It is customary to talk about lipid metabolism disorders in the body if there is an imbalance between the levels of high- and low-density lipoprotein cholesterol, as well as triglycerides. This causes many health problems and leads to the development of serious diseases, including cardiovascular disasters - myocardial infarction and stroke.
The head of the Department of Cardiology and Rheumatology of BelMAPO, Doctor of Medical Sciences, Professor Andrey Pristrom told the journalist of the information portal “Healthy People” about the causes of lipid metabolism disorders, what it entails and how to diagnose the pathology .
Why is cholesterol needed?
Cholesterol is necessary for our body for the functioning of organs and systems. It is part of cell membranes, ensures their strength, participates in the synthesis of sex hormones (androgens and estrogens), as well as those hormones produced by the adrenal glands (cortisol) and in the ovaries (estradiol). Cholesterol plays an important role in the metabolism of fat-soluble vitamins (A, D, E and K). Approximately three-quarters of cholesterol is synthesized in the body and only a quarter comes from food.
Lipoproteins, which are divided into:
- Very low-density lipoproteins (VLDL), which are produced in the liver, contain lipids (triglycerides and cholesterol). They are transported through the blood to the tissues;
- low-density lipoproteins (LDL) are formed from VLDL due to the release of triglycerides from them, contain mainly cholesterol, which is delivered from the liver to the body tissues;
- High-density lipoproteins (HDL) transport unused cholesterol from tissues to the liver, where it is synthesized into bile acids.
Andrey Pristrom: “Lipid metabolism disorders occur due to a breakdown in the mechanism for regulating cholesterol levels. What does it mean? When cholesterol rises, mechanisms must be activated that reduce its formation, and vice versa. There are many reasons that can lead to such an “imbalance.” It’s almost impossible to say unequivocally what exactly triggered the failure.”
Symptoms of metabolic syndrome
When diagnosing MS, 4 parameters are distinguished:
- hypertension (high blood pressure);
- high blood sugar;
- obesity (waist circumference more than 102 cm in men and more than 88 cm in women);
- abnormal cholesterol levels (decreased high-density lipoprotein levels and/or increased triglyceride levels).
Each of these conditions is dangerous individually, but together they trigger a cascade of pathological processes and turn into a mortal threat to blood vessels and human life and health in general.
Doctors nicknamed this complex of diseases the “deadly quartet.” In fact, metabolic syndrome is not an independent disease. This is a group of symptoms that often occur together and increase the risk of other - even more severe - disorders.
Reasons for the development of lipid metabolism disorders
Lipid metabolism disorders can be either hereditary or acquired. Among hereditary forms, homozygous and heterozygous disorders are distinguished. The key point in these forms is excessively high levels of low-density lipoprotein cholesterol. This leads to atherosclerotic vascular damage already in childhood and the development of heart and vascular diseases in the second or third decade of life.
Andrey Pristrom: “Persons with homozygous hypercholesterolemia have a very high likelihood of developing cardiovascular accidents (heart attacks and strokes) at 20–30 years of age, and sometimes younger. However, such disorders, compared to heterozygous forms, are quite rare: approximately 1 case per 200–300 thousand population.”
Acquired lipid metabolism disorders are most often diagnosed. Among the risk factors:
- smoking is the most significant risk factor. Smoking damages the vascular endothelium and triggers the development of all disorders. This applies to both active, including electronic devices for tobacco consumption, and passive smoking;
- consumption of large quantities of foods high in saturated fats: red meat, sausages, sausages, hard cheeses, pastries and baked goods;
- obesity;
- inactive lifestyle;
- the presence of concomitant diseases (diabetes mellitus, liver and kidney diseases, arterial hypertension, decreased thyroid function);
- chronic stress;
- age.
Men with lipid metabolism disorders are more likely than women to develop cardiovascular diseases. However, after menopause in women, this indicator levels off in both sexes.
Andrey Pristrom: “More than a third of the male population of our country aged 18 to 44 years have more than 3 risk factors for the development of cardiovascular accidents.
Most often these are smoking, obesity, hypertension and high cholesterol.”
Treatment of dyslipidemia
Treatment of dyslipidemia is complex and includes:
- Drug therapy - fibrates, vitamins, statins and other drugs that correct lipid metabolism disorders;
- Non-drug treatment - weight normalization through fractional meals, dosed physical activity, limiting alcohol and smoking, and stressful situations.
- Diet therapy - foods rich in dietary fiber and vitamins are recommended (vegetables, cereals, fruits, beans, low-fat lactic acid products); fatty and fried meats are not allowed.
If lipid imbalance is a secondary pathology resulting from exposure to negative factors or any disease, NEARMEDIC cardiologists prescribe therapy aimed at timely detection and treatment of the underlying disease.
