Home — For the public
- Map of medical organizations
- Vaccination
- Clinical examination
- Fluorography
- Addresses and opening hours of clinics
- Emergency rooms
- Oncology
- Where to take an HIV test
- Healthy child's office
- Services
- Prevention of CVD
- Disease Prevention
- World Patient Safety Day
- Newspaper "Medical News"
- specialist
- School of Health
— Disease prevention
- HIV infection
- All about vaccination
- All about proper nutrition
- Hepatitis
- Flu
- Dementia
- Schoolchildren's health
- STD
- Tick-borne encephalitis
- Whooping cough
- Measles
- Legionellosis
- Meningococcal infection
- Oncology
- Acute intestinal infection
- Pediculosis
- First aid
- Pneumococcal infection
- Pneumonia
- Prevention of rabies
- Dependency Prevention
- Rotavirus infection
- Diabetes
- Cardiovascular diseases
- Injuries
- Tuberculosis
- Tularemia
- Physical activity
- Obstructive pulmonary disease
- Exotic infections
- Ecology
- Why is swimming in ponds dangerous?
— Cardiovascular diseases — Disease of peripheral arteries and veins
Diseases of peripheral vessels and arteries are a group of inflammatory diseases, which in most cases are accompanied by damage to the arteries and veins of the lower (less often, upper) extremities. With these pathologies, a narrowing or significant expansion of the lumen of blood vessels occurs, blood circulation and tissue nutrition in the affected areas are disrupted.
A number of these diseases are caused by atherosclerotic changes in the walls of the arteries, and varicose veins or aneurysms of the aorta and arteries are provoked by pathological overstretching of the venous and arterial walls. The diagnosis is established on the basis of a physical examination and the results of some instrumental studies, which make it possible to visualize the nature of changes in the walls of blood vessels. In severe cases, patients with such diseases may require surgical operations to correct vascular pathology; in milder cases, the resulting disorders can be eliminated conservatively.
Obliterating atherosclerosis
Peripheral artery disease (PAD) in most cases is caused by atherosclerosis, another systemic disease characterized by abnormalities in the structure of the artery walls. Atherosclerotic plaques form in the lumen of the vessels, leading to the settling of blood clots, narrowing of the arterial lumen and the appearance of areas of thrombosis. As a result, the trophism of the tissues surrounding the affected vessels is disrupted, they begin to suffer from ischemia (insufficient blood flow) and the patient develops obliterating atherosclerosis.
Thrombosis usually affects the vessels of the lower extremities at the level of:
- abdominal aorta (Leriche syndrome) – the infrarenal section of the abdominal aorta narrows and blood circulation is impaired in both legs;
- pelvis – the iliac artery is affected;
- hips – the lumen of the femoral artery is blocked;
- shins – blood clots settle in the arteries of the legs and feet.
With significant narrowing of the peripheral arteries of the legs, tissue trophism can be so disrupted that the patient develops trophic ulcers due to constant ischemia and gangrene can develop, leading to the need for amputation of the leg. In addition, atherosclerosis is prone to progression and the patient’s risk of developing myocardial infarction and stroke increases in the future, since both the coronary and carotid arteries are involved in the pathological process.
The process of occurrence and spread of atherosclerotic plaques occurs unnoticed in almost 50% of patients. Often, patients with such pathologies consult a doctor only when conservative treatment methods are not enough to restore blood flow and there is a need for surgical correction of the affected arteries.
The causes of PAD are the same as the factors that provoke the development of atherosclerosis:
- *imbalance in lipoproteins and accumulation of cholesterol in vascular walls;
- autoimmune pathologies accompanied by infiltration of vessel walls with leukocytes and macrophages;
- congenital defects in the structure of blood vessels;
- hormonal imbalances of adrenocorticotropic and gonadotropic hormones, leading to increased cholesterol levels in the blood;
- failures in antioxidant systems;
- brought infections.
