Lipid metabolism disorders (dyslipidemia) affect the processes of absorption, transformation and metabolism of fats in the body. In addition to their energy function, fats are an important component of cell membranes, participate in the synthesis of hormones, transmit nerve impulses, and perform a host of other vital tasks. Therefore, a violation of lipid metabolism significantly affects the condition of the entire organism as a whole and can lead to the development of severe consequences.
Causes of dyslipidemia
- Nutritional – eating large amounts of animal and vegetable fats. The norm is set individually for each person, the average is from 0.8 to 1 g. fat per kilogram of body weight per day.
- Congenital disorders of lipid metabolism. They arise as a result of mutations in genes that are responsible for the processes of synthesis, breakdown, and transportation of fats. These mutations are passed on from generation to generation, so the disease can occur in young children for no apparent reason. Examples of genetic disorders of lipid metabolism are Gaucher disease, Tay-Sachs disease, and Niemann-Pick disease.
- Secondary disorders of lipid metabolism. Caused by other diseases that can affect the gastrointestinal tract, endocrine and enzyme systems, various internal organs (liver, kidneys).
Among the provoking factors that increase the risk of developing lipid metabolism disorders are bad habits (smoking, alcohol abuse), a sedentary lifestyle, excess weight, chronic stress, and taking hormonal medications.
Symptoms, causes, diagnosis and treatment of lipid metabolism disorders
The increase in the content of fat-like substances - lipids - in the blood is influenced by three main factors: excess intake of fat into the body from food, impaired excretion and increased synthesis in the body.
Depending on the mechanism of development of the disease, the causes of dyslipidemia are different.
Pathology can be:
- primary (due to hereditary factors);
- secondary (as a result of complications of any diseases);
- nutritional (if the human diet is oversaturated with animal fats).
An anomaly is often recognized after the fact, when problems with the cardiovascular system arise, since lipid metabolism disorders are most often asymptomatic. But in some patients, due to high levels of LDL, clouding of the cornea occurs, and xanthomas appear on the elbows and knees, and on the soles. With very high triglyceride levels (exceeding 11.3 mmol/l), pancreatitis develops and xanthomatous rashes are observed on the body.
Dyslipoproteinemia
Lipid metabolism is one of the most complex metabolisms in the human body. The importance of lipids in the body is great: they form the basis of the central nervous system, form the lipid matrix of cell membranes and cell organelles, and play an important role in energy metabolism. Some lipids are complex enzyme complexes that take part in immunological reactions, digestive processes, and blood clotting.
Until recently it was believed that lipid metabolic disorders were rare, but now we know that in industrialized countries with excess nutrition it is the most common factor in metabolic diseases.
The WHO classification of hyperlipoproteinemias, compiled on the basis of the Fredrickson classification, describes the entire spectrum of lipoproteins in the most common hyperlipidemias, but it does not divide the causes of disorders into genetically determined and secondary - in response to environmental factors or the underlying disease (Table 1).
Table 1. Classification of hyperlipoproteinemia
| Type | Plasma cholesterol | LDL cholesterol | Lipoprotein triglycerides | Violations | Clinical signs |
| I | Promoted | Increased or normal | Promoted | Excess chylomicrons | Abdominal pain Hepatomegaly Lipemic retinopathy Xanthomas |
| IIa | Increased or normal | Promoted | Fine | Excess LDL | Xanthomas Early atherosclerosis |
| IIb | Promoted | Promoted | Promoted | Excess LDL and VLDL | Xanthomas Xanthelasmas Early atherosclerosis |
| III | Promoted | Decreased or normal | Promoted | Excess chylomicron remnants and DILI | Obesity Common atherosclerosis Xanthomas |
| IV | Increased or normal | Fine | Promoted | Excess VLDL | Abdominal pain Vascular atherosclerosis |
| V | Promoted | Fine | Promoted | Excess chylomicrons and VLDL | Abdominal pain Pancreatic necrosis Obesity Xanthomas |
Type I hyperlipoproteinemia - hyperchylomicronemia (exogenous hyperlipemia; essential, fat-induced hypertriglyceridemia; Buerger-Grützsche disease) - is expressed in hypertriglyceridemia with an excess of chylomicrons and develops with lipoprotein lipase deficiency, caused by hereditary deficiency of lipoprotein lipase, deficiency of apoprotein C II. Enzyme deficiency leads to incomplete breakdown of chylomicrons and their accumulation in the bloodstream.
The disease is very rare and appears in childhood. The leading clinical symptoms are splenomegaly and recurrent abdominal pain, reminiscent of acute pancreatitis, eruptive xanthomas, lipemia in the retinal vessels. Plasma triglyceride levels rise to 50-100 mmol/l. After restricting dietary fats for 10-14 days, there is a progressive normalization of laboratory parameters and condition. The diagnosis is justified if the activity of lipoprotein lipase is less than 10% of its normal content. Differential diagnosis is made with hyperlipidemia type V. The prognosis is generally favorable, except for a predisposition to pancreatitis. The main focus of treatment is to reduce the formation of chylomicrons by limiting fat intake.
Type II hyperlipoproteinemia - familial hypercholesterolemia (multiple tuberous xanthoma) - is divided into two subtypes: IIa, IIb. In type IIa, the level of LDL cholesterol increases, and in type IIb, the picture is complemented by a moderate form of hypertriglyceridemia due to an increase in VLDL. The most severe form is homozygous hypercholesterolemia (frequency is 1:1,000,000), with plasma cholesterol levels reaching 12-25 mmol/l. In the heterozygous form, the frequency of which is 1:500, cholesterol levels range from 6-13 mmol/l. In the homozygous form, they are absent, and in the heterozygous form, the number of receptors for LDL is reduced. Normally, LDL binds to receptors, is absorbed by cells, is included in lysosomes, where proteins are destroyed, and the released cholesterol suppresses the activity of the main enzyme of cholesterol synthesis (HMG-CoA reductase). With receptor deficiency, the activity of this enzyme is not suppressed, which leads to increased cholesterol synthesis.
| Hyperlipidemias are diseases in which, as a result of impaired synthesis, transport and breakdown of lipoproteins, the level of cholesterol and/or triglycerides in the blood plasma increases. Since blood lipids, due to their insolubility in water, are transported only in the form of complexes with proteins, it is more correct to use the term “hyperlipoproteinemia” |
Clinical signs of the disease appear in the second - third - fourth decades of life and depend on the level of cholesterol in the plasma. The most typical clinical manifestations are cutaneous xanthomas, which are usually located on the skin of the extensor surfaces of the joints, in the buttocks, neck, and chin. Tendon xanthomas are common. Their primary localization is on the Achilles tendon, extensor tendons of the palms and feet. Ophthalmological changes are characterized by corneal lipemic arcs and periorbital xanthelasmas.
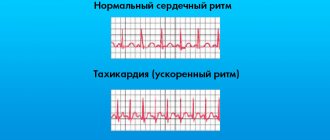
Changes in the cardiovascular system are determined by the development of coronary atherosclerosis: anginal pain appears. According to echocardiography, aortic stenosis and thickening of the aortic valve leaflets are detected. Angiography reveals uneven narrowing and funnel-shaped deformation of the proximal part of the coronary arteries. The progression of the atherosclerotic process contributes to the development of myocardial infarction. The prognosis for this form of hyperlipidemia depends on the degree of damage to the vascular bed by the atherosclerotic process. Treatment usually includes combination drug therapy and diet.
In type III hyperlipoproteinemia, the accumulation of chylomicron remnants and DILI leads to an increase in cholesterol and triglycerides. Lipid metabolism disorders in this type of hyperlipidemia are caused by a hereditary defect of apoprotein E, which is usually combined with obesity, diabetes mellitus, and hypothyroidism. The incidence of type III hyperlipoproteinemia is 1:5000. Clinical manifestations are noticed after 20 years. A distinctive feature is the high degree of damage to the entire vascular bed by the atherosclerotic process. Along with the symptoms of coronary heart disease, there are signs of peripheral vascular damage, often with symptoms of intermittent claudication, reminiscent of the symptoms of obliterating endarteritis. Characteristic is the presence of yellow or orange skin xanthoma localized on the palms, elbows, knees, buttocks and less commonly on the tendons. Patients often experience impaired carbohydrate tolerance: carbohydrate loading leads to a sharp increase in plasma triglyceride levels. Treatment comes down to eliminating any causes aggravating the disease (hypothyroidism, diabetes, obesity) and prescribing hypolipemic drugs.
An increase in triglyceride levels in blood serum taken from patients with type IV hyperlipidemia is due to the accumulation of VLDL, often accompanied by moderate hypercholesterolemia with normal LDL cholesterol. The incidence of this disease in the population is 0.2 - 0.3%. Clinical manifestations of combined familial hypertriglyceridemia are usually observed in adults and are characterized by atherosclerotic lesions of the coronary and peripheral vessels. It is possible to develop pancreatitis, manifested by attacks of abdominal pain and dyspeptic symptoms. For patients with hypertriglyceridemia, a typical feature of the fat layer of the face and neck area is the so-called “Louis Philippe face.” Skin manifestations - xanthomas - are rare. Most patients have impaired glucose tolerance. The main directions of treatment are to follow a modified fat diet aimed at normalizing body weight, limiting sugar and excess alcohol, and encouraging physical activity. If ineffective, drug therapy may be required.
The cause of severe triglyceridemia in type V hyperlipoproteinemia is an excess of both chylomicrons and VLDL. Unlike hyperlipoproteinemia type I, this disorder rarely manifests itself in childhood. The clinical manifestations of familial hypertriglyceridemia differ little from the clinical manifestations of type IV hyperlipoproteinemia. The disease also manifests itself in the second or third decade of life with obesity and the appearance of eruptive xanthomas. In the foreground is a more pronounced abdominal syndrome, which accompanies severe pancreatitis, up to the development of pancreatic necrosis. With this type of hyperlipoproteinemia, tolerance to both fats and carbohydrates is reduced.
Hyperlipoproteinemia type V is a secondary risk factor for the development of atherosclerosis due to the accumulation of VLDL.
Each of the hyperlipoproteinemia phenotypes can be either primary or secondary. Among the secondary causes of hyperlipoproteinemia, the most common are diabetes, hypothyroidism, inflammatory kidney diseases, and obesity (Table 2).
Table 2. Etiology of hyperliporotheidemia phenotypes
| Type | Primary causes | Secondary causes |
| I | Lipoprotein lipase deficiency Apo-C-II deficiency | Systemic lupus erythematosus (rare) |
| IIa | Familial hypercholesterolemia | Hypothyroidism |
| IIb | Familial combined hypercholesterolemia | Diabetes, nephrotic syndrome, anorexia nervosa |
| III | Familial hyperlipoproteinemia type III | Hypothyroidism, diabetes, obesity |
| IV | Combined familial hyperlipidemia, familial hypertriglyceridemia | Diabetes, chronic kidney disease |
| V | Familial hypertriglyceridemia | Alcohol, diuretics, contraceptives |
The five types of hyperlipoproteinemia mentioned do not exhaust the entire variety of lipid metabolism disorders. First of all, this concerns this fairly common form of disorder, which is characterized by a decrease in HDL cholesterol. In this case, there is no hyperlipoproteinemia as such; a decrease in the level of total cholesterol may even be observed, however, an atherogenic shift can be determined in the lipid composition of the blood. To characterize the atherogenic direction of the lipid spectrum, the atherogenic index is calculated, which is equal to the ratio of the cholesterol content in LDL and VLDL to its content in HDL. Normally, it should not exceed 4.0 (in children - 2.0). Thus, the term hyperlipoproteinemia is not all-encompassing to characterize shifts in lipid composition, so it is more correct to use the term dyslipidemia (dyslipoproteinemia).
The variety of types of dyslipoproteinemia and their clinical manifestations indicates that disruption of lipid homeostasis can occur at any level; therefore, there cannot be a standard approach to the treatment of this category of patients. It is necessary to individualize the correction of dyslipoproteinemia depending on the type of lipid metabolism disorder and the clinical course. The goal of treatment is to minimize the risk of developing vascular atherosclerosis, coronary heart disease and pancreatitis.
Treatment of hyperlipidemia always begins with diet. The basic principles of a lipid-lowering diet are: weight loss if it is excess; the total calorie content of the diet is provided by 55% carbohydrates, 10-15% proteins and up to 30% fats, including 10% saturated, monounsaturated and polyunsaturated fatty acids, cholesterol less than 300 mg/day and 35 mg/day fiber, obtained mainly in the form legumes, as well as other vegetables and fruits. If the standard diet is ineffective, then fat intake should be reduced to 20-25%, and cholesterol to 150 mg/day or less.
Healthy foods contain mostly plant fats rather than animal fats. Many animal fats contain large amounts of cholesterol. For example, the yolk of a chicken egg contains up to 300 mg of cholesterol, i.e., the daily need for cholesterol is completely covered after eating one egg. In addition, animal fats contain saturated fatty acids. Vegetable fats contain predominantly unsaturated fatty acids, which are actively involved in cholesterol metabolism in the body. It is advisable to eat fats consisting of 2/3 vegetable and only 1/3 animal fats. Vegetable fats retain their beneficial qualities if they have not been subjected to heat treatment. In general, eating fried foods is not recommended. As for proteins, it is advisable to use less fatty meats (lamb and pork), it is better to cook from lean beef, and give preference to boiling. A special place in the diet should be given to fish. Studies conducted among the Canadian Eskimo population showed an almost complete absence of atherosclerosis. The basis of their diet is fish and fish oil, rich in polyunsaturated fatty acids. You should more often include plant proteins in your diet - mushrooms, nuts, legumes. Regarding carbohydrates, it should be said that the consumption of sugar, confectionery, and sweets containing simple sugars must be limited, and preference should be given to products that contain polysaccharides (brown bread, carrots, fruits). This is especially true for people with increased body weight and impaired glucose tolerance. Low-fat dairy products are very useful, especially kefir, yogurt, and cottage cheese. Coarse plant fiber, which is found in some vegetables (cabbage, lettuce, carrots) and fruits (apples, pears, grapefruits), partially adsorbs cholesterol and TG and prevents the absorption of dietary fats. Therefore, their inclusion in the diet of patients with hyperlipidemia is justified.
Some patients with hyperlipidemia do not respond adequately to diet and correction of other causative factors. In such cases, drug treatment is required, but with the obligatory continuation of diet. Pharmacotherapy for dyslipoproteinemia is quite complex and varied. Based on the principle of action, all lipid-lowering drugs can be divided into the following main groups.
- Drugs that prevent the absorption of lipids in the intestine - these include bile acid sequestrants (anion exchange resins - cholestyramine, colestipol; nonspecific enterosorbents, specific cholesterol enterosorbents).
- Drugs that enhance the catabolism of triglycerides - fibrates (clofibrate, bezafibrate, gemfibrozil, ciprofibrate, fenofibrate).
- Drugs that suppress cholesterol synthesis - HMG-CoA reductase inhibitors (simvastatin, pravastatin, lovastatin, fluvastatin, atorvastatin, icerivastatin).
- Drugs that reduce the production of LDL and VLDL are nicotinic acid derivatives (nicofuranose, acipimox, enduracin) and drugs based on omega-3-polyunsaturated fatty acids (fish oil, maxepa, eikonol, polyene).
If conservative therapy is ineffective, patients with high hypercholesterolemia are shown surgical methods for correcting dyslipoproteinemia, in particular LDL apheresis through columns with mono- and polyclonal antibodies to LDL and cascade plasma filtration through columns with heparin. WHO recommendations for the treatment of dyslipoproteinemia identify five observation groups.
Group A includes individuals with moderate hypercholesterolemia: serum cholesterol 200 - 250 mg/dl (5.2 - 6.5 mmol/l), triglycerides less than 200 mg/dl (<2.3 mmol/l). Diet alone is quite effective; drug therapy is rarely necessary.
Group B includes individuals with cholesterol levels of 250 - 300 mg/dL (6.5 - 7.8 mmol/L). If a carefully followed diet does not produce satisfactory results, drug treatment, usually small doses of bile acid sequestrants, should be considered.
Group C includes individuals with hypertriglyceridemia: (serum cholesterol less than 200 mg/dL (<5.2 mmol/L), triglycerides 200 - 500 mg/dL (2.3 - 5.6 mmol/L). Many of them have HDL cholesterol levels are also low. Treatment mainly consists of losing excess weight and reducing alcohol consumption. A lipid-lowering diet is prescribed. Drug treatment is not usually used, but may be considered if high triglyceride levels are associated with familial combined hyperlipidemia or the presence of other high-risk factors for developing atherosclerosis.
Group D includes individuals with elevated serum levels of cholesterol: 200-300 mg/dl (5.2 - 7.8 mmol/l) and triglycerides: 200 - 500 mg/dl (2.3 - 5.6 mmol/l ). Such patients may have combined hyperlipidemia, the diagnosis of which includes family evaluation. Although the increase in lipid levels is mild, this disorder is associated with an increased risk of CAD. Treatment consists of losing excess weight and adopting a lipid-lowering diet. For a small number of patients, drug treatment along with diet is required. Sometimes combination drug therapy is necessary.
Group E includes individuals with severe hyperlipidemia (cholesterol levels greater than 300 mg/dL (>7.8 mmol/L), and/or triglycerides greater than 500 mg/dL (>5.6 mmol/L). Patients with cholesterol levels greater than 300 mg/dL (>7.8 mmol/L) and with normal triglycerides usually have familial hypercholesterolemia and a particularly high risk of CAD. Therapy usually includes diet and one or two lipid-lowering drugs: a bile acid sequestrant in combination with one of the fibrates (or inhibitors cholesterol synthesis) or with nicotinic acid. There is no suitable drug therapy for chylomicronemia; it is treated with a low-fat diet. Remnant hyperlipidemia (type III) usually manifests as a significant increase in both cholesterol and triglycerides. It is very often associated with coronary and peripheral atherosclerosis, most cases require treatment with diet and medications, usually fibrates.Family hypertriglyceridemia, like chylomicronemia, can lead to acute pancreatitis. It is often accompanied by diabetes. Treatment requires: body weight control, diet, and in severe cases, fibrates or nicotinic acid.
One of the most important aspects of medicine is prevention. It is more correct to start it at an early age, when there are no signs of dyslipoproteinemia. This type of prevention is called primary, in contrast to secondary, in which preventive measures are carried out for existing signs of atherosclerosis. The goal of primary prevention is to prevent the development of the disease; secondary prevention is aimed at stabilizing the condition and preventing serious complications. The basis of preventive measures is the formation of a healthy lifestyle, quitting smoking, excessive alcohol consumption, and introducing the principles of a rational diet. The fight against excess weight and a sedentary lifestyle is of no small importance. A decisive role is given to measures to normalize blood pressure, sugar levels and the content of blood lipid fractions. Primary prevention of hyperlipoproteinemia and related diseases is carried out among children whose parents have lipid metabolism disorders and early signs of coronary atherosclerosis. Mass preventive measures should and can be of great benefit when carried out in childhood and adolescence.
How to determine the phenotype of hyperlipoproteinemia?
To determine the phenotype of hyperlipoproteinemia, it is necessary to know the concentrations of triglycerides, total cholesterol and low-density lipoprotein cholesterol (LDL). In addition, the presence of chylomicrons or very low-density lipoproteins (VLDL) should be assessed. Because plasma lipid levels have significant biological variation between days, diagnosis of elevated lipid levels should be based on two tests taken two to three weeks apart. Measuring total and high-density lipoprotein (HDL) cholesterol levels does not require prior fasting. Triglycerides are typically measured in plasma or serum samples 12 hours after the last meal, usually in the morning; It is allowed to take water or other liquids that do not contain fats. Studies should be carried out no earlier than three to four weeks after a major operation or myocardial infarction. Most laboratories calculate LDL cholesterol levels from total cholesterol, triglycerides, and HDL cholesterol. This calculation is usually carried out using the Friedwald formula:
LDL cholesterol (mg/dl) = TC - triglycerides/5 - HDL cholesterol LDL cholesterol (mmol/l) = TC - triglycerides/2.2 - HDL cholesterol
This formula is valid for triglyceride values <500 mg/dL (5.5 mmol/L). In specialized laboratories, the level of LDL cholesterol can be measured directly by ultracentrifugation and electrophoresis.
According to European recommendations, a cholesterol level of 5.2 mmol/l (200 mg/dl) is considered normal, 5.2 - 6.5 mmol/l (200-250 mg/dl) - mild hypercholesterolemia, 6.5-7.8 mmol /l (250-300 mg/dl) - moderate, and a level >7.8 mmol/l (>300 mg/dl) - severe hypercholesterolemia. Triglyceride levels above 2.0 mmol/L for men and 1.5 mmol/L for women require correction. The risk of developing vascular atherosclerosis increases with LDL cholesterol >4.2 mmol/l (164 mg/dl), HDL cholesterol <1.0 mmol/l (39 mg/dl).
Classification of lipid metabolism disorders
Today, the Fredrickson classification of dyslipidemias is considered the main one:
- The cause of type 1 dyslipidemia is enzyme deficiency. Violations of this type are quite rare.
- Dyslipidemia 2a occurs due to mutations in genes and is one of the most common types of lipid metabolism disorders.
- Dyslipidemia 2b also occurs quite often and can be either hereditary or combined (the cause may be previous diseases and a diet oversaturated with animal fats).
- Type 3 lipid metabolism disorders are characterized by an increase in triglycerides and LDL in the blood.
- Type 4 hyperlipidemia, characterized by an increase in VLDL, is of endogenous origin.
- Dyslipidemia type 5 occurs when the level of cholinomicrons in the blood increases and also refers to hereditary disorders.
Oligosaccharide and glucoprotein dysmetabolism
53. Cellular inclusion disease. Glycoprotein enzymes, N-acetylglucosaminylphosphotransferase, are affected. Severe mental retardation, and in somatic terms - hepatomegaly, disorders of the skeletal system, swelling of the gums. Prenatal diagnosis is possible. The type of inheritance is autosomal recessive.
54. Mannosidosis. The enzyme mannosidase is affected. Severe mental retardation. Somatically: hepatomegaly, disorders of the skeletal system, roughening of the face. Prenatal diagnosis is possible. The type of inheritance is autosomal recessive.
55. Fucosidosis. The enzyme fucosidase is affected. Marked mental retardation. Somatically (see paragraph 56). Prenatal diagnosis is possible. The type of inheritance is autosomal recessive.
Diagnostic measures
Diagnostic procedures include a consultation with a physician, physical examination, medical history, and blood chemistry tests.
During a physical examination, the doctor notes the possible presence of xanthelasma, xanthomas, and lipoid arch of the cornea. Patients often experience high blood pressure. Auscultation (listening) and percussion (tapping) are not informative, since they are not accompanied by changes in dyslipidemia.
To identify inflammation and concomitant diseases, a laboratory test of blood and urine is prescribed. Genetic analysis identifies genes that carry hereditary information and are responsible for the development of type 2 dyslipidemia.
A biochemical blood test allows you to determine the level of total blood protein and sugar, uric acid and creatinine to detect concomitant organ damage. Immunological analysis determines the content of antibodies to cytomegalovirus and chlamydia, as well as the level of C-reactive protein.
But the main method for diagnosing dyslipidemia is a lipidogram - a blood test for fat-like substances, lipids. When measuring the lipid spectrum
The levels of triglycerides, total cholesterol, LDL and HDL are determined.
The studies are carried out on an empty stomach, in NEARMEDIC's own laboratory.
Treatment of dyslipidemia is prescribed after a complete diagnosis, accurate diagnosis and determination of the cause of the pathology.
Mucopolysaccharidoses
A group of hereditary connective tissue diseases characterized by combined damage to the musculoskeletal system, internal organs, eyes and nervous system. Increased excretion of mucopolysaccharides in the urine and their accumulation in various organs and tissues. There are nine types of the disease. Here are some of them.
47. MSSI syndrome. The enzyme iduronidase is affected. Mental retardation is pronounced. Prenatal diagnosis is possible. Various somatic anomalies are detected. The type of hereditary transmission is autosomal recessive.
Diseases 48–52 are characterized by similar somatic disorders: varying degrees of bone damage, hepatosplenomegaly, limited joint mobility, etc.
48. Gunther's disease II. The enzyme iduronate sulfase is affected. Mental retardation is pronounced. Somatic abnormalities are observed. Prenatal diagnosis is possible. The type of hereditary transmission is recessive, linked to chromosome X.
49. Sanfilippo III syndrome. Mental retardation is combined with such anomalies as thickening of the skull bones, enlarged liver, and deformation of the lumbar vertebrae. Prenatal diagnosis is possible. The type of hereditary transmission is autosomal recessive. Various enzymes are affected (phosphatases types A-D).
50. Morquio's disease IV. The enzyme N-acetylgalactosamine is affected. There are no data on mental retardation. Prenatal diagnosis is possible. The type of inheritance is autosomal recessive.
51. Maroteaux-Lami disease IV. The enzyme arylsulfatase B is affected. Mental retardation does not always occur. Prenatal diagnosis is possible. The type of inheritance is autosomal recessive.
52. Gargoilism (the name comes from the images of chimeras that decorated ancient drainpipes). Other names: Gurler disease, Johnny McL disease. (name of the first patient), multiple dazostosis, Pfaundler's disease. The main symptoms are: cognitive deficit, chondroosteodystrophy, hepatosplenomegaly, corneal opacification. A large head, an ugly structure of the facial part of the skull, dwarf stature, and increasing blindness are typical. The type of hereditary transmission is autosomal recessive. Prenatal diagnosis of the disease is possible.
Treatment of dyslipidemia
Treatment of dyslipidemia is complex and includes:
- Drug therapy - fibrates, vitamins, statins and other drugs that correct lipid metabolism disorders;
- Non-drug treatment - weight normalization through fractional meals, dosed physical activity, limiting alcohol and smoking, and stressful situations.
- Diet therapy - foods rich in dietary fiber and vitamins are recommended (vegetables, cereals, fruits, beans, low-fat lactic acid products); fatty and fried meats are not allowed.
If lipid imbalance is a secondary pathology resulting from exposure to negative factors or any disease, NEARMEDIC cardiologists prescribe therapy aimed at timely detection and treatment of the underlying disease.
Dyslipidemia develops over years and requires equally long-term treatment. You can prevent further disturbances in lipid metabolism by strictly following the recommendations of doctors: move more, watch your weight, quit bad habits.
Contact your doctors on time!
In the early stages, stopping the pathological process is much easier. Timely therapy, elimination of risk factors and disciplined implementation of doctors’ recommendations significantly prolong and improve the lives of patients
Contact our clinics, do not delay your visit to the doctor. You will be consulted by experienced doctors, and you will undergo an expert examination using high-tech diagnostic equipment. Based on the results obtained, the cardiologist will prescribe competent treatment for dyslipidemia and recommend preventive measures.
To make an appointment with a cardiologist, call or fill out a request on the website.
Our clinics in St. Petersburg
Structural subdivision of Polikarpov Alley Polikarpov 6k2 Primorsky district
- Pionerskaya
- Specific
- Commandant's
Structural subdivision of Zhukov Marshal Zhukov Ave. 28k2 Kirovsky district
- Avtovo
- Avenue of Veterans
- Leninsky Prospekt
Structural subdivision Devyatkino Okhtinskaya alley 18 Vsevolozhsk district
- Devyatkino
- Civil Prospect
- Academic
For detailed information and to make an appointment, you can call +7 (812) 640-55-25
Make an appointment
There are 5 types of lipoproteins:
- Chylomicrons are synthesized by intestinal cells, after which they enter the lymphatic vessels and then into the blood. They are a transport form of triglycerides, cholesterol and exogenous fatty acids.
- Very low density lipoproteins . They are formed in the liver and contain up to 15 percent of total cholesterol. Very low density lipoproteins can be transformed into small particles, most of which are excreted in the liver.
- Intermediate density lipoproteins are an intermediate phase of very low density lipoproteins.
- Low-density lipoproteins (LDL) contain 60-70% cholesterol and are considered the main carriers of cholesterol to tissues. The role of low-density lipoproteins has been most studied in the process of atherogenesis. It produces smaller and denser particles. This type of disorder often occurs in diabetes mellitus.
- High-density lipoproteins (HDL) contain about 20-30% cholesterol. They play a very important role in the reverse transport of cholesterol from tissues to the liver. Experts have established a connection between a decrease in the concentration of HDL in the blood and the risk of coronary heart disease.