Dyslipidemia develops over years and requires equally long-term treatment. You can prevent further disturbances in lipid metabolism by strictly following the recommendations of doctors: move more, watch your weight, quit bad habits.
Contact your doctors on time!
In the early stages, stopping the pathological process is much easier. Timely therapy, elimination of risk factors and disciplined implementation of doctors’ recommendations significantly prolong and improve the lives of patients
Contact our clinics, do not delay your visit to the doctor. You will be consulted by experienced doctors, and you will undergo an expert examination using high-tech diagnostic equipment. Based on the results obtained, the cardiologist will prescribe competent treatment for dyslipidemia and recommend preventive measures.
To make an appointment with a cardiologist, call or fill out a request on the website.
Diagnostics (lipid profile)
The main method for diagnosing lipid metabolism disorders is the determination of 4 main indicators of lipid metabolism in venous blood (total cholesterol, low and high density lipoproteins, triglycerides), which is called a lipid profile. To make a diagnosis, such an analysis is performed at least twice, one to several weeks apart. Blood is taken on an empty stomach, and it is recommended to avoid a heavy dinner the night before.
If a person is healthy and does not have cardiovascular diseases, diabetes mellitus or serious kidney disorders, the main indicator is total cholesterol. The norm is less than 5 mmol/l.
In the presence of pathologies of the heart and blood vessels, as well as a high risk of their development (determined by the cardiovascular risk scale - SCORE), another control criterion is used: low-density lipoprotein cholesterol.
The target depends directly on the level of risk:
- for low-risk patients – less than 3 mmol/l;
- for patients with moderate risk – less than 2.6 mmol/l;
- for high-risk patients – less than 1.8 mmol/l;
- for patients with a very high risk level - less than 1.4 mmol/l.
The risk of developing cardiovascular accidents is considered high with a score of 5 or more on the SCORE scale.
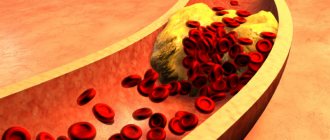
Elevated levels of LDL cholesterol can cause lipid deposits in the walls of blood vessels, usually in the arteries. It is LDL cholesterol that leads to the appearance of atherosclerotic plaques, which narrow the lumen of blood vessels or completely clog them, thereby blocking the flow of blood.
Andrey Pristrom: “In people with a severe lipid profile disorder, it is also recommended to perform an ultrasound of the brachiocephalic arteries in order to identify atherosclerotic plaques. Atherosclerosis, which develops against the background of lipid metabolism disorders, is a systemic process. If there are changes in the brachiocephalic arteries, then they will be in other vessels.”
The consequences of atherosclerosis are very severe. This is the development of myocardial infarction, stroke, chronic coronary heart disease, occlusion of peripheral arteries, which can lead to amputation of the lower extremities.
Hereditary hypercholesterolemia can be suspected by a blood test: the level of low-density lipoprotein cholesterol will be above 5 mmol/l. In addition, in such people, yellow formations (xanthomas) and white cloudy stripes on the cornea can be seen on the eyelids. Another sign of a hereditary form of lipid metabolism disorders is the appearance of growths on the extensor tendons of the fingers and in the area of the Achilles tendon. In such cases, genetic testing is recommended to confirm or refute hereditary hypercholesterolemia.
The frequency of studies depends on the presence of a risk of cardiovascular accidents. If the risk is low, a blood lipid profile should be performed approximately once every five years; if the risk is high, once a year. However, after 40 years, it is advisable to do a blood test for cholesterol levels annually.
Alarming trends
Until recently, metabolic syndrome primarily affected older people (over 60 years of age).
The picture has changed significantly over the past 20 years. The dynamics have shown that this problem is getting younger and becoming relevant for the younger population. In some countries, the proportion of adults suffering from these symptoms reaches 25%. Metabolic syndrome has another name - “new world syndrome”. The fact is that mainly people who lead a sedentary lifestyle (and this applies to the majority of residents of large cities) and consume large amounts of fast carbohydrates and trans fats suffer from obesity and related pathologies. As a result, there is a worldwide surge in cardiovascular disease and diabetes.
Metabolic syndrome affects both developed countries (where high-tech production has eliminated the need for the population to move a lot) and developing countries (a large percentage of the population of which has to save on food and consume more fast carbohydrates - pasta, bread, potatoes, corn).
There is another trend in recent years. Women of reproductive age began to suffer from metabolic syndrome. What this is connected with is not entirely clear. Presumably, oral contraceptives may have a negative effect.
Just imagine: over the past 20 years, the number of people with metabolic syndrome in the world has increased by more than 100 million - that is, by a third.
