Reasons for the development of pathology
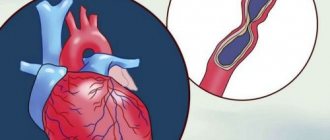
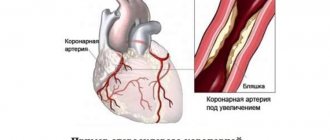
Symptoms of unstable angina develop against the background of a gradual narrowing of the lumen of the coronary arteries. This phenomenon causes necrosis of cardiomyocytes. Lipid deposits on the coronary vessels lead to the formation of atherosclerotic plaques. The patient suffers from decreased blood flow in the coronary arteries.
A significant amount of lipid deposits can cause blood clots. Damaged vessels become overly susceptible to substances released by platelets. This phenomenon provokes further narrowing of the arterial lumen.
Treatment of MVS
Treatment of MWS includes standard therapy for coronary artery disease: β-blockers, nitrates, calcium antagonists, statins, antiplatelet agents, second-line drugs (angiotensin-converting enzyme (ACE) inhibitors, nicorandil, ivabradine, ranolazine, trimetazidine), non-drug treatments (spinal cord stimulation, psychotherapy) [37].
Traditional antianginal drugs are prescribed in the first stages of treatment. Short-acting nitrates are recommended to relieve anginal attacks, but they often have no effect. Thus, only less than 50% of patients noted an improvement in their condition when using sublingual nitroglycerin. Conversely, nicorandil, which opens potassium ATP channels and has nitrate-like effects, has been reported to have a beneficial effect in MWS [38].
In patients with dominant symptoms of angina pectoris, therapy with β-blockers, which have been proven to eliminate the symptoms of angina pectoris, seems rational. These are the drugs of first choice, especially in patients with obvious signs of increased adrenergic activity (high heart rate at rest or during exercise) [39]. However, patients with microvascular or epicardial spasm should use caution when using β-blockers (especially those lacking vasodilatory properties) because these drugs may increase coronary vasoconstriction by masking α-adrenergic receptors in the coronary vessels [37].
Another drug that reduces myocardial oxygen demand due to its rate-lowering effects is ivabradine [40]. Calcium antagonists as first-line drugs are indicated in case of variability in the threshold of angina pectoris, especially in the angiospastic genesis of myocardial ischemia. Patients with clinical signs of MWS and lipid metabolism disorders are shown statins, which are known to have a positive effect on endothelial function. ACE inhibitors improve exercise tolerance and relieve angina symptoms [41]. The positive effect of ranolazine on endothelial function is known. In the work of E. Rayner-Hartley et al. [42] assessed the effect of ranolazine on the quality of life of patients with severe refractory angina caused by MVA. Patients received ranolazine at a dose of 1000 mg/day together with sulodexide for 4 weeks. The use of ranolazine improved the quality of life and reduced the number of visits to medical care. To correct endothelial dysfunction, trimetazidine is also used, which improves the metabolism of cardiomyocytes during myocardial ischemia. In the study by S.A. Boldueva et al. [43] showed the effectiveness of using trimetazidine in patients with MWS, in addition to standard antianginal therapy, with improvement in the clinical picture, quality of life, myocardial perfusion and endothelial function.
Unfortunately, traditional therapy for MWS is not always effective; the quality of life remains low due to pain, and patients are often hospitalized. Therefore, all patients with MWS require active correction of traditional risk factors, such as hypertension, diabetes mellitus, smoking, obesity, sedentary lifestyle, and hyperlipidemia.
Forms of pathology
The classification of unstable angina used by cardiologists takes into account the timing of the onset of primary symptoms of the disease.
| Form of angina | Description |
| First appeared | Pain syndrome develops against the background of many years of asymptomatic disease. Pain occurs during periods of physical activity of the patient. The frequency and intensity of attacks increase over time |
| Progressive | Over the course of a month, there is a sharp increase in the number of attacks. The pain syndrome develops at rest. The course of the disease is complicated by arrhythmia and functional disorder of the left ventricle |
| Spontaneous | It is characterized by single attacks that are not associated with the patient’s physical activity. The duration of the acute phase is at least 15 minutes. ECG reveals signs of ischemia, but cardiomyocyte necrosis does not develop |
| Variant | Unstable angina occurs when the patient is at rest. The attacks last more than 10 minutes. Cardialgia appears regularly, at the same time interval. Between attacks, the patient can perform any physical activity without consequences |
| Post-infarction | Develops several days after myocardial infarction. It is characterized by an extensive area of necrosis with an unfavorable course. Unstable angina of this form requires emergency care. |
Publications in the media
Unstable angina includes several clinical situations: • New-onset angina pectoris • Progressive angina pectoris (characterized by an increase in angina attacks and/or an increase in their duration and strength) • Angina pectoris that first appeared at rest.
Every patient with unstable angina must be hospitalized, because further development of the disease is unpredictable.
Statistical data. In the United States, approximately 750,000 patients are hospitalized each year for unstable angina.
Etiology - see Stable angina pectoris.
Pathogenesis . Rupture of the fibrous plaque capsule in the coronary artery, which provokes the formation of a blood clot with incomplete closure of the lumen of the vessel. The presence of a thrombus in the coronary artery prevents adequate blood supply to the myocardium, which leads to pain and full-blown unstable angina. The rupture of fibrous plaque is facilitated by the accumulation of large amounts of lipids and insufficient collagen content, inflammation and hemodynamic factors. Other mechanisms responsible for the development of unstable angina include: • intraplaque hemorrhage due to rupture of the vasa vasorum • increased platelet aggregation • decreased antithrombotic properties of the endothelium • local vasoconstriction due to the release of vasoactive agents such as serotonin, thromboxane A2, endothelin in response to disrupt the integrity of the fibrous plaque.
Classification. There is no generally accepted classification. In practice, the Braunwald classification (1989) is often used, dividing unstable angina into three classes (the higher the functional class, the greater the likelihood of complications).
• Class I - new angina or worsening of existing angina within a month.
• Class II - angina at rest during the previous month.
• Class III - angina at rest during the last 48 hours.
Clinical manifestations. Unstable angina pectoris is manifested by typical attacks, however, when collecting an anamnesis, characteristic signs of progression of angina pectoris can be identified.
• Over the past 1–2 months, the number, severity and duration of angina attacks (so-called crescendo angina) have increased.
• Attacks have never occurred before, appeared no more than 1 month ago (new-onset angina, de novo angina).
• Angina attacks began to appear at rest or at night.
• An important clinical sign is the absence or decrease in the effect of nitroglycerin, which previously stopped attacks of angina.
Diagnosis and differential diagnosis. The leading clinical manifestation of unstable angina is pain. The main condition with which unstable angina should be differentiated is MI, primarily small-focal (without a Q wave).
• ECG for unstable angina - changes in the final part of the ventricular complex (similar changes in MI with a Q wave) •• ST segment depression in 30% of patients •• T wave inversion - in 20% •• transient ST segment elevation - in 5%. A normal ECG does not exclude the presence of unstable angina. A resting ECG helps differentiate between large focal MI and unstable angina, since the former has an abnormal Q wave.
• Daily ECG monitoring allows you to identify changes characteristic of unstable angina, especially episodes of silent myocardial ischemia.
• Enzyme diagnostics. With MI, the following changes occur (unlike unstable angina): •• The MB fraction of CPK increases after 6–12 hours •• The myoglobin content increases after 3 hours •• Troponin T and troponin I react simultaneously with the MB fraction of CPK.
• EchoCG is not very informative (pathological movement of the walls of the left ventricle can be detected only during a painful episode).
• Coronary angiography is indicated when discussing the surgical treatment of unstable angina (percutaneous transluminal coronary angioplasty or coronary bypass surgery) or in patients with prognostically unfavorable signs of the disease. Angiographic examination can detect thrombi in the coronary arteries (in 40% of patients) and stenosis of the coronary arteries (in 40–60% of patients). At the same time, 15% of patients may have hemodynamically insignificant stenosis of the coronary arteries (narrowing of the artery lumen less than 60%), which confirms the greater importance of the nature of the fibrous plaque in the development of unstable angina than the severity of the stenosis.
TREATMENT
General tactics • Emergency hospitalization • Sharp limitation of physical activity • Relief of pain • Drugs to reduce myocardial oxygen demand • Anticoagulant and antiplatelet therapy.
Relief of pain syndrome. Administration of nitroglycerin solution at a dose of 5–10 mcg/min IV, increasing every 15 minutes by 5–10 mcg/min (up to 200 mcg/min) until pain disappears or a side effect appears in the form of arterial hypotension. After 24 hours, transfer to oral nitrates is carried out - isosorbide dinitrate or isosorbide mononitrate. Reduced myocardial oxygen demand
• b-Adrenergic blockers - propranolol 1-5 mg IV on the first day to all patients in the absence of contraindications. Subsequently, long-acting beta-blockers orally (for example, metoprolol retard, atenolol). Dosages are selected individually with the calculation of reducing heart rate to 55–60 per minute.
• If there are contraindications to the use of beta-blockers, slow calcium channel blockers (verapamil and diltiazem) are used. In the absence of sufficient antianginal effect from monotherapy, it is possible to use combination therapy - nitrates and beta-blockers, nitrates and slow calcium channel blockers.
Antiplatelet and anticoagulant therapy
• Acetylsalicylic acid at a dose of 75–325 mg/day (antiplatelet agent).
• If there are contraindications to taking acetylsalicylic acid, clopidogrel can be used at a dose of 75 mg 2 times a day.
• Anticoagulants •• Heparin - at an initial dose of 80 IU/kg (5000–7000 IU) intravenously, and then dropwise at 18 IU/kg/h (up to 1500 IU) for 1–2 days, followed by switching to subcutaneous administration at the same daily dose for several days. Heparin treatment is carried out under the control of PTT, which should be 2–2.5 times higher than the initial one (within 45–70 s) •• Low molecular weight heparins (calcium nadroparin, sodium enoxaparin) are prescribed 2 times/day subcutaneously.
Endovascular methods and coronary bypass surgery are performed according to general indications (see Atherosclerosis of the coronary arteries). Autovenous veins are preferred as shunts.
Flow. With adequate therapy, the condition of most patients (80%) improves within 24–48 hours. If there is no effect of drug treatment after 48 hours, surgical treatment methods (percutaneous transluminal coronary angioplasty with the installation of stents or coronary artery bypass grafting) should be considered. Indications for surgical intervention and the choice of method are similar to those for stable angina.
Forecast. Within 3 months, 10–20% of cases develop MI with a mortality rate of 4–10%. Sudden cardiac death is also possible. Prognostically unfavorable signs of unstable angina: • duration of pain more than 20 minutes • night pain • repeated pain with increasing duration • depression of the ST segment more than 1 mm • deep negative T waves • increased content of the MB-fraction of CPK • increased concentration of troponin T or troponin I • History of MI • History of coronary artery bypass grafting • Unstable hemodynamics (low blood pressure, labile pulse).
ICD-10 • I20.0 Unstable angina
Signs of pathology
The main symptom of unstable angina is intense pressing pain behind the sternum. The attack can last 10-15 minutes. The pain radiates to the left arm, shoulder, shoulder blade, neck and jaw. Taking nitroglycerin by the patient does not completely relieve symptoms. Over time, the frequency and intensity of attacks increase.
Manifestations of unstable angina develop against the background of:
- physical activity;
- stressful conditions;
- changeable weather;
- excessive food consumption.
Patients may experience interruptions in heart rate that occur with minimal physical activity (moving around the apartment, performing daily household chores). Later, shortness of breath joins the listed symptoms, and the person faces a lack of air.
Diagnostic procedures
The absence of specific symptoms does not allow the cardiologist to confirm the diagnosis during a physical examination. The doctor carries out differential diagnosis to exclude heart attack and non-ischemic heart pathologies from the patient’s history. Clinical guidelines suggest the following tests to confirm unstable angina:
- electrocardiography;
- general and biochemical blood tests;
- echocardiography;
- coronary angiography.
Cardiologists detect changes in the condition of the coronary arteries and decreased left ventricular function. Based on these data, the diagnosis is confirmed.
Introduction
Microvascular angina (MVA) is a disease of the cardiovascular system, accompanied by chest pain typical of angina and electrocardiographic changes characteristic of myocardial ischemia, without damage to the epicardial coronary arteries, according to angiography [1]. SWS is characterized by prolonged pain in the heart area not only during and after physical activity [2], but also at rest, often accompanied by a decrease in the pain threshold and a change in the emotional status of patients. Despite the fact that the prognosis for MVA is usually favorable, angina pectoris significantly worsens the quality of life of patients and poses a significant burden on the healthcare system. Diagnosis of MBC in real clinical practice is often based on history and clinical data, which leads to false-positive or false-negative results. With coronary angiography, only the epicardial arteries can be seen, and it is not possible to assess the state of the microvasculature [3]. Considering the widespread prevalence of MHS among patients with heart pain, an in-depth study of this pathology, its diagnosis and treatment is necessary.
Therapeutic measures
Conservative treatment involves prescribing several groups of drugs to the patient. Antianginal drugs relieve symptoms of angina pectoris. In acute attacks accompanied by intense pain, intravenous infusion of painkillers is performed.
Thrombolytics reduce the likelihood of blood clots. A similar goal is pursued when prescribing direct anticoagulants to a patient.
Lipid-lowering drugs remain an integral component in the drug treatment of unstable angina. They help normalize cholesterol levels in the patient’s blood. Constant use of such drugs reduces the likelihood of complications and recurrent attacks.
If conservative treatment is ineffective, the patient is prescribed surgery. The type of surgical intervention is determined by a cardiologist based on coronary angiography data. Imaging will allow us to understand the extent of damage to the coronary arteries. The most common methods of surgical treatment of angina remain coronary bypass surgery and coronary angioplasty.
Place of MVS in the structure of IHD
Cardiovascular diseases (CVD) still maintain a leading position in the structure of mortality around the world [4, 5]. Thus, according to Rosstat data for 2021, mortality from CVD was 633 cases per 100 thousand population. A year earlier, this figure was 622.1 cases per 100 thousand population. The annual mortality rate from coronary heart disease (CHD) among the Russian population is 27%. However, only 40–50% of patients with coronary artery disease know about their disease and receive comprehensive treatment. In more than half of hospitalized patients diagnosed with acute coronary syndrome, coronary angiography reveals unchanged coronary arteries, which indicates a different origin of anginal pain, not excluding AVS [6]. It is now widely accepted that obstructive disease of the epicardial arteries is not the only cause of myocardial ischemia [7, 8]. In a retrospective analysis of the NCDR Cath registry, only 37.6% of patients were diagnosed with obstructive epicardial artery disease, while 69% of patients were confirmed to have transient myocardial ischemia using noninvasive diagnostic tests [9]. It should be noted that chest pain with intact coronary arteries is not always a consequence of MVA, therefore, diagnostics require the use of high-resolution optical systems.