification Pain does not occur when walking or climbing stairs. Seizures occur with severe, rapid or prolonged strain at work • Class II - “mild limitation of usual activities.” Pain occurs when walking or quickly climbing stairs, walking uphill, walking or climbing stairs after eating, in the cold, against the wind, during emotional stress, or within a few hours of waking up. Walking more than 100–200 m on level ground or climbing more than 1 flight of stairs at a normal pace and under normal conditions • Class III - “significant limitation of usual physical activity.” Walking on level ground or climbing one flight of stairs at a normal pace under normal conditions provokes an attack of angina pectoris • Class IV - “impossibility of any physical activity without discomfort.” Seizures may occur at rest
CLINICAL MANIFESTATIONS
Complaints. Characteristics of the pain syndrome • Localization of pain - retrosternal • Conditions for the occurrence of pain - physical activity, strong emotions, large meals, cold, walking against the wind, smoking. Young people often have the so-called phenomenon of “going through pain” (the “warm-up” phenomenon) - a decrease or disappearance of pain while increasing or maintaining the load (due to the opening of vascular collaterals) • Duration of pain - from 1 to 15 minutes, has an increasing character (“ crescendo"). If the pain continues for more than 15 minutes, the development of MI should be assumed • Conditions for stopping pain - stopping physical activity, taking nitroglycerin • The nature of pain during angina (squeezing, pressing, bursting, etc.), as well as the fear of death, are very subjective and not have serious diagnostic significance, since they largely depend on the physical and intellectual perception of the patient • Irradiation of pain - both to the left and right parts of the chest and neck. Classic irradiation - to the left arm, lower jaw.
Associated symptoms are nausea, vomiting, increased sweating, fatigue, shortness of breath, increased heart rate, increased (sometimes decreased) blood pressure.
Angina equivalents: shortness of breath (due to impaired diastolic relaxation) and severe fatigue during exercise (due to decreased cardiac output due to impaired systolic myocardial function with insufficient oxygen supply to skeletal muscles). In any case, symptoms should decrease when exposure to the provoking factor (physical activity, hypothermia, smoking) or nitroglycerin is stopped.
Physical data • During an attack of angina pectoris - pallor of the skin, immobility (patients “freeze” in one position, since any movement increases the pain), sweating, tachycardia (less often bradycardia), increased blood pressure (less often, its decrease) • Extrasystoles, “rhythm” can be heard gallop”, systolic murmur resulting from mitral valve insufficiency as a result of dysfunction of the papillary muscles • An ECG recorded during an attack of angina can detect changes in the terminal part of the ventricular complex (T wave and ST segment), as well as cardiac arrhythmias.
Laboratory data - supporting value; They can only determine the presence of dyslipidemia, identify concomitant diseases and a number of risk factors (DM), or exclude other causes of pain (inflammatory diseases, blood diseases, thyroid diseases).
Instrumental data
• ECG during an attack of angina: repolarization disturbances in the form of changes in T waves and ST segment displacement up (subendocardial ischemia) or down from the isoline (transmural ischemia) or heart rhythm disturbances.
• Daily ECG monitoring allows you to identify the presence of painful and non-painful episodes of myocardial ischemia in the usual conditions for patients, as well as possible heart rhythm disturbances throughout the day.
• Bicycle ergometry or treadmill (stress test with simultaneous recording of ECG and blood pressure). Sensitivity - 50-80%, specificity - 80-95%. The criterion for a positive stress test during bicycle ergometry is ECG changes in the form of horizontal ST segment depression of more than 1 mm lasting more than 0.08 s. In addition, stress tests can reveal signs associated with an unfavorable prognosis for patients with angina pectoris: •• typical pain syndrome •• ST segment depression of more than 2 mm •• persistence of ST segment depression for more than 6 minutes after cessation of exercise •• appearance of segment depression ST when the heart rate (HR) is less than 120 per minute •• the presence of ST depression in several leads, ST segment elevation in all leads, with the exception of aVR •• absence of a rise in blood pressure or its decrease in response to physical activity •• the occurrence of cardiac arrhythmias ( especially ventricular tachycardia).
• EchoCG at rest allows you to determine the contractility of the myocardium and conduct a differential diagnosis of pain syndrome (heart defects, pulmonary hypertension, cardiomyopathies, pericarditis, mitral valve prolapse, left ventricular hypertrophy in arterial hypertension).
• Stress echocardiography (echocardiography assessment of the mobility of left ventricular segments with an increase in heart rate as a result of dobutamine administration, transesophageal pacemaker or under the influence of physical activity) is a more accurate method for detecting coronary artery insufficiency. Changes in local myocardial contractility precede other manifestations of ischemia (ECG changes, pain). The sensitivity of the method is 65–90%, specificity is 90–95%. Unlike bicycle ergometry, stress echocardiography can detect coronary artery insufficiency when one vessel is affected. Indications for stress echocardiography are: •• atypical angina pectoris (the presence of angina equivalents or an unclear description of the pain syndrome by the patient) •• difficulty or impossibility of performing stress tests •• uninformativeness of bicycle ergometry in a typical clinical picture of angina pectoris •• absence of changes on the ECG during stress tests due to for blocks of the His bundle branches, signs of left ventricular hypertrophy, signs of Wolff–Parkinson–White syndrome in a typical clinical picture of angina pectoris •• positive stress test during bicycle ergometry in young women (since the likelihood of coronary artery disease is low).
• Coronary angiography is the “gold standard” in the diagnosis of coronary artery disease, since it allows us to identify the presence, location and degree of narrowing of the coronary arteries. Indications (recommendations of the European Society of Cardiology; 1997): •• exertional angina pectoris above functional class III in the absence of the effect of drug therapy •• exertional angina pectoris I–II functional class after MI •• exertional angina pectoris with His bundle branch block in combination with signs of ischemia according to data myocardial scintigraphy •• severe ventricular arrhythmias •• stable angina in patients undergoing vascular surgery (aorta, femoral, carotid arteries) •• myocardial revascularization (balloon dilatation, coronary artery bypass grafting) •• clarification of the diagnosis based on clinical or professional (for example, pilots) considerations.
• Myocardial scintigraphy is a method of visualizing the myocardium that allows identifying areas of ischemia. The method is very informative when it is impossible to evaluate the ECG due to blockades of the His bundle branches.
Diagnostics. In typical cases, stable angina pectoris is diagnosed based on a detailed history, a detailed physical examination of the patient, a resting ECG recording, and subsequent critical analysis of the data obtained. It is believed that these types of examinations (history, examination, auscultation, ECG) are sufficient to diagnose angina pectoris with its classic manifestation in 75% of cases. If there is any doubt about the diagnosis, 24-hour ECG monitoring, stress tests (veloergometry, stress echocardiography) are performed consistently, and if appropriate conditions are present, myocardial scintigraphy is performed. At the final stage of diagnosis, coronary angiography is necessary.
Differential diagnosis. It should be borne in mind that chest pain syndrome can be a manifestation of a number of diseases. We should not forget that there may be several causes of chest pain at the same time • Cardiovascular disease •• MI •• Angina pectoris •• Other causes ••• possibly of ischemic origin: aortic stenosis, aortic valve insufficiency, hypertrophic cardiomyopathy, arterial hypertension, pulmonary hypertension , severe anemia ••• non-ischemic: aortic dissection, pericarditis, mitral valve prolapse • Gastrointestinal diseases •• Esophageal diseases - esophageal spasm, esophageal reflux, esophageal rupture •• Stomach diseases - peptic ulcer • Diseases of the chest wall and spine •• Anterior thoracic syndrome walls •• Syndrome of the anterior scalene muscle •• Costal chondritis (Tietze syndrome) •• Damage to the ribs •• Herpes zoster • Lung diseases •• Pneumothorax •• Pneumonia involving the pleura •• PE with or without pulmonary infarction • Pleural diseases.
TREATMENT. The goals are to improve the prognosis (prevention of MI and sudden cardiac death) and reduce the severity (elimination) of symptoms of the disease. Non-drug, medicinal (drug) and surgical treatment methods are used.
• Non-drug treatment - impact on risk factors for coronary artery disease: dietary measures to reduce dyslipidemia and reduce body weight, smoking cessation, sufficient physical activity in the absence of contraindications. Normalization of blood pressure levels and correction of carbohydrate metabolism disorders are also necessary.
• Drug therapy - three main groups of drugs are used: nitrates, b-blockers and slow calcium channel blockers. Additionally, antiplatelet agents are prescribed.
Nitrates. When nitrates are administered, systemic venodilation occurs, leading to a decrease in blood flow to the heart (reduction in preload), a decrease in pressure in the chambers of the heart and a decrease in myocardial tension. Nitrates also cause a decrease in blood pressure, reduce resistance to blood flow and afterload. In addition, the expansion of large coronary arteries and an increase in collateral blood flow are important. This group of drugs is divided into short-acting nitrates (nitroglycerin) and long-acting nitrates (isosorbide dinitrate and isosorbide mononitrate).
• To relieve an attack of angina, nitroglycerin is used (tablet forms sublingually in a dose of 0.3–0.6 mg and aerosol forms - spray - are also used in a dose of 0.4 mg sublingually). Short-acting nitrates relieve pain in 1–5 minutes. Repeated doses of nitroglycerin to relieve an attack of angina can be used at 5-minute intervals. Nitroglycerin in tablets for sublingual use loses its activity after 2 months from the moment the tube is opened due to the volatility of nitroglycerin, so regular replacement of the drug is necessary.
• To prevent angina attacks that occur more often than once a week, long-acting nitrates are used (isosorbide dinitrate and isosorbide mononitrate) • Isosorbide dinitrate at a dose of 10-20 mg 2-4 times a day (sometimes up to 6) 30-40 minutes before expected physical activity. Retard forms of isosorbide dinitrate - at a dose of 40-120 mg 1-2 times / day before the expected physical activity • Isosorbide mononitrate at a dose of 10-40 mg 2-4 times / day, and retard forms - at a dose of 40-120 mg 1-2 r/day also 30–40 minutes before the expected physical activity.
• Tolerance to nitrates (loss of sensitivity, addiction). Regular daily use of nitrates for 1–2 weeks or more can lead to a decrease or disappearance of the antianginal effect •• The reason is a decrease in the formation of nitric oxide, acceleration of its inactivation due to increased activity of phosphodiesterases and increased formation of endothelin-1, which has a vasoconstrictor effect •• Prevention - asymmetric (eccentric) administration of nitrates (for example, 8 a.m. and 3 p.m. for isosorbide dinitrate or only 8 a.m. for isosorbide mononitrate). In this way, a nitrate-free period lasting more than 6–8 hours is provided to restore the sensitivity of the SMC of the vascular wall to the action of nitrates. As a rule, a nitrate-free period is recommended for patients during periods of minimal physical activity and a minimal number of painful attacks (individually in each case) •• Other methods of preventing nitrate tolerance include the use of sulfhydryl group donors (acetylcysteine, methionine), ACE inhibitors (captopril, etc. ), angiotensin II receptor blockers, diuretics, hydralazine, however, the incidence of tolerance to nitrates with their use decreases to a small extent.
Molsidomine is similar in action to nitrates (a nitrocontaining vasodilator). After absorption, molsidomine is converted into an active substance that is converted into nitric oxide, which ultimately leads to relaxation of vascular smooth muscle. Molsidomine is used in a dose of 2–4 mg 2–3 times/day or 8 mg 1–2 times/day (long-acting forms).
b-Adrenergic blockers. The antianginal effect is due to a decrease in myocardial oxygen demand due to a decrease in heart rate and a decrease in myocardial contractility. For the treatment of angina pectoris the following is used:
• non-selective b-adrenergic blockers (act on b1- and b2-adrenergic receptors) - for the treatment of angina, propranolol is used in a dose of 10-40 mg 4 times / day, nadolol in a dose of 20-160 mg 1 time / day;
• cardioselective b-adrenergic blockers (act primarily on b1-adrenergic receptors of the heart) - atenolol at a dose of 25–200 mg/day, metoprolol 25–200 mg/day (in 2 doses), betaxolol (10–20 mg/day), bisoprolol ( 5–20 mg/day).
• Recently, b-blockers have been used that cause peripheral vasodilation, such as carvedilol.
Slow calcium channel blockers. The antianginal effect consists of moderate vasodilation (including coronary arteries), reducing myocardial oxygen demand (in representatives of the verapamil and diltiazem subgroups). Used: verapamil - 80-120 mg 2-3 times / day, diltiazem - 30-90 mg 2-3 times / day.
Prevention of MI and sudden cardiac death
• Clinical studies have shown that the use of acetylsalicylic acid at a dose of 75–325 mg/day significantly reduces the risk of developing MI and sudden cardiac death. Patients with angina pectoris should be prescribed acetylsalicylic acid in the absence of contraindications - peptic ulcer, liver disease, increased bleeding, intolerance to the drug.
• The prognosis of patients with stable angina pectoris is also positively influenced by reducing the concentration of total cholesterol and LDL cholesterol using lipid-lowering drugs (simvastatin, pravastatin). Currently, optimal levels are considered to be no more than 5 mmol/l (190 mg%) for total cholesterol and no more than 3 mmol/l (115 mg%) for LDL cholesterol.
Surgery. When determining the tactics of surgical treatment of stable angina pectoris, it is necessary to take into account a number of factors: the number of affected coronary arteries, left ventricular ejection fraction, and the presence of concomitant diabetes. Thus, with one or two vessel lesions with a normal left ventricular ejection fraction, myocardial revascularization is usually started with percutaneous transluminal coronary angioplasty and stenting. In the presence of two or three-vessel disease and a decrease in the left ventricular ejection fraction of less than 45% or the presence of concomitant diabetes, it is more advisable to perform coronary artery bypass grafting (see also Atherosclerosis of the coronary arteries).
• Percutaneous angioplasty (balloon dilatation) - expansion of a section of the coronary artery narrowed by an atherosclerotic process with a miniature balloon under high pressure under visual control during angiography. The success of the procedure is achieved in 95% of cases. Complications are possible during angioplasty: •• mortality is 0.2% with single-vessel disease and 0.5% with multi-vessel disease, MI occurs in 1% of cases, the need for coronary artery bypass grafting appears in 1% of cases; •• late complications include restenosis (in 35–40% of patients within 6 months after dilatation), as well as the appearance of angina (in 25% of patients within 6–12 months).
• In parallel with the expansion of the lumen of the coronary artery, stenting has recently been used - implantation of stents (thin wire frames that prevent restenosis) at the site of narrowing.
• Coronary artery bypass grafting is the creation of an anastomosis between the aorta (or internal mammary artery) and the coronary artery below (distal) the site of narrowing to restore effective blood supply to the myocardium. A section of the saphenous vein of the thigh, the left and right internal mammary arteries, the right gastroepiploic artery, and the inferior epigastric artery are used as a graft. Indications for coronary artery bypass grafting (recommendations of the European Society of Cardiology; 1997) •• Left ventricular ejection fraction less than 30% •• Lesion of the trunk of the left coronary artery •• The only unaffected coronary artery •• Left ventricular dysfunction in combination with three-vessel disease, especially with damage to the anterior interventricular branches of the left coronary artery in the proximal part •• When performing coronary bypass surgery, complications are also possible - MI in 4-5% of cases (up to 10%). Mortality is 1% for single-vessel disease and 4–5% for multi-vessel disease. Late complications of coronary artery bypass grafting include restenosis (with the use of vein grafts in 10–20% of cases during the first year and 2% each year for 5–7 years). When arterial grafts are used, shunts remain open in 90% of patients for 10 years. Within 3 years, angina returns in 25% of patients.
The prognosis for stable angina pectoris with adequate treatment and monitoring of patients is relatively favorable: mortality is 2–3% per year, fatal MI develops in 2–3% of patients. A less favorable prognosis is for patients with a decrease in the ejection fraction of the left ventricle, a high functional class of stable angina pectoris, elderly patients, patients with multivessel disease of the coronary arteries, stenosis of the main trunk of the left coronary artery, proximal stenosis of the anterior interventricular branch of the left coronary artery.
Age characteristics • Children. The most common cause of symptoms of angina pectoris in children is hereditary dyslipidemia • Elderly - high sensitivity to the side effects of drugs (for example, severe depression when prescribing b-blockers) • Pregnancy - after clarifying the diagnosis, careful observation by an obstetrician and cardiologist is necessary, an increase in the need for oxygen during pregnancy increases the symptoms of angina pectoris.
Prevention • Stop smoking, diet low in cholesterol and fat, regularly perform a set of special exercises • Lipid-lowering drugs.
Synonyms • Angina pectoris • Angina pectoris • Heberden's disease.
ICD-10 • I20.8 Other forms of angina
Diagnosis of pathology
The patient is examined by a cardiologist. The most effective way to diagnose exertional angina is an ECG obtained during an attack. Ischemia is induced by stress testing. Conducting them in a clinical setting eliminates the possibility of complications developing in the patient. Holter monitoring can detect myocardial ischemia and heart rhythm disturbances.
EchoCG is aimed at assessing myocardial contractility. The use of this technique allows for differential diagnosis and exclusion of other pathologies of the cardiovascular system from the patient’s medical history. Laboratory tests - general and biochemical blood tests - provide an opportunity to detect signs of atherosclerotic damage to the patient’s blood vessels.
Diagnostics
In order to make a differential diagnosis, i.e. To distinguish ischemic pain from non-ischemic pain based on symptoms, I use specially developed criteria, including 3 main signs:
- classic attacks of angina pectoris,
- their appearance during physical work,
- weakening and disappearance after taking Nitroglycerin tablet/spray or stopping the load.
The presence of all three criteria is typical for typical angina, and two for atypical angina. If the patient has only one criterion, then the diagnosis is doubtful.
I also conduct a general examination of the patient, during which symptoms of heart failure can be identified:
- swelling of the legs,
- thickening of the fingertips,
- bluish lip color,
- swollen veins in the neck,
- enlarged and painful liver.
I especially often notice such signs in the elderly. In patients with heart defects, various sounds can be heard on auscultation. It is mandatory to measure blood pressure, since the vast majority of people with angina have hypertension.
To confirm or refute the diagnosis, I prescribe an additional examination, which includes:
- Blood analysis. Almost all people with coronary heart disease have elevated cholesterol levels. Therefore, I always prescribe a lipid profile (cholesterol fraction) determination. Also, following the protocol, you need to check the glucose concentration and do a general blood and urine test.
- Electrocardiography (ECG) is the main diagnostic method for suspected angina. The main symptom of the disease is a decrease (depression) in the ST segment. Sometimes a negative T wave is recorded. However, often these changes cannot be detected at rest, i.e. when there is no pain. Therefore, I prescribe additional ECG studies for my patients.
- Electrocardiography with stress. Of all such tests, I prefer bicycle ergometry (riding an exercise bike) and treadmill test (walking or running on a treadmill). If, after a certain time, symptoms of angina appear and the ECG shows typical signs (ST segment depression greater than 1 mm and a negative T wave), the test is considered positive. It is worth noting that such studies are not suitable for everyone. For example, I do not perform them on patients over 85 years of age and people with severe heart failure (III-IV functional class).
- Daily ECG monitoring. In cases where physical tests are not possible or the results obtained are questionable, it is advisable to conduct a Holter study. It is also a very good way to detect silent myocardial ischemia. Most often, I prescribe Holter ECG to patients with diabetes.
- Echocardiography (Echo-CG, ultrasound of the heart). The method allows you to check the ability of an organ to pump blood, assess the condition of the valves, the degree of wall thickening, and the presence of intracardiac blood clots.
- Transesophageal electrical stimulation of the heart (TEC) - the procedure is as follows. A flexible probe with an electrode is inserted through the patient's nose and installed in the esophagus in the projection closest to the heart. Then weak signals are sent, causing an attack of angina. At the same time, an ECG film is removed to record specific changes. I also perform this method on patients for whom physical tests are contraindicated.
- Myocardial scintigraphy - with this method I study the intensity of blood supply to the myocardium. For this, a radioactive drug is used (I mainly use thallium-201 and technetium-99-m), which is administered intravenously to the patient. Then he begins to perform moderate physical activity, after which an image is displayed on a special device. The degree of intensity of the glow is used to judge the blood circulation of different parts of the heart. I resort to myocardial scintigraphy if the patient has serious arrhythmias (bundle branch blocks, repeated ventricular extrasystoles), in which it is impossible to see specific changes on the cardiogram. This method is of little information for women, since breast tissue accumulates a significant part of the pharmaceutical drug.
- Coronary angiography is the gold standard for diagnosing coronary heart disease, allowing a reliable diagnosis. It can also be used to determine whether surgery is necessary.
Treatment
Therapy begins with the elimination of all provoking factors that can affect the condition of a person suffering from the pathology. The attacks are controlled by taking nitroglycerin. After making a diagnosis, the cardiologist can prescribe the patient long-acting nitrates, antiplatelet agents, calcium channel blockers and beta-blockers.
The persistence of symptoms during conservative treatment becomes a reason to refer a child or adult for surgery. During the intervention, surgeons perform stenting of the coronary arteries and perform endovascular angioplasty. Clinical recommendations provide for the possibility of coronary artery bypass grafting against the background of exertional angina. The effectiveness of surgical treatment is 90-95%.
Canadian classification
To determine the severity of symptoms of angina pectoris, the Canadian Society of Cardiology has developed a special classification in the form of a table, which includes the following functional classes of angina pectoris:
Functional class 1
When performing normal physical activity for a person, he feels good. Pain only appears during intense and prolonged work, such as weightlifting or long-distance running.
Functional class 2
Pain occurs even during normal walking, when a person walks more than 200 meters. Also, angina pectoris develops if the patient climbs stairs above the 2nd floor, goes outside in very cold weather, or overeats.
Functional class 3
The attack begins when walking from 100 to 200 meters, or when climbing to the 2nd floor.
Functional class 4
Doing any physical work causes pain. An attack can develop even in a completely calm state.
Questions and answers
Is there a set of preventive measures to prevent the development of angina pectoris?
Recommendations from cardiologists are addressed to people with a family history of coronary heart disease. Doctors insist that patients stop smoking and drinking alcohol. Fatty foods should be excluded from the diet. The dosage of medications prescribed for pathologies of the cardiovascular system should be observed.
Is surgery necessary for exertional angina?
The need for surgical intervention is determined by the clinical picture of the disease. For mild cases, patients are prescribed medication. The risk of complications or a severe form of pathology can become a decisive factor when a doctor makes a decision on surgical treatment.
Description of the disease
Angina pectoris, or angina pectoris, a chronic disease of the cardiovascular system, is characterized by chest pain during physical or gastronomic stress, in stressful conditions, and sudden hypothermia. This differs from another form - angina at rest. Pressing, squeezing or burning pain occurs due to the fact that the heart muscle cells are in a state of severe oxygen deficiency (ischemia).
Pain in angina pectoris quickly decreases and disappears almost immediately after a person puts a Nitroglycerin tablet under the tongue or stops doing any physical work. This is the main difference between “angina” pain and others.
Angina pectoris is considered the most common type of coronary heart disease and is classified under ICD code I20.8.
According to the World Health Organization (WHO), approximately 300,000,000 people worldwide suffer from angina. The average age of onset of the disease is 45-50 years. The male to female ratio is 2.5:1. However, this only applies to premenopausal women. After menopause, this figure is compared with men. There is a very specific explanation for this fact.
The main cause of angina pectoris is the deterioration of blood flow through the vessels that supply the heart muscle (coronary arteries) due to atherosclerosis. It occurs due to the fact that cholesterol, namely the so-called “bad” variety (low and very low density lipoproteins), is deposited in the walls of blood vessels. Female sex hormones (estrogens) have the ability to reduce the level of this fraction, which reduces the degree of formation of atherosclerotic plaque. And with the onset of menopause, the content of protective hormones in a woman’s blood sharply decreases, which increases cholesterol levels and, accordingly, the rate of development of pathology.
If angina pectoris is not recognized and treated in time, it can lead to myocardial infarction, the number one killer of all diseases.
Statistical data
Pathologies of the cardiovascular system remain the most common cause of death among Muscovites – 55% of cases in 2019. This figure is three times higher than the European average. The total number of Russian residents suffering from heart disease exceeds 16 million people. A quarter of them have congenital pathologies of the cardiovascular system. Prevention of attacks of myocardial ischemia remains one of the key tasks of cardiologists when monitoring patients at risk.
How does the disease develop?
It is at such moments that common signs of angina pectoris appear in women and men: you feel a lack of air, arrhythmia. At this time, chemical changes occur in the myocardium associated with metabolic disorders, a decrease in the synthesis of substances, and the accumulation of acids. The functions of the myocardium are gradually disrupted, and its metabolism changes.
What causes this disease? There are certain factors:
- high cholesterol levels;
- obesity when consuming excessive amounts of fats and carbohydrates;
- physical inactivity disrupts lipid volume;
- smoking causes oxygen starvation of cells and arterial spasm;
- arterial hypertension causes myocardial tension;
- anemia, intoxication contribute to oxygen starvation;
- diabetes mellitus increases the risk of ischemia;
- increased blood viscosity is a direct risk of blood clots;
- psycho-emotional stress (especially in women) worsens myocardial nutrition.