*Elevated is considered to be a total cholesterol level of more than 8 mmol/l, an HDL level in men of less than 1 mmol/l and in women less than 1.3 mmol/l, an LDL level of more than 6 mmol/l, and a triglyceride level of more than 1.7 mmol/l.
All these reasons can trigger the process of formation of atherosclerotic deposits, but the leading role in damage to peripheral arteries lies in lipid balance disorders. According to statistics, men over 40–45 years of age are more likely to encounter such pathologies.
The following controllable and uncontrollable factors can predispose to the development of atherosclerotic lesions of the arteries:
- age (for women after 55 years and men after 45 years);
- smoking;
- postmenopausal period;
- excess weight and waist circumference in women is more than 88 cm, and in men more than 100 cm;
- arterial hypertension more than 180/110 mm Hg. Art.;
- diabetes;
- hypothyroidism;
- hereditary disorders (coagulopathies, homocystinuria);
- hereditary predisposition to vascular and heart diseases;
- congenital vascular anomalies;
- adynamia;
- taking a large amount of fast food, fatty, fried, flour, sweets, baked goods, carbonated drinks;
- taking medications that increase blood cholesterol levels;
- taking hormonal contraceptives;
- disorders in the blood coagulation system, accompanied by increased thrombus formation;
- frequent stress;
- chronic sleep deficiency.
Uncontrollable factors cannot be eliminated. They contribute to the formation of atherosclerotic plaques, but in the absence of controlled conditions are not capable of causing obliterating atherosclerosis.
With the development of atherosclerosis, the following occurs:
- on the inner wall of the artery, a lipid stain is formed that transforms into liposclerosis, leading to the formation of unstable atherosclerotic plaques, which can still dissolve;
- fibrous plaques appear that can no longer resolve, and atheromatosis develops, accompanied by the disintegration of the contents of plaques, collagen and elastin in the vessels;
- when plaques disintegrate, the stage of complications of atherosclerosis begins: thrombosis, embolism, rupture of the aneurysm formed in the lumen of the artery;
- the formation of atherocalcinosis - this stage is accompanied by the deposition of calcium salts in the atherosclerotic plaque and severe ischemia of tissues and organs.
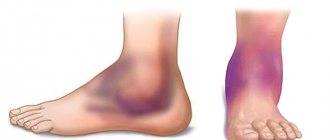
Symptoms of peripheral artery disease do not appear immediately, but only at the stage of severe ischemia of a particular area. Initially, the patient complains of pain, cramps and fatigue in the legs after walking or physical activity. The pain is usually located in the thighs, buttocks and feet. Sometimes patients may experience swelling. There is also no pulsation in the area of damage to the arterial vessel. The skin on the affected limb becomes paler and cooler to the touch at the level of the arterial lesions. Men may experience problems with potency due to impaired blood flow.
Somewhat later, the patient develops a symptom characteristic of obliterating atherosclerosis of the lower extremities, such as intermittent claudication (claudication) - pain and cramps in the calf muscles, aggravated by walking. It is provoked by a lack of oxygen, which is most pronounced during walking, and disappears after the person stops.
Intermittent claudication is most pronounced when climbing stairs. Initially, it occurs after walking long distances, and then, as atherosclerotic lesions of the arteries and ischemia progress, it appears even after covering very short distances. In the most advanced stages, it occurs even during rest. This condition is commonly called critical ischemia.
The stages of PAD are:
- I – symptoms of thrombosis and narrowing of the arteries are not felt;
- IIa – pain and intermittent claudication occur after covering more than 200 m;
- IIb – pain and lameness occur when covering less than 200 m;
- III – pain and intermittent claudication occur at rest;
- IV – due to ischemia, ulcers and wounds occur due to tissue necrosis.
The progression of PAD is indicated by the following manifestations:
- increased pain syndrome;
- sensory disturbances and coldness of the limb;
- dry skin and the appearance of cracks prone to infection;
- the occurrence of ulcers and wounds on the feet, legs or toes.
When PAD is complicated, it leads to the development of gangrene and the need for urgent surgery to amputate the limb.
Classification
Common arterial diseases include:
- Obliterating atherosclerosis. This pathology is provoked by excessive amounts of cholesterol and lipid fractions on the walls of blood vessels. As a result, plaques form in the lumens, which can clog or narrow even a large artery.
- Diabetic angiopathy. This pathology is a complication of diabetes mellitus. It is characterized by deformation of blood vessels against the background of high concentrations of glucose in the blood. With this pathology, blood vessels become thinner and thicker. As a result, the normal passage of blood through them is disrupted. This reduces the saturation of organs with oxygen and nutrients. All metabolic processes in tissues slow down.
- Embolism. Acute thrombosis is a critical condition. It is dangerous due to the complete cessation of blood supply to a tissue or organ.
- Menkenberg's arteriosclerosis. This pathology occurs quite often and is characterized by the accumulation of cholesterol deposits and calcium salts on the walls of blood vessels. The condition is very dangerous, as it may not have any symptoms for a long time.
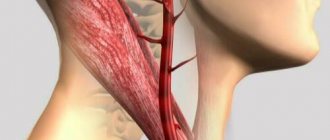
- Extravasal compressions. These pathologies are characterized by compression of blood vessels as a result of the appearance of neoplasms and intervertebral hernias. Vessels become walled and deformed. As a result, the blood supply to the brain is reduced.
- Obliterating endarteritis. This disease is chronic. It progresses rapidly and is characterized by blockage of blood vessels, provoking spontaneous gangrene.
Inflammatory vascular lesions are included in a separate group.
These include:
- Winivarter-Buerger disease (thromboangiitis obliterans). This pathology is accompanied by acute damage to the medium and small vessels of the lower or upper extremities.
- Nonspecific aortoarteritis. With this inflammatory process, the ostia of blood vessels become clogged, causing a reduction in pulse rate and a decrease in blood pressure. The pathology is also characterized by impaired blood supply to the brain and upper extremities.
- Specific aortitis and arteritis. These pathologies can affect both the entire thickness of the vessel and its individual layer. Aortitis and arteritis are dangerous because they lead to ischemia of the limbs.
Aneurysms
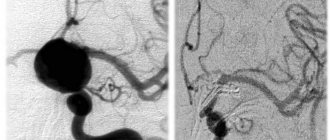
Aneurysms of peripheral arteries are characterized by the appearance of pathologically dilated areas of the arterial wall, resulting from its weakening. As a result, the artery wall bulges and this condition can be complicated by thromboembolism, strokes, or, if the arterial wall is significantly thinned, ruptures.
About 70% of such aneurysms occur in the popliteal arteries, and 20% in the iliofemoral segment. Sometimes they are combined with abdominal aortic aneurysms, which in 50% of cases are bilateral. Typically, aneurysms of peripheral arteries are provoked by atherosclerosis and infectious diseases (in such cases, the protrusion is most often localized in the femoral artery). Sometimes the root cause of their occurrence is entrapment of the popliteal artery or septic emboli, leading to the formation of a mycotic aneurysm.
Peripheral aneurysms are often asymptomatic. In some cases they are manifested by the following symptoms:
- pain when palpating;
- pallor and coldness of the affected limb;
- sensitivity disorders;
- absence of pulse in the affected area due to thromboembolism or rupture of a pathological protrusion;
- pain, fever, general malaise (if the aneurysms are infectious).
The risk of artery rupture in the area of the aneurysm is low - no more than 5% for popliteal bulges and 1 - 14% for iliofemoral aneurysms.
Symptoms of vascular occlusion
Acute occlusion of the vessels of the extremities is manifested by a symptom complex, designated in the English literature as the “complex of five Ps” (pain - pain, pulselessness - lack of pulse, pallor - pallor, paresthesia - paresthesia, paralysis - paralysis). The presence of at least one of these signs makes one think about possible acute occlusion of the vessels of the extremities.
Sudden pain distal to the site of occlusion occurs in 75-80% of cases and is usually the first sign of acute occlusion of the vessels of the extremities. If collateral circulation is preserved, pain may be minimal or absent. More often, the pain is diffuse in nature with a tendency to intensify, and does not subside when the position of the limb changes; In rare cases of spontaneous resolution of occlusion, the pain disappears on its own.
An important diagnostic sign of acute occlusion of the vessels of the extremities is the absence of pulsation of the arteries distal to the site of occlusion. In this case, the limb first turns pale, then acquires a cyanotic tint with a marbled pattern. Skin temperature is sharply reduced - the limb is cold to the touch. Sometimes, upon examination, signs of chronic ischemia are revealed - wrinkled and dry skin, lack of hair, brittle nails.
Disorders of sensitivity and motor sphere in acute occlusion of the vessels of the extremities are manifested by numbness, tingling and crawling sensations, decreased tactile sensitivity (paresthesia), decreased muscle strength (paresis) or lack of active movements (paralysis) first in the distal and then in the proximal joints . In the future, complete immobility of the affected limb may occur, which indicates deep ischemia and is a formidable prognostic sign. The end result of acute vascular occlusion can be gangrene of the limb.
Phlebeurysm
Varicose veins are a pathological expansion of the lumen of superficial venous vessels, accompanied by incompetence of the venous valves and leading to impaired blood flow. It is usually not possible to determine the underlying cause of vascular damage. Such a disorder is usually caused by primary valvular insufficiency and reflux, primary dilatation of the venous walls due to weakness of vascular tissues, chronic venous hypertension or insufficiency.
Varicose veins are more often detected in women. It often occurs during pregnancy or difficult childbirth. There are usually no risk factors for its development, but sometimes its occurrence is explained by hereditary predisposition. As a rule, it is the veins of the lower extremities that are affected.
Symptoms of varicose veins are not always visually noticeable. At the beginning, the veins may be tense and palpable. As the disease progresses, they enlarge, protrude above the surface of the skin and become visible. The patient complains of leg pain, discomfort, fatigue, tension and pressure. Particularly pathological dilated vessels are noticeable in a standing position.
When a vein thromboses, the patient experiences severe pain, and the superficial veins can form venous bullae, which rupture and bleed at the slightest physical impact. Sometimes such bleeding goes unnoticed (for example, during sleep), and leads to death.
Ulcers and other dermatological disorders with varicose veins rarely occur. They can manifest as eczema or pigmentation that appears in the ankle area. Ulcerative lesions usually occur after injury and are small in size and superficial.
Who is at risk?
Those who lead an unhealthy lifestyle, as well as those who are predisposed to them from birth, are most at risk of developing vascular diseases.
There are general risk factors for vascular damage, which include:
- smoking – it is one of the main risk factors; male gender;
- frequent and severe stress;
- rare physical activity;
- work that involves lifting heavy objects, standing for long periods of time, or staying in one position;
- hypothermia;
- excess weight;
- a lot of salt and fat in food;
- diabetes;
- high cholesterol;
- high blood pressure.
Diagnosis of vascular diseases of the lower extremities
To identify obliterating diseases of the arteries of the lower extremities (LOAD) and aneurysms, the patient is referred to a vascular surgeon. After a physical examination, the patient may be prescribed the following tests:
- determination of the ankle-brachial index;
- Doppler and duplex ultrasound scanning;
- digital angiography;
- CT angiography and MRI angiography;
- blood tests for the level of lipoproteins VP, NP and SNP, SC myoglobin and C-reactive protein, the level of total cholesterol and triglycerides, sugar, atherogenicity coefficient.
To find out the root cause of the disease and prevent complications, the patient may be recommended to consult other highly specialized specialists: cardiologist, neurologist, endocrinologist, hematologist, ophthalmologist. If necessary, the examination of the patient is supplemented by ECG, Echo-CG, Dopplerography of the vessels of the head and neck, renal arteries, etc.
Varicose veins are usually detected during an objective examination and special tests. If necessary, the examination is supplemented with duplex ultrasound scanning of the leg veins.
Causes of the disease
The risk group for arterial diseases includes men and women of different ages with:
- hereditary predisposition;
- overweight;
- metabolic disorders;
- high blood pressure;
- diabetes mellitus
The development of pathologies can be caused by heart rhythm disturbances, elevated cholesterol levels, poor diet, autoimmune disorders, bad habits, and chronic infectious diseases.
Treatment of obliterating atherosclerosis and superficial aneurysms of peripheral vessels
Treatment of OZANK is carried out depending on the nature and severity of the manifestations of the disease. If there is a slight disturbance in the structure of blood vessels, the patient is prescribed conservative therapy and dynamic observation.
All patients are recommended to eliminate the factors that provoke the progression of the pathology:
- to give up smoking;
- weight normalization;
- treatment of arterial hypertension and control of blood pressure;
- sufficient physical activity: walking, walks, physical therapy;
- changing your diet to reduce bad cholesterol and triglycerides;
- blood sugar control;
- the use of pneumatic cuffs and stockings to eliminate stress on blood vessels.
Drug treatment is aimed at reducing thrombus formation, normalizing blood flow and treating pathologies that increase the risk of stroke and myocardial infarction. For this purpose, the patient is prescribed antiplatelet agents (Aspirin, Cardiomagnyl, etc.), Pentoxifylline, ACE inhibitors, blood thinners (for example, Clopidogrel, Cilostazol, etc.).
If it is impossible to restore normal blood flow, patients with stage II-III OZANK can undergo the following types of surgical operations:
- thromboendarterectomy - performed to eliminate short localized lesions of the aorta, common or deep femoral, iliac arteries;
- artery bypass - an additional vessel (shunt) is created to bypass the blocked artery to normalize blood supply;
- artery replacement – the affected area of the artery is replaced with an artificial vascular prosthesis;
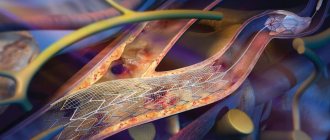
- endovascular operations (balloon angioplasty and artery stenting) - the lumen of the artery is expanded using a special balloon, which is inserted into the lumen of the artery and inflated; if necessary, a cylindrical wire structure (stent) can be installed at the site of narrowing, restoring normal blood flow.
The choice of surgical treatment method is determined by the clinical manifestations of the pathology. Endovascular interventions are less invasive and therefore doctors try to give preference to their implementation.
If surgical techniques turn out to be ineffective and the patient still develops gangrene, then to save his life, operations to amputate the limb (full or partial) are performed.
Also, for the treatment of patients with chronic ischemia of the lower extremities, angiogenesis stimulators (from autologous CD133+ endothelial progenitor cells) and Angiostimulin (a gene preparation of the vascular endothelial growth factor VEGF165) can be used.
Surgical removal of peripheral aneurysms of the vessels of the legs is indicated when the artery is dilated more than 2 times, and for protrusions in the arteries of the arms, operations are performed in all cases. To eliminate them, the affected area of the arterial vessel is excised and replaced with a graft. Sometimes an endovascular stent graft is used to repair aneurysms - a woven polyester tube covered with a metal frame is installed into the aneurysm without open surgery. This technique is used for patients who cannot undergo other types of surgery. Its purpose is to strengthen the vessel wall and prevent its rupture.
Treatment of acute vascular occlusion of the extremities
If acute occlusion of the vessels of the extremities is suspected, the patient requires emergency hospitalization and consultation with a vascular surgeon. For tension ischemia and degree IA ischemia, intensive conservative therapy is carried out, including the administration of thrombolytics (intravenous heparin), fibrinolytic agents (fibrinolysin, streptokinase, streptodecase, tissue plasminogen activator), antiplatelet agents, and antispasmodics. Physiotherapeutic procedures (diadynamic therapy, magnetic therapy, barotherapy) and extracorporeal hemocorrection (plasmapheresis) are indicated.
In the absence of positive dynamics within 24 hours from the onset of acute occlusion of the vessels of the extremities, it is necessary to perform an organ-preserving surgical operation - thromboembolectomy from a peripheral artery using a Fogarty balloon catheter or endarterectomy.
In case of ischemia of degrees IB–IIB, emergency intervention is necessary to restore blood flow: embolism or thrombectomy, bypass surgery. Prosthetic replacement of a segment of a peripheral artery is performed for short-term acute occlusions of the vessels of the extremities.
Ischemia of degrees IIIA–IIIB is an indication for emergency thrombus or embolectomy, bypass surgery, which must be supplemented with fasciotomy. Restoring blood circulation with limited contractures allows for delayed necrectomy or subsequent amputation at a lower level.
In case of ischemia and IIIB degree, vascular surgery is contraindicated, since restoration of blood flow can lead to the development of post-ischemic syndrome (similar to traumatic toxemia in the long-term crush syndrome) and the death of the patient. At this stage, amputation of the affected limb is performed. In the postoperative period, anticoagulant therapy is continued to prevent rethrombosis and re-embolism.
Treatment of varicose veins
To eliminate varicose veins, both conservative and surgical techniques are used. The patient is recommended to wear compression products (stockings, tights or knee socks) and periodically take medications to strengthen the walls of venous vessels (Troxevasin, Detralex, Cyclo 3 Fort, etc.). For local application, agents such as Lyoton, Curiosin, Venoruton, Heparin ointment, etc. are used. To normalize the condition of veins and blood flow, physiotherapy can be prescribed: amplipulse therapy, local darsonvalization, intermittent pneumocompression, magnetic therapy, hyperbaric oxygenation, laser therapy, balneo- and hydrotherapy.
As a minimally invasive technique for minor manifestations of varicose veins, sclerotherapy can be performed - the introduction of a sclerosant drug (for example, Fibro-Vein, Athoxysclerol, Sodium tetradecyl sulfate, Sclerowein, etc.) into the dilated areas of the veins, causing “gluing” of the pathologically dilated vessel. Other minimally invasive techniques can be used to remove varicose veins - ablation using laser or radiofrequency ablation. These procedures seem to seal the dilated vessels. In other cases, traditional surgical interventions are performed to remove veins, consisting of ligation or removal of the large and sometimes small saphenous veins. They are performed using different methods (stripping, miniphlebectomy, crossectomy) and can be supplemented with minimally invasive methods. The patient may also be prescribed some endoscopic types of interventions: endoscopic dissection and transluminal phlebectomy.
Prognosis and prevention
The most important prognostic criterion for acute occlusion of the vessels of the extremities is the time factor. Early surgery and intensive therapy can restore blood flow in 90% of cases. If treatment is started late or is absent, disability occurs due to the loss of a limb or death. With the development of reperfusion syndrome, death can occur from sepsis, renal failure, or multiple organ failure.
Prevention of acute vascular occlusion of the extremities involves timely elimination of potential sources of thromboembolism and prophylactic administration of antiplatelet agents.
1. Occlusive-stenotic lesions of blood vessels
Occlusive-stenotic vascular lesions
is a group of diseases characterized by impaired patency of the main arteries.
The etymology of vasoconstriction is different, and the location is found in different basins of the circulatory system. The result of such changes is a disruption of the blood supply to certain parts of the body or organs and, as a result, their functional failure.
A must read! Help with treatment and hospitalization!