The problem of childhood obesity, and with it childhood MS, is especially acute. Scientists link the increase in childhood obesity to frequent refusal of breastfeeding. Breastfeeding eliminates early introduction of complementary foods, which can lead to unhealthy weight gain. Protein and total energy intakes are higher in formula-fed infants, leading to increased infant weight. Formula feeding also slightly increases insulin levels, which in turn promotes fat deposition and the early development of fat cells (adipocytes).
Thus, rapid weight gain in infancy is associated with childhood obesity. Breastfeeding can help program a person to maintain a healthy weight as an adult.
Risk factors
- Elderly age. The older a person is, the higher the risk of developing metabolic syndrome, according to statistics.
- Ethnicity. Hispanics are at greatest risk for developing metabolic syndrome. But this does not mean that Russians do not suffer from this disease.
- Obesity. As already mentioned at the beginning, excess weight increases the chances of developing MS.
- Diabetes. The likelihood of developing metabolic syndrome increases if the patient had diabetes during pregnancy (gestational diabetes). A family history of type 2 diabetes is also a reason for close attention to your health.
- Other diseases. The risk of metabolic syndrome is higher if the patient has had fatty liver disease, polycystic ovary syndrome, or sleep apnea.
Recommendations
Following a healthy lifestyle can prevent conditions that cause metabolic syndrome. A healthy lifestyle means a set of simple habits:
- Physical activity for at least half an hour every day.
- A balanced diet with plenty of vegetables, fruits, and enough protein.
- Reduce the amount of salt and saturated fat in the diet.
- Maintaining a healthy weight.
- Quitting smoking and alcohol.
Author:
Baktyshev Alexey Ilyich, General Practitioner (family doctor), Ultrasound Doctor, Chief Physician
What are the reasons?
The main reason why metabolic syndrome develops is external factors: poor nutrition, low mobility.
These bad habits ultimately disrupt the normal functioning of adipose tissue and lead to insulin resistance. Metabolic syndrome has a hereditary predisposition, which, however, is also largely explained by external factors. People who grow up in the same family are more likely to have similar eating habits and attitudes toward exercise. If there is a huge amount of fast carbohydrates and fats on the parent’s table and few vegetables, herbs and fruits, the child develops an unhealthy relationship with food from childhood. It's the same with sports: a child is more likely to be active if he has active parents.
Classification
Hyperlipidemia is divided into:
- Primary (genetically predisposed and hereditary).
- Secondary (symptom of diseases associated with metabolic disorders).
Secondary ones are divided into:
- Basal (detected during fasting examination and indicate serious disorders of fat metabolism).
- Induced (detected after taking excess amounts of fats or carbohydrates, hormonal drugs or after physical activity). For the most part, these are nutritional hyperlipidemias . Secondary dyslipoproteinemia is characterized by elevated levels of several classes of lipoproteins.
According to the classification of D. Fredrickson, there are several types of lipid metabolism disorders, depending on the ratio of different lipoproteins.
- Type I This is a fairly rare type that develops when there is a deficiency of the enzyme lipoprotein lipase or the protein that activates lipoprotein lipase . This type is manifested by an increase in the level of chylomicrons.
- II type . Hyperlipoproteinemia type 2 is the most common type of lipid metabolism disorder. This type is characterized by an increase in LDL cholesterol. This type is subdivided into types IIa and IIb. Type IIa is characterized by increased total cholesterol and LDL cholesterol. In type IIb, all fractions are elevated, including triglycerides. The frequency of occurrence of the latter type is 10%, found in metabolic syndrome). Statins, fibrates (for very high triglyceride levels), as well as a combination of these two groups of drugs are prescribed for treatment. ω3-fatty acids are also used.
- III type . This type is manifested by an increase in the level of chylomicrons and intermediate density lipids. The occurrence does not exceed 0.02%.
- IV type . This type is characterized by an increase in triglycerides. The occurrence reaches 1%.
- V type . Manifested by high levels of chylomicrons and VLDL.
In clinical practice, lipid metabolism disorders of types II and IV are important, the rest are very rare. In the prevention of atherosclerosis, the main thing is the correction of disorders that can be influenced and are associated with nutrition, lifestyle and obesity .
What is metabolism
Metabolism is a set of chemical reactions in the human body that break down food and convert it into energy. Special enzymes take part in metabolism, which speed up the process of digesting food and absorbing nutrients.
There are 3 types of metabolic disorders that can occur in the body:
- Protein metabolism disorder. A person constantly feels hungry, is in an irritated and restless state, and becomes depressed. In this case, a protein diet will help.
- Disturbance of carbohydrate metabolism. A person cannot live a day without coffee, is indifferent to sweets, and has no appetite. The opposite picture may be observed - a person constantly eats sweets, snacks on sweets and cakes. A carbohydrate diet under the supervision of a specialