Home » Department of Vascular Surgery » Diseases » Vascular insufficiency
Vascular insufficiency is a pathological condition characterized by a decrease in the volume of blood circulating in the vessels. As a result of a decrease in blood flow speed, the transport of oxygen and nutrients across cell membranes is disrupted. Hypoxia develops and the functioning of cells and tissues is disrupted.
Causes of the disease
As a rule, cardiovascular failure occurs in patients who suffer from coronary heart disease and have suffered a myocardial infarction.
The following can also lead to the development of pathology:
- rheumatic heart defects;
- dilated cardiomyopathy;
- hypertonic disease;
- diabetes mellitus in combination with arterial hypertension.
Factors that provoke cardiovascular failure are:
- arrhythmias;
- pneumonia;
- anemia;
- hyperthyroidism;
- intake of cardiotoxic substances;
- alcoholism;
- excess body weight;
- rheumatism, etc.
Therapeutic measures
Assistance for vascular insufficiency of any type should be provided to the patient immediately:
- the patient is placed in a horizontal position so that his limbs are slightly elevated;
- clothing that can compress the chest and abdomen is either removed altogether or unbuttoned;
- moisten a cotton swab with ammonia and wave it a little near the victim’s nose.
Treatment of vascular insufficiency involves the administration of the following synthetic medications:
- orciprenaline sulfate;
- sodium benzoate;
- mesatone;
- caffeine;
- ascorbic acid;
- glucose;
- strychnine.
Classification
Acute failure.
The development of this pathology occurs according to:
- Left type. In this case, acute left ventricular or left atrial failure occurs.
- Right type. In this case, right ventricular failure occurs.
Acute failure goes through 3 stages of development:
- Initial. It is characterized by signs of circulatory failure. They appear only during physical activity. Patients complain of shortness of breath, fatigue and palpitations.
- Expressed. It is characterized by prolonged circulatory failure and a number of hemodynamic disorders. Symptoms of the pathology also appear at rest. The patient's ability to work is limited.
- Dystrophic (final). It is characterized by persistent circulatory failure, disturbances in the structure of organs such as the kidneys, lungs and liver. Patients also complain of general exhaustion.
Cerebrovascular insufficiency: clinical picture, diagnosis and therapy
Stroke and chronic forms of cerebrovascular insufficiency represent one of the most pressing problems of modern neurology. According to epidemiological data, the incidence of stroke in the world is 150 cases per 100 thousand population per year. Chronic insufficiency of blood supply to the brain is also very widespread.
In the domestic literature, the term “dyscirculatory encephalopathy” (DE) is usually used to denote the clinical syndrome of brain damage resulting from insufficient blood supply to the brain. According to the classification of vascular diseases of the brain proposed by E.V. Schmidt (1985), dyscirculatory encephalopathy refers to chronic disorders of cerebral circulation.
Vascular diseases of the brain (E.V. Schmidt et al., 1985)
- Acute cerebrovascular accidents
*Stroke– Ischemic stroke (thrombotic, embolic, hemodynamic, lacunar)
– Hemorrhagic stroke (parenchymal hemorrhage, subarachnoid hemorrhage)
*Transient cerebrovascular accidents
– Transient ischemic attacks
– Hypertensive cerebral crises
- Chronic cerebrovascular accidents
*Initial manifestations of insufficient blood supply to the brain*Encephalopathy
However, as modern research shows, various cardiovascular diseases, as a rule, lead simultaneously to chronic cerebral ischemia and repeated acute cerebrovascular accidents. Therefore, it would be more correct to define discirculatory encephalopathy as a syndrome of chronic progressive brain damage, which is based on repeated strokes and/or chronic insufficiency of blood supply to the brain (N. N. Yakhno, I. V. Damulin, 2001).
Etiology and pathogenesis of DE
The most common causes of impaired blood supply to the brain are atherosclerosis of the main arteries of the head, heart disease with a high risk of thromboembolism in the brain, and hypertension. Less commonly, cerebrovascular accidents develop as a result of inflammatory changes in blood vessels (vasculitis), disorders of the blood coagulation system, abnormalities in vascular development, etc. In the vast majority of cases, cerebral vascular insufficiency develops in elderly people suffering from the above cardiovascular diseases.
As follows from the definition of DE, 2 main pathogenetic mechanisms play a role in the formation of this syndrome: stroke and chronic cerebral ischemia. Ischemic strokes of the brain develop as a result of thrombosis of cerebral arteries, thromboembolism in the brain, arteriolosclerosis, rheological and hemodynamic disorders.
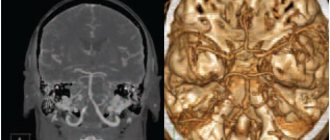
Chronic cerebral ischemia is based on structural changes in the vascular wall, which arise as a consequence of prolonged arterial hypertension or an atherosclerotic process. It has been established that lipohyalinosis of small-caliber vessels penetrating the brain substance can lead to chronic ischemia of the deep white matter. A reflection of this process are changes in the white matter (leukoaraiosis), which are defined as focal or diffuse changes in signal intensity from deep cerebral structures on T2-weighted images of magnetic resonance imaging of the brain. These abnormalities are considered to be typical neuroimaging symptoms that develop in patients with long-term uncontrolled arterial hypertension.
Clinical manifestations of DE
The clinical picture of DE is highly variable. As mentioned above, most patients with chronic vascular diseases of the brain have a history of strokes, often repeated. The localization of strokes undoubtedly largely determines the characteristics of the clinic. However, in the overwhelming majority of cases with cerebrovascular pathology, along with the consequences of strokes, there are also neurological, emotional and cognitive symptoms of dysfunction of the frontal lobes of the brain. This symptomatology develops as a result of disruption of connections between the frontal cortex and the subcortical basal ganglia (the “disconnection” phenomenon). The reason for the “disconnection” lies in diffuse changes in the white matter of the brain, which, as mentioned above, are a consequence of the pathology of small-caliber cerebral vessels.
Depending on the severity of the disorders, it is customary to distinguish 3 stages of dyscirculatory encephalopathy. The first stage is characterized mainly by subjective neurological symptoms. Patients complain of headache, dizziness, heaviness or noise in the head, sleep disorders, increased fatigue during physical and mental stress. These symptoms are based on a mild to moderate decrease in mood associated with dysfunction of the frontal lobes of the brain. Objectively, mild impairments of memory and attention, as well as possibly other cognitive functions, are detected. There may be an asymmetrical increase in tendon reflexes, uncertainty when performing coordination tests, and slight changes in gait. Instrumental research methods that make it possible to detect the pathology of cerebral vessels are important in the diagnosis of cerebral vascular insufficiency at this stage of the pathological process.
The second stage of discirculatory encephalopathy is spoken of in cases where neurological or mental disorders form a clinically defined syndrome. For example, we may be talking about mild cognitive impairment syndrome. This diagnosis is legitimate in cases where impairments in memory and other cognitive functions clearly go beyond the age norm, but do not reach the severity of dementia. At the second stage of DE, neurological disorders such as pseudobulbar syndrome, central tetraparesis, usually asymmetrical, extrapyramidal disorders in the form of hypokinesia, mild or moderate increase in muscle tone of the plastic type, ataxic syndrome, neurological disorders of urination, etc. can also develop.
At the third stage of dyscirculatory encephalopathy, a combination of several of the above neurological syndromes is noted and, as a rule, vascular dementia is present. Vascular dementia is one of the most severe complications that develops with the unfavorable course of cerebrovascular insufficiency. According to statistics, vascular etiology underlies at least 10–15% of dementia in old age.
Vascular dementia, like DE in general, is a pathogenetically heterogeneous condition. Vascular dementia is possible after a single stroke in a strategic area of the brain for cognitive activity. For example, dementia can develop acutely as a result of a heart attack or hemorrhage in the thalamus. However, much more often vascular dementia is caused by repeated strokes (so-called multi-infarct dementia). Another pathogenetic mechanism of vascular dementia is chronic cerebral ischemia, reflected by changes in the white matter of the brain. Finally, in addition to cerebral ischemia and hypoxia, secondary neurodegenerative changes play an important role in the pathogenesis of dementia in cerebrovascular insufficiency, at least in some patients with DE. Modern research has convincingly proven that insufficient blood supply to the brain is a significant risk factor for the development of degenerative diseases of the central nervous system, in particular Alzheimer's disease. The addition of secondary neurodegenerative changes undoubtedly aggravates and modifies cognitive disorders in cerebrovascular insufficiency. In such cases, the diagnosis of mixed (vascular-degenerative) dementia is legitimate.
Clinical manifestations of vascular dementia in each specific case depend on the pathogenetic mechanisms determining the disease. In post-stroke and multi-infarction dementia, clinical features depend on the location of the strokes. Changes in the white matter of the deep lobes of the brain as a result of chronic ischemia lead to cognitive impairment of the “frontal” type. These disorders are characterized by emotional disorders in the form of decreased mood, depression or apathy, and loss of interest in the environment. Emotional lability, which is a rapid, sometimes causeless change of mood, tearfulness or increased irritability, is also very characteristic. In the cognitive sphere, memory and attention impairments, slowness of thinking, decreased intellectual flexibility, and difficulties associated with switching from one type of activity to another are determined. The behavior of patients changes: the ability for self-criticism and the sense of distance are reduced, increased impulsiveness and distractibility are noted, symptoms such as disregard for socially accepted rules of behavior, asociality, foolishness, flat and inappropriate humor, etc. may be present.
The presence of secondary neurodegenerative changes in vascular dementia is manifested primarily by progressive memory impairment. At the same time, to a greater extent, the patient forgets what happened recently, while memories of distant events are retained for quite a long time. The neurodegenerative process is also characterized by disturbances in spatial orientation and speech.
Diagnosis of dyscirculatory encephalopathy
To diagnose dyscirculatory encephalopathy syndrome, it is necessary to carefully study the medical history, assess the neurological status, and use neuropsychological and instrumental research methods. It is important to emphasize that the presence of cardiovascular diseases in an elderly person does not in itself serve as evidence of the presence of cerebral vascular insufficiency. A necessary condition for correct diagnosis is to obtain convincing evidence of a cause-and-effect relationship between neurological and cognitive symptoms and cerebrovascular pathology, which is reflected in the currently accepted diagnostic criteria for DE.
Diagnostic criteria for DE (N. N. Yakhno, I. V. Damulin, 2001)
- Presence of signs (clinical, anamnestic, instrumental) of brain damage.
- Presence of signs of acute or chronic cerebral dyscirculation (clinical, anamnestic, instrumental).
- The presence of a cause-and-effect relationship between hemodynamic disorders and the development of clinical, neuropsychological, and psychiatric symptoms.
- Clinical and paraclinical signs of progression of cerebrovascular insufficiency.
Evidence of a vascular etiology for symptoms would include the presence of focal neurological symptoms, a history of stroke, characteristic neuroimaging changes such as post-ischemic cysts or marked white matter changes.
Treatment of cerebrovascular insufficiency
Cerebrovascular insufficiency is a complication of various cardiovascular diseases. Therefore, etiotropic therapy for DE should be, first of all, aimed at the underlying pathological processes of cerebrovascular insufficiency, such as arterial hypertension, atherosclerosis of the main arteries of the head, heart disease, etc.
Antihypertensive therapy is an essential factor in the secondary prevention of the increase in mental and motor symptoms of cerebrovascular insufficiency. To date, however, the question of what blood pressure levels should be achieved in the treatment of hypertension has not been resolved. Most neurologists believe that complete normalization of blood pressure in elderly patients with a long history of hypertension, while reducing the risk of acute vascular episodes, can simultaneously contribute to the aggravation of chronic cerebral ischemia and an increase in the severity of cognitive dysfunction of the “frontal” type.
The presence of hemodynamically significant atherosclerosis of the main arteries of the head requires the prescription of antiplatelet agents. Drugs with proven antiplatelet activity include acetylsalicylic acid at doses of 75-300 mg per day and clopidogrel (Plavix) at a dose of 75 mg per day. The study showed that the use of these drugs reduces the risk of ischemic events (myocardial infarction, ischemic stroke, peripheral thrombosis) by 20-25%. The possibility of simultaneous use of these drugs has now been proven. Medicines with antiplatelet properties also include dipyridamole (chimes), which is used in doses of 25 mg three times a day. Monotherapy with this drug does not provide prevention of cerebral or other ischemia, however, with combined use, dipyridamole significantly increases the preventive effect of acetylsalicylic acid. In addition to the prescription of antiplatelet agents, the presence of atherosclerotic stenosis of the main arteries of the head requires referral of the patient for consultation with a vascular surgeon to decide on the advisability of surgical intervention.
If there is a high risk of thromboembolism in the brain, for example in cases of atrial fibrillation and valvular disease, antiplatelet agents may be ineffective. The listed conditions serve as an indication for the prescription of indirect anticoagulants. The drug of choice is warfarin. Therapy with indirect anticoagulants should be carried out under strict monitoring of coagulogram parameters.
The presence of hyperlipidemia that cannot be corrected by diet requires the prescription of lipid-lowering drugs. The most promising drugs are from the statin group (Zocor, Simvor, Simgal, Rovacor, Medostatin, Mevacor, etc.). According to some data, therapy with these drugs not only normalizes lipid metabolism, but also may have a preventive effect against the development of a secondary neurodegenerative process against the background of cerebrovascular insufficiency.
An important pathogenetic event is also the impact on other known risk factors for cerebral ischemia. These include smoking, diabetes, obesity, physical inactivity, etc.
In the presence of cerebrovascular insufficiency, the prescription of drugs that act primarily on the microvasculature is pathogenetically justified. These include:
- phosphodiesterase inhibitors: aminophylline, pentoxifylline, vinpocetine, tanakan, etc. The vasodilating effect of these drugs is associated with an increase in the cAMP content in the smooth muscle cells of the vascular wall, which leads to their relaxation and an increase in the lumen of blood vessels;
- calcium channel blockers: cinnarizine, flunarizine, nimodipine. They have a vasodilating effect due to a decrease in the intracellular calcium content in the smooth muscle cells of the vascular wall. Clinical experience suggests that calcium channel blockers, such as cinnarizine and flunarizine, may be more effective for vertebrobasilar circulatory failure; this is manifested by symptoms such as dizziness and unsteadiness when walking;
- α2-adrenergic receptor blockers: nicergoline. This drug eliminates the vasoconstrictor effect of the mediators of the sympathetic nervous system: adrenaline and norepinephrine.
Vasoactive drugs are among the most commonly prescribed drugs in neurological practice. In addition to the vasodilatory effect, many of them also have positive metabolic effects, which allows these drugs to be used as symptomatic nootropic therapy. Experimental data indicate that the vasoactive drug tanakan has the ability to deactivate free radicals, thereby reducing the processes of lipid peroxidation. The antioxidant properties of this drug also allow it to be used for secondary prevention of the increase in memory impairment and other cognitive functions in cases of secondary neurodegenerative changes.
In domestic practice, vasoactive drugs are usually prescribed in courses of 2-3 months, 1-2 times a year.
Metabolic therapy is widely used for cerebrovascular insufficiency, the purpose of which is to stimulate the reparative processes of the brain associated with neuronal plasticity. In addition, metabolic drugs have a symptomatic nootropic effect.
Piracetam was the first drug specifically synthesized to affect memory and other higher brain functions. In recent years, however, it has been possible to prove that in previously taken doses this drug has a relatively small clinical effect. Therefore, the use of piracetam in dosages of at least 4–12 g/day is currently recommended. Intravenous administration of this drug in saline solution is more appropriate: 20–60 ml of piracetam per 200 ml of saline solution intravenously, 10–20 infusions per course.
The peptidergic drug Cerebrolysin is no less successfully used for cerebrovascular insufficiency, as well as vascular and degenerative dementia. As in the case of piracetam, views on the dosage regimen of this drug have changed significantly in recent years. According to modern concepts, the clinical effect occurs in the case of intravenous administration of Cerebrolysin in doses of 30–60 ml intravenously in 200 ml of saline, 10–20 infusions per course.
Peptidergic drugs that have a beneficial effect on cerebral metabolism also include Actovegin. Actovegin is used in the form of intravenous infusions (250–500 ml per infusion, 10–20 infusions per course), or in the form of intravenous or intramuscular injections of 2–5 ml 10–20 injections, or orally 200–400 mg 3 times a day within 2-3 months.
Like vasoactive drugs, metabolic therapy is carried out in courses 1-2 times a year. Pathogenetically justified and appropriate is the combined implementation of vasoactive and metabolic therapy. Currently, the doctor has several combined dosage forms at his disposal, which include active substances with vasoactive and metabolic effects. These drugs include instenon, vinpotropil, fezam and some others.
The development of vascular dementia syndrome requires more intensive nootropic therapy. Among modern nootropic drugs, acetylcholinesterase inhibitors have the most powerful clinical effect on cognitive functions. Initially, drugs in this group were used in the treatment of mild and moderate dementia due to Alzheimer's disease. Today it has been proven that acetylcholinergic deficiency plays an important pathogenetic role not only in this disease, but also in vascular and mixed dementia. Therefore, cognitive disorders of vascular and mixed etiology are increasingly appearing among the indications for the prescription of acetylcholinesterase inhibitors.
In Russia, two drugs from the group of latest generation acetylcholinesterase inhibitors are currently available: Exelon and Reminyl. Exelon is prescribed at an initial dose of 1.5 mg 2 times a day, then the single dose is increased by 1.5 mg every 2 weeks. up to 6.0 mg 2 times daily or until side effects occur. Common side effects when using Exelon are nausea and vomiting. These phenomena do not pose a threat to the life or health of the patient, but may interfere with the achievement of a therapeutic effect. Reminyl is prescribed at 4 mg 2 times a day for the first 4 weeks, and then 8 mg 2 times a day. This drug is less likely to cause adverse events.
First generation acetylcholinesterase inhibitors include neuromidin. According to some data, this drug has a positive nootropic effect in both vascular and primary degenerative and mixed dementia. It is prescribed in a dose of 20–40 mg 2 times a day.
Therapy with acetylcholinesterase inhibitors should be carried out continuously. In this case, it is necessary to monitor the level of liver enzymes in the blood once every 3–6 months.
The use of akatinol memantine is also pathogenetically justified for vascular dementia. This drug is an inhibitor of NMDA glutamate receptors. Chronic intake of akatinol memantine has a symptomatic nootropic effect, and may also slow down the rate of increase in cognitive disorders. The effect of the drug was manifested in both mild and moderate and severe dementia. It should be noted that akatinol memantine is the only drug effective at the stage of severe dementia. It is prescribed during the first week 5 mg 1 time per day, during the second week - 5 mg 2 times a day, starting from the third week and then continuously - 10 mg 2 times a day.
In conclusion, it should be emphasized that a comprehensive assessment of the state of the cardiovascular system of patients with cerebrovascular insufficiency, as well as the impact on both the cause of the disorders and the main symptoms of DE, undoubtedly contribute to improving the quality of life of patients and preventing severe complications of cerebrovascular insufficiency, such as , such as vascular dementia and movement disorders.
V.V. Zakharov, Doctor of Medical Sciences Clinic of Nervous Diseases named after. A. Ya. Kozhevnikova, Moscow
Symptoms
Acute failure is characterized by:
- attacks of suffocation (mainly at night);
- cough with difficult to clear sputum;
- cold sweat;
- feeling of lack of air;
- severe weakness.
Upon examination, the specialist discovers:
- pale skin;
- acrocyanosis;
- severe shortness of breath;
- weak arrhythmic pulse;
- dull heart sounds;
- reduced blood pressure;
- hard breathing with occasional wheezing.
Chronic insufficiency is characterized by:
- nocturnal attacks of suffocation;
- dyspnea;
- dry cough;
- palpitations;
- increased fatigue.
The condition is dangerous because it can lead to a number of complications.
The most common ones are the following:
- Heart rhythm disturbances. They can be fatal.
- Infectious lesions and bronchopneumonia. Such pathologies arise due to stagnation of fluid and blood, as well as low respiratory activity.
- Pulmonary hemorrhages.
- Liver cell failure. This pathology also develops with venous stagnation. It is also provoked by deterioration of perfusion (tissue nutrition).
- Cachexia of the heart. This pathology is a common complication in the terminal stages of insufficiency. It is caused by metabolic disorders (poor absorption of fats).
- Pulmonary infarctions.
- Emboli.
- Chronic renal failure.
Symptoms of vascular insufficiency
Characteristic manifestations of acute vascular insufficiency are shock, fainting or collapse. The difference between them consists mainly in the absence or presence of a disorder of consciousness, however, each condition also has its own characteristic symptoms:
- Fainting is characterized by the suddenness of its appearance, a sharp deterioration in general health, and autonomic disorders. Usually a person feels increasing weakness, discomfort, nausea, and then loses consciousness for a while. As the pathological condition develops, pale skin, ringing sounds in the ears, and a feeling as if the earth is disappearing from under one’s feet are observed.
- Collapse is associated with a decrease in the volume of circulating blood and a deterioration in vascular tone. Symptoms of vascular insufficiency in such a situation manifest themselves in the form of weakened vision and a feeling of thirst. The person remains conscious, but his skin turns pale, his face takes on a sallow color, and his fingers, lips and the tip of his nose become bluish. The pathology is characterized by indifference to everything around, a feeling of melancholy and shallow breathing.
- Shock is a complex pathological process caused by a sharp decrease in blood flow against the background of extreme influences (electric shock, burns, severe injuries, etc.). The clinical picture of shock is almost similar to collapse, but it goes through several stages, and at the last (terminal) the actions of doctors may not produce results.
Diagnostics
Insufficiency is a secondary syndrome that develops in a number of known pathologies, so diagnosis should be carried out even in the absence of pronounced manifestations.
The examination includes:
- Collection of clinical history. The specialist pays attention to the patient's fatigue. This symptom is often the earliest. The cardiologist also clarifies whether the patient has had a myocardial infarction, whether he suffers from hypertension and other diseases. Particular attention is paid to inspection. The specialist listens to heart sounds and examines the legs (for swelling).
- Laboratory research. When the first signs of pathology are detected during examination, specialists determine the gas and electrolyte composition of the blood, as well as the level of acid-base balance. The parameters of creatinine, urea, and cardiac-specific enzymes are studied. The parameters of protein-carbohydrate metabolism are also studied.
- ECG. This study makes it possible to detect myocardial hypertrophy and circulatory failure. An ECG can also detect arrhythmia.
- Load tests. Such studies are carried out to assess the reserve capacity of the heart.
- EchoCG. This study allows you to evaluate the pumping function of the myocardium, detect congenital and acquired defects, arterial hypertension and other pathologies.
- X-ray of the lungs and chest organs. Such a study makes it possible to detect stagnant processes in the pulmonary circulation.
- Radioisotope ventriculography. This study is carried out to assess the contractility of the ventricles and determine their volumetric capacity.
In severe forms of pathology, the condition of the internal organs must be assessed. Patients are referred for ultrasound of internal organs (pancreas, liver, spleen, etc.). Additionally, you can be observed by an andrologist, obstetrician-gynecologist, or other specialist. Everyone will prescribe an adequate diagnosis in accordance with their profile. This will eliminate the presence of third-party pathologies or confirm them and promptly begin adequate therapy.
Symptoms of heart failure
Common signs of heart failure of any type:
- difficulty breathing, shortness of breath, suffocation;
- increased fatigue, decreased physical activity;
- swelling in heart failure (including internal organs);
- weight gain due to fluid retention.
As for other symptoms of heart failure, manifestations may vary depending on which ventricle of the heart the pathology develops in.
For left ventricular acute heart failure (due to stagnation of blood in the pulmonary circulation) the following are typical:
- Cardiac asthma - an attack of suffocation occurs at night or after physical effort. There is a feeling of acute lack of air, shortness of breath quickly increases to suffocation. The patient breathes through the mouth to ensure greater air flow.
- Orthopnea - the patient is forced to take a sitting position, which improves the outflow of blood from the vessels of the lungs.
- The cough is dry at first, then with the release of pinkish sputum and foam.
- Pulmonary edema - moist wheezing, bubbling difficulty breathing, foam at the mouth.
Characteristic signs of right ventricular acute heart failure are caused by stagnation of blood in the veins of the systemic circulation:
- Swelling of the neck veins (associated with difficulty in blood flow to the heart, worsens with inhalation);
- rapid heartbeat (accompanied by shortness of breath);
- swelling (due to slow blood circulation, fluid retention occurs);
- lowering blood pressure.
First aid for heart failure (HF)
It is necessary to call an ambulance, sit the patient down, making sure to lower his legs. Provide fresh air flow. If the person is conscious, talk to him and try to calm him down. If possible, immerse the patient's limbs in warm water to reduce blood flow to the heart. Measure blood pressure: if the numbers are elevated, give a nitroglycerin tablet under the tongue.
Signs of chronic heart failure:
Shortness of breath - with physical effort, and with a long course of the disease - even at rest. Inability to exercise - the heart cannot provide the blood flow necessary for active activities. Shortness of breath and weakness appear. Cyanosis - due to a lack of oxygen in the blood, the skin turns blue. The most common cyanosis is on the lips, fingertips, and the rim of the ears (acrocyanosis). Edema - the first thing to occur in CHF is swelling of the extremities. Then excess fluid begins to accumulate in the cavities: pleural, abdominal. Over time, edema due to heart failure and other congestion lead to pathological changes in the lungs, liver, and kidneys.
1 Ultrasound for heart failure
2 Ultrasound for heart failure
3 Diagnosis of heart failure
Treatment
Therapy is always aimed at eliminating the underlying pathology.
In acute or severe forms of chronic insufficiency, the patient is prescribed bed rest and complete physical and mental rest. In other cases, patients need to adhere to moderate loads. You should also limit your salt and liquid intake. Additionally, a diet is prescribed. Patients' nutrition should be balanced. Particular attention is paid to easily digestible foods with plenty of vitamins.
If an attack develops, the patient is hospitalized. He is urgently given nitroglycerin, diuretics, and oxygen inhalations. For ascites, fluid is removed by puncture. If the pathology provokes hydrothorax, pleural puncture is performed.
Pharmacotherapy is also required. It allows you to prolong and improve the patient's life.
For pathology, the following drugs are recommended:
- Glycosides. They allow you to increase the level of myocardial contractility, increase its diuresis and pumping function, and the body’s resistance to physical stress.
- ACE inhibitors and vasodilators. These drugs dilate arteries and veins and reduce vascular tone. Due to this, the resistance of the arteries is reduced during heart contractions.
- Nitrates. These drugs increase cardiac output, improve filling of the ventricles with blood and dilate the coronary arteries.
- Diuretics. With the help of these drugs, the risk of fluid retention in the body is reduced.
- Beta blockers. These drugs improve the filling of the heart with blood, increase its output and reduce heart rate.
- Anticoagulants. These drugs prevent the formation of blood clots in blood vessels.
Drugs that improve myocardial metabolism are also prescribed.
We know exactly how to carry out complex therapy for pathology and eliminate major diseases. Prices for services in our clinic in Moscow are relatively low. The approximate cost is indicated on the website. You can find out the price of a specialist consultation or a specific examination from our specialists.
What is heart failure?
Our heart is like a pump that pumps blood and supplies oxygen and nutrients to all parts of the body. Impaired ability of the heart to pump blood leads to stagnation and leads to the development of heart failure .
Poor blood supply puts other organs and tissues at risk. In terms of prevalence, heart failure rivals the most well-known infectious diseases.
According to statistics, around 28 million people suffer from heart failure throughout Europe. In our country, the number of patients with this disease exceeds 9 million (more than 25% of them are under 60 years of age)! At the same time, Russians die from it 10 times more often than from myocardial infarction.
1 Tests for heart failure
2 Tests for heart failure
3 Tests for heart failure
Prevention
Measures to prevent deficiency are:
- Elimination of factors contributing to its development.
- Elimination of concomitant pathologies.
Prevention necessarily includes:
- Rejection of bad habits.
- Weight loss (if it is overweight).
- Moderate physical activity.
To prevent the progression of the disease, you should take all prescribed medications and be constantly monitored by a cardiologist. It is also important to follow all treatment rules.
Causes of heart failure
A variety of diseases can lead to this disease, but more often its development is facilitated by:
- cardiac ischemia;
- arterial hypertension;
- heart defects;
- myocardial infarction;
- myocarditis;
- cardiomyopathy (including alcoholic);
- arrhythmias;
- thyroid diseases;
- diabetes.
Risk factors for developing heart failure include smoking, drinking alcohol or drugs, taking certain medications, and being overweight.
1 ECG for heart failure
2 Ultrasound for heart failure
3 ECHO-CG for heart failure
Advantages of the clinic
We employ highly qualified specialists. They conduct successful examinations and therapy for various diseases. The multidisciplinary nature of the clinic (work in such areas as cardiology, gynecology, urology, etc.) allows doctors of various specializations to work in a single team. Combining knowledge and skills makes it possible to eliminate even serious pathologies. All specialists comply with medical ethics, have extensive diagnostic capabilities and provide a safe and comfortable environment for all patients. In addition, our clinic adheres to a loyal pricing policy. Anyone can benefit from the help of professionals. Unique comprehensive therapeutic programs are used in priority medical areas. We are ready to eliminate not only the obvious manifestations of pathologies, but also their causes.
Each patient is valuable to us, first of all, as an individual, and not as a patient with an interesting medical history or a client who creates the financial well-being of a specialist. In our clinic you do not spend money on treatment, you invest it in your health.
Contact us!
Our medical center provides the widest range of services. You can always contact us regarding the treatment of diseases in cardiology. We are ready to provide you with ] treatment of premature ventricular excitation syndrome[/anchor] and treatment of sick sinus syndrome.
Diagnosis of heart failure
When diagnosing a disease, it is extremely important to identify the true cause of its development - only then can treatment be as successful as possible.
After collecting an anamnesis and physical examination, a cardiologist may prescribe:
- general clinical, biochemical blood and urine tests;
- electrocardiography (at rest);
- Ultrasound of the heart (Echocardiography);
- chest x-ray;
- coronary angiography;
- Holter ECG monitoring and other studies.
Causes of AHF
The loss of the heart's ability to contract can be caused by overload of the heart muscle, for example, due to increased blood pressure, a decrease in the number of functioning muscle fibers, heart rhythm disturbances, or the inability to adapt to physical and emotional stress.
The leading causes of AHF are cardiac, associated with pathologies of the heart itself:
- Acute coronary syndrome (ACS) is a condition caused by a sudden disruption of the blood supply to the heart. It develops with thrombosis of the arteries that supply blood to the heart muscle, narrowing of the heart vessels caused by the presence of atherosclerotic plaques or spasm. It manifests itself as myocardial infarction - irreversible necrosis of the heart muscle and a pre-infarction state, which is not accompanied by a complete cessation of blood supply to the myocardium, but can result in a heart attack. The leading symptoms of ACS are severe chest pain and specific changes in the electrocardiogram (ECG).
- Hypertensive crisis. It is caused by a persistent increase in blood pressure (BP) and is accompanied by certain symptoms: headache, nausea and vomiting, shortness of breath, visual disturbances, sometimes convulsions, chest pain due to insufficient blood supply to the myocardium.
- Sudden arrhythmias and heart blocks. The following are considered life-threatening: complete inability to conduct a cardiac impulse to the ventricles of the heart from the atria, when each of them contracts in its own rhythm (AV block), a decrease in the heart rate (HR) to 40 beats/min and below, paroxysmal tachycardia, cardiac arrest . “Precursors” of dangerous arrhythmias are heart rate less than 50 and more than 110 beats/min, frequent extraordinary heart contractions, atrial fibrillation.
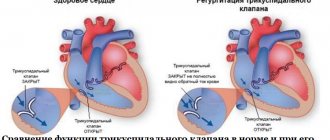
- Severe heart valve defects. They appear against the background of rheumatism and other connective tissue pathologies, atherosclerosis, coronary artery disease (IHD) and severe infections. Various defects lead to overload of the heart with pressure or volume, which creates an obstacle to the release of blood into the circulatory system. With myocardial infarction, ruptures of the tendon structures of the mitral and tricuspid valves are possible with the formation of valvular insufficiency.
- Acute myocarditis. These are severe inflammatory lesions of the heart muscle caused by viruses or bacteria.
- Cardiac tamponade. This is the accumulation of blood or other fluid between the layers of the outer lining of the heart, which prevents adequate heart contractions and filling the heart with blood. Tamponade occurs with wounds and trauma to the heart, dissection and rupture of an aortic aneurysm (protrusion), myocardial infarction with rupture of the heart wall (transmural infarction), pericarditis due to infections and cancer. The accumulation of 500 ml of fluid in the pericardial cavity leads to cardiac arrest.
- Chronic heart failure (CHF) in the stage of decompensation.
Extracardiac causes of AHF are:
- Thromboembolism of the pulmonary artery (PE) and its branches. The source of pulmonary embolism is thrombosis of the veins of the lower extremities with thrombophlebitis, in the postoperative period, with prolonged immobility of the body and limbs due to injuries (most often).
- Acute circulatory disorders of the brain, in which the release of vasoactive hormones occurs (they maintain high pressure in the vessels of the lungs).
- Pneumothorax is the accumulation of air in the chest cavity due to lung diseases and due to chest injuries. With tension pneumothorax, with each inhalation and exhalation, the volume of air in the chest increases, the lung on the affected side collapses, and the heart moves to the opposite side. In this case, the venous return to the heart and the contractile function of the myocardium are disrupted.
Risk factors
Factors that increase the risk of developing acute heart failure include:
- failure to comply with recommendations for the treatment of CHF;
- physical stress and emotional stress;
- severe acute infections and pneumonia;
- an increase in BCC (circulating blood volume) with excessive intravenous drips of drugs (for kidney disease, in patients with CHF);
- renal failure;
- alcohol abuse;
- overdose of drugs with cardiotoxic effect;
- bronchial asthma.
Forms of the disease
The following forms of left ventricular AHF are distinguished:
- Acute decompensated heart failure is an extreme degree of heart failure that appears for the first time.
- Hypertensive AHF. It is characterized by high blood pressure and venous congestion in the lungs, which is visible on x-ray.
- Pulmonary edema is a high degree of blood stagnation in the capillaries of the lungs with the release of the liquid part of the blood with red blood cells into the lumen of the alveoli, the formation of foamy sputum and impaired gas exchange. Blood oxygen saturation in pulmonary edema before treatment is less than 90% (normally 96–99%).
- Cardiogenic shock is a sudden decrease in cardiac output and systolic pressure to 90 mmHg. Art. and below, which lead to a significant decrease in blood supply to organs and tissues. The main causes of cardiogenic shock are severe rhythm disturbances and myocardial infarction.
- AHF with high cardiac output. A rare form of deficiency. Accompanies those pathologies in which the heart rate increases: severe anemia, thyrotoxicosis, arrhythmias, sepsis.
The main forms of acute left ventricular failure are listed above. The first three are the most common. These include up to 90% of all cases of hospitalization with AHF. Acute right ventricular failure is less common. It develops mainly in severe lung diseases, right ventricular myocardial infarction and pulmonary embolism.
Symptoms of AHF
The symptoms of acute left ventricular and right ventricular failure are different.
Symptoms of left ventricular AHF
Acute left ventricular failure almost never occurs in healthy people. It is preceded by undetected or inadequately treated hypertension, heart defects, ischemic heart disease with cardiosclerosis, arrhythmias, and myocardial infarction.
Provoking factors may be physical activity, stress, intravenous infusion of an excess volume of dissolved drugs. In some cases, symptoms develop at night due to increased pulmonary congestion or heart rhythm disturbances.
The main manifestations of left ventricular AHF are cardiac asthma, pulmonary edema and cardiogenic shock. These conditions are a consequence of severe stagnation of venous blood in the lungs. They can develop sequentially, accompanied by the following symptoms:
- severe shortness of breath, which can cause suffocation;
- fear of death, dizziness, weakness;
- persistent chest pain;
- forced sitting position with support on hands to facilitate breathing - orthopnea;
- cough is dry, then wet, with foamy pink sputum;
- the skin is pale, covered with cold sweat, there may be a bluish discoloration of the lips, ears, nose;
- pulse is frequent (more than 90 beats/min), weak filling, often arrhythmic;
- Blood pressure may be elevated or normal and decreases as symptoms progress.
Symptoms of right ventricular AHF
With this pathology, “acute cor pulmonale” (ACP) develops. Causes of ULS:
- acute severe diseases of the bronchopulmonary system - a prolonged attack of bronchial asthma, extensive acute pneumonia, total right-sided pleurisy, tension pneumothorax;
- blockage of large branches of the pulmonary artery by blood clots, fat and tumor cells, and air;
- extensive infarction of the interventricular septum with transition to the right ventricle.
Symptoms of acute right ventricular failure include:
- signs of causative diseases;
- sudden shortness of breath and an increase in respiratory rate of more than 20 in one minute;
- pain in the right hypochondrium (when pressure is applied to the liver, the neck veins dilate);
- cyanosis of the skin, rapidly developing swelling of the legs;
- frequent weak pulse, possible bradycardia and decreased blood pressure.