Find out more about diseases starting with the letter “K”: Causalgia, Brain cyst, Cluster headache, Tick-borne encephalitis, Kozhevnikov epilepsy, Colloid cyst of the third ventricle, Coma, Compressive myelopathy, Balo concentric sclerosis, Radicular syndrome, Corticobasal degeneration, Craniovertebral anomalies, Craniospinal tumor, Craniopharyngioma, Myasthenia gravis crises, Hemorrhage into the ventricles of the brain.
Coma is a pathological disorder of consciousness, borderline between life and death, and poses a certain danger to human life. Translated from Greek “deep sleep”. It occurs through damage to special areas of the brain and is determined by the patient’s complete lack of connection with the surrounding reality. Occurs due to metabolic or organic root causes.
Characterized by a lack of consciousness and reflexes of the pupils of the eyes to the brightest stimuli. Computed tomography and magnetic resonance imaging and laboratory blood tests have a key role in diagnosing coma. All therapeutic measures are focused on eliminating the factors of the pathological process
general information
During a comatose state, the patient completely loses contact with others. A profound impairment of consciousness is determined by the complete absence of mental activity. Even intense stimulation cannot bring the patient out of this state. Coma is different in that the patient is always in a supine position with his eyes closed, which he does not open when exposed to sound stimuli or pain.
Clinical symptoms depend on the cause of occurrence and the severity of suppression of the nervous system - absence or presence of spontaneous movements, extinct or preserved reflexes, spontaneous breathing, dependence on life-supporting equipment.
The origin is due to extensive damage to special brain areas responsible for wakefulness.
What could be the way out of a coma?
There are three options for exiting a coma. The first involves partial restoration of the nervous system and brain function. After this, everything will depend on the success of the rehabilitation course. In some cases, a person recovers so much that he can do without outside help and live an almost normal life.
Of course, some consequences will still remain. Staying in a coma cannot pass without leaving a trace. It is likely that motor, speech, and cognitive impairments will remain, and personality changes will occur. But this is something that a person’s loved ones are usually prepared for. His return in itself is perceived by them as salvation.
Even when, despite long-term rehabilitation, a person remains disabled, this is not the worst thing that can happen to him. Because the second option is to exit the coma into a vegetative state.
In this case, cognitive, motor, and speech abilities will be lost. But the person will remain alive, and as long as he is alive, there will be hope. Even if from a medical point of view it is equal or close to zero.
The person will need constant care, attention, care, to which he probably will not even respond. Not everyone close to you is ready for this. But still, this is not the worst thing, because there is a third option for exiting a coma - death.
Our task, the doctors of the department of anesthesiology and intensive care of the International Clinic Medica24, is to ensure that the person comes out of the coma according to the first option. And when we succeed, we consider it our victory and success. This is the best reward for our efforts.
We will call you back
Message sent!
expect a call, we will contact you shortly
Causes
The occurrence of coma is always caused by damage to the nerve pathways caused by severe pathologies of the central nervous system. A coma cannot be an independent disease.
The reticular formation is a mesh-like structure that runs throughout the brain. All signals from the surrounding reality pass through it, filtered and systematized. When the cells of this unique system are damaged, the nervous system's connection with the outside world is lost.
The causes of damage to the reticular pharmacy system are divided into:
- Physical: cerebral hemorrhages, injuries, bruises, bullet wounds, strokes.
- Chemical, in turn, are divided into external and internal. Poisonous compounds coming from outside can be narcotic substances, sleeping pills, neurotropic poisons, toxic toxins in infectious diseases. Internal chemical compounds are formed as a result of metabolism and diseases of internal organs. These include ammonia (severe liver pathologies), abnormal levels of glucose and acetone (diabetes mellitus), and insufficient oxygen in the blood (hypoxia).
- The most severe is the combination of physical and chemical effects on the reticular formation. The result is a worsening of intracranial pressure indicators. This case occurs with tumors of the central nervous system and traumatic brain injuries.
How does a coma develop?
The basis of clinical coma syndromes is depression of consciousness, resulting from a mismatch of interneuronal interactions and progressive deep inhibition. The mediator biochemical mechanism is a factor that determines the rate of growth of comatose lesions. Its timely correction determines the subsequent possibility of restoring consciousness. Morphological damage to brain cells indicates the irreversibility of the process of depression of consciousness.
The etiology of comatose lesions is very extensive, however, the pathogenetic algorithm for the development of the disease is universal, and consists of metabolic disorders, on which the satisfaction of the energy needs of the brain directly depends. Normal blood flow in the brain is the basis for adequate metabolism. In the absence of sufficient oxygen supply to brain cells, hypoxia develops in them, which further causes a chain of pathological processes based on impaired metabolism of nerve cells. As a result, the patient experiences a decrease in the production of adenosine triphosphate, a substance involved in metabolic processes. The patient develops intracellular acidosis, the permeability of the vascular walls increases, and cerebral edema forms. These factors negatively affect the state of blood flow in the brain and increase the state of hypoxia.
Due to hypoglycemia, lactate, calcium ions, and free fatty acids accumulate inside the cells, causing the cells to die.
Disorders of the acid-base state are characterized by metabolic acidosis, while electrolyte balance disorders can be based on pathological changes in the concentration of sodium, potassium, calcium, and ammonium ions.
Hypoxia and changes in acid-base balance are factors that provoke swelling and edema of the brain, the appearance of intracranial hypertension.
Classification
Comatose states are classified according to groups of criteria:
- the reason that caused it;
- degree of depression of consciousness.
Depending on the reasons, they are divided into the following types:
- traumatic - as a consequence of cranial and brain injuries;
- epileptic - as a worsening of epilepsy;
- apoplexy - the result of a stroke;
- meningeal - a consequence of meningitis;
- tumor - neoplasms in the skull;
- endocrine - during diabetes mellitus, a decrease in the properties of the thyroid gland;
- toxic - a consequence of renal and liver failure.
Causal classification does not reflect the patient’s actual well-being, and therefore is not used in neurology. Professionals in this field of medicine classify the case according to the severity of the person’s condition - the Glazko scale. The method is based on a general assessment of three indicators: the patient’s speech, the presence of body movements, and the opening of the eyelids. Depending on the severity of their violations, a certain number of points are assigned. The sum of the scores determines the patient’s degree of consciousness:
- 15 points - clear consciousness;
- 14-13 points - moderate stunning;
- 12-10 - deep stun;
- 9-8 - stupor;
- 7 or less - comatose state.
Based on these data, the severity of a person’s situation can be easily calculated, emergency treatment tactics can be quickly developed and the outcome of the disease can be predicted.
In intensive care circles, doctors divide coma into 4 degrees:
- I - stupor of consciousness;
- II - stupor;
- III - atonic;
- IV - beyond.
Clinical symptoms
The main clinical sign is the patient’s absolute lack of consciousness, deprivation of mental activity and contact with the outside world. All other manifestations of the disease are associated with the causes that caused brain damage:
- Body temperature indicators. Hypothermia occurs in case of poisoning with sleeping pills, alcohol (can decrease to 32-34 C⁰). An increase in temperature to 42-43 C⁰ and dry skin accompany a coma caused by general overheating.
- Respiratory frequency. Slow, shallow breathing is a sign of an overdose of morphine-containing drugs, sleeping pills, and a decrease in the level of thyroid hormones. Deep breathing is a distinctive feature against the background of infectious intoxication due to pneumonia. This symptom occurs with kidney failure, brain tumors, uncontrolled sugar levels in diabetes in the form of acidosis.
- Pulse and blood pressure. A decrease in heart rate (bradycardia) signals coma due to heart pathologies. Frequent heartbeat - tachycardia, in combination with significant blood pressure numbers, indicate an increase in intracranial pressure. Hypertension, as a symptom, appears in patients in a coma after a stroke. Low blood pressure occurs in cases of poisoning with sleeping pills, heavy intra-abdominal bleeding, myocardial infarction, and diabetic coma.
- Skin color is also a significant diagnostic symptom. When intoxicated with carbon monoxide, the skin gradually acquires a dark red color. Suffocation is accompanied by a sharp decrease in the level of oxygen in the body’s blood, as a result of which the nail phalanges of the fingers and the nasolabial triangle turn blue. Bleeding from the ears and nose, bruises, bruises around the eyes (“a symptom of glasses”) correspond to a coma that manifested itself as a result of a traumatic brain injury. If the coma is caused by global blood loss, the skin becomes distinctly pale.
- Maintaining contact with others. A favorable encouraging sign is the ability of patients to utter some sounds. This is observed with mild coma or stupor. The more severe the patient's condition becomes, the faster the ability to make sounds is lost. The mild form is also characterized by reflex movements of the limbs in response to pain, possibly causing grimaces.
Anatomical and functional features of the central nervous system
Being the central regulator of all processes occurring in the body, the brain operates in an active metabolic mode. Its weight is only 2% of body weight (about 1500 g). However, for the uninterrupted functioning of the brain, 14-15% of the total volume of circulating blood (700-800 ml) must flow into and out of the cranial cavity every minute. The brain uses 20% of all the oxygen the body consumes. It is metabolized only by glucose (75 mg per minute or 100 g per day).
So, the physiological functioning of brain tissue depends on adequate perfusion with its blood, the content of a sufficient amount of oxygen and glucose, the absence of toxic metabolites and the free outflow of blood from the cranial cavity.
A powerful autoregulation system ensures smooth functioning of the brain. Thus, even with significant blood loss, the perfusion of the central nervous system is not impaired. In these cases, a compensatory reaction of centralization of blood circulation with ischemia of less important organs and tissues is activated, aimed primarily at maintaining adequate blood supply to the brain. The body reacts to another pathological condition - hypoglycemia - by increasing blood flow to the brain and increasing the transport of glucose here. Hyperventilation (hypocapnia) reduces blood flow to the brain; hypoventilation (hypercapnia) and metabolic acidosis, on the contrary, increase blood flow, promoting the removal of “acidic” substances from tissues.
With significant damage to brain tissue, insufficient autoregulation or excessive manifestations of the compensatory reaction of the inflow and outflow of blood, the brain cannot voluntarily change its volume. The closed cavity of the skull becomes its trap. Thus, an increase in intracranial volume by only 5% (with hematomas, tumors, hyperhydration, liquor hypertension, etc.) disrupts the activity of the central nervous system with the patient losing consciousness. In another pathology, excessive growth of cerebral blood flow leads to overproduction of cerebrospinal fluid. The brain tissue is compressed between the blood and the cerebrospinal fluid, swelling develops, and functions are impaired.
Traumatic destruction of brain tissue, edema and swelling, increased intracranial pressure, impaired circulation of cerebrospinal fluid, circulatory disorders and other damaging mechanisms lead to hypoxia of CNS cells. It manifests itself primarily as a disturbance of consciousness.
Diagnostics
The diagnosis immediately establishes the causes of the comatose case. The conclusion differentiates the condition from other similar disorders of consciousness. The following diagnostic methods are used:
- Anamnesis collection. They find out from the patient's relatives or witnesses whether the patient took medications, and whether empty jars or blisters of medications were found nearby. You should ask about the presence of chronic diseases of blood vessels, endocrine glands, and heart. Clarify that the patient may have voiced complaints. An important factor is the age of the patient and the speed of development of symptoms. Young people more often fall into this state after poisoning with sleeping pills or narcotic drugs. In elderly patients, the formation of a coma occurs against the background of heart attacks, strokes, and other cardiovascular diseases.
- Inspection. During the examination, the possible root cause of the coma is determined. Respiratory rate, pulse rate, blood pressure, body temperature, injection marks, bad breath, bruises are indicators on the assessment of which the establishment of a correct diagnosis depends.
- The patient's position can also characterize the severity of brain damage. During hemorrhages and meningitis, the patient’s head is thrown back, the neck muscles have a pronounced tone - signs of irritation of the meninges. Convulsive attacks, cramping spasms of individual muscles indicate the patient’s status epilepticus, the condition of eclampsia in pregnant women. Unexpressed paralysis of the limbs indicates a stroke, a complete absence of reflexes indicates deep lesions of the cortex and spinal cord.
- A differential feature distinguishing it from other disorders of consciousness was the study of the patient’s function to open his eyes to irritation in the form of sound or pain. If the response to sound and pain stimulation in the form of involuntary opening of the eyes persists, then this is not a coma. If the eyes remain closed, the case is considered comatose by doctors.
- The doctor carefully evaluates the ability of the pupils to respond to light. Its quality makes it possible to determine the damaged area of the brain, and also indicates the factor that provoked the coma. The clarity of the pupil's reaction to light indicates the future prognosis of the disease.
Pinpoint pupils that do not respond to bright light indicate alcohol or drug poisoning. If the pupils of the left and right eyes have different diameters, this is a sign of increasing intracranial pressure. Excessively wide pupils are a symptom of midbrain pathologies. If, when exposed to bright light, the reaction of the pupils is completely absent, their diameter remains wide, this is a very unfavorable symptom, which indicates imminent brain death.
The development of medicine makes it possible to use hardware methods for diagnostic purposes to examine patients with impaired consciousness immediately upon admission to a medical institution. Performing head computed tomography (CT), magnetic resonance imaging (MRI) makes it possible to detect changes in areas of the brain, lesions, tumor-like neoplasms, and signs of intracranial hypertension. The conclusions obtained as a result of the tomograph study serve as the basis for determining treatment tactics - surgical or conservative.
X-rays of the head and spine in several projections are performed if MRI or CT is not possible.
A biochemical blood test can confirm a metabolic failure. Tests for the level of glucose, urea, acetone, and ammonia in the blood are carried out very quickly. The ratio of the content of electrolytes and blood gases is determined. In addition, the blood is examined for insulin levels, adrenal and thyroid hormones, for the presence of narcotic substances, tranquilizers and other toxic drugs, and bacterial blood cultures are performed to identify a possible infectious agent.
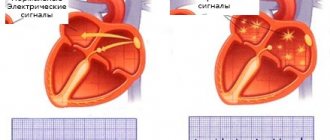
During an electroencephalogram (EEG), electrical impulses from the brain are recorded, which make it possible to determine the type of coma and understand what caused it - hemorrhage, poisoning or a tumor.
Stages
The comatose state is classified according to stages. There are 4 of them in total, but doctors additionally identify precomatose. The main ones describe how serious the patient’s condition is. The first is considered the weakest, and the fourth is the most serious. To determine the exact depth of the condition, doctors use the Glasgow scale, its improved version, the Glasgow-Pittsburgh scale, or the Shakhnovich version. To evaluate, doctors study how the patient's eyes open, what his speech is like, and how much he can move.
The precomatose state can last from a couple of minutes to several days. It all depends on the state of the brain and the root cause of the problems. If you provide help to the patient at this moment, the chance of recovery will be much higher. The symptoms of a precomatose state may resemble some diseases. It is accompanied by deafness and confusion, drowsiness, very sound sleep, disorientation in space, physical and mental weakness, headaches, attacks of nausea, while the patient will be able to move, blink and talk. Over time, symptoms worsen. It is accompanied by dehydration, increased heart rate, a feeling of fear, facial cramps, loss of appetite and dry skin. After this, a coma sets in.
Second degree
With the 2nd degree of coma, the work of the subcortical structures of the brain is inhibited, and in parallel with this, the functioning of some parts of its trunk is disrupted. Any connection with the patient is completely absent, and he himself is in the deepest sleep stage, which is the main symptom of this stage. Along with this, involuntary physical movements may occur. They are usually chaotic and caused by cramps, fibrillation or instability of muscle tone in the limbs. The patient ceases to feel, which is why he does not perceive pain. The pupils narrow and also stop responding to any stimuli.
Other symptoms also appear:
- significant increase in body temperature;
- excessive sweating;
- blood pressure surges;
- noticeable tachycardia;
- fecal and urinary incontinence.
Stage 2 coma may result in breathing problems. It may have pauses, be too loud or unstable in the depth of breaths. It often resembles snoring. Sometimes this causes pneumonia to develop, which creates even more problems. If the respiratory center inside the medulla oblongata is affected, the patient will experience a Cheyne-Stokes type disorder, characterized by superficial and unstable movements of the chest. It is also possible to develop Kussmaul breathing, characterized by very deep breaths.
Doctors were able to find out whether a person can hear while in a second-stage coma. If his auditory analyzer located in the brain is not damaged, then theoretically he could hear the speech of others. But in practice this is impossible, since the patient is not able to perceive words spoken by anyone nearby. The brain simply does not allow us to analyze them, comprehending each of them.
The condition can be dynamic. Therefore, coma is capable of moving from one stage to another.
Treatment
Treatment is a complex, comprehensive process that must prevent death, maintain vital body functions, and at the same time combat the root cause of this condition.
The first resuscitation measures aimed at preserving a person’s life are carried out immediately upon the arrival of the ambulance team and during transportation of the patient, before all diagnostic procedures are carried out. First aid consists of fixing the patient's position, ensuring patency of the airway - straightening the tongue, clearing the nose and mouth of vomit, an oxygen mask, tracheotomy with the installation of a breathing tube. It is necessary to normalize blood circulation by administering medications that normalize cardiac activity and blood pressure. If necessary, indirect cardiac massage is performed.
In the intensive care unit, the patient is connected to an artificial respiration apparatus. Medicines are administered aimed at eliminating the pathological symptoms of the disease - anticonvulsants, antipyretics, hemostatics. Intravenous infusions of glucose and saline solutions are required. Measures are necessary to normalize body temperature. In case of hypothermia, the patient is covered and covered with hot water bottles. If there is a suspicion of poisoning with chemical or pharmacological drugs, gastric lavage is performed.
At the second stage, having detailed results of all types of examinations, the cause is eliminated. In case of hyperglycemic coma, measures are taken to normalize blood sugar and insulin levels. In case of renal failure, hemodialysis is performed. If an injury, hematoma or brain tumor is detected, urgent or planned surgical intervention is performed according to indications.
Prognosis and possible prevention
Predicting the situation while a patient is in a coma is based on the degree of brain damage and the causes of the disease. The more severe the patient’s condition, the more likely an unfavorable outcome is possible. The patient's chances of recovery are assessed according to the following measures:
- precoma, coma I - the prognosis is favorable, complete recovery is possible without residual effects;
- coma II and III - an unreliable position that can lead to both recovery and death of the patient,
- coma IV - in most cases leads to the death of the patient, the prognosis is extremely unfavorable.
Early prevention is focused on timely diagnosis of major disorders of the cardiovascular system, various tumor pathologies and other conditions that can lead to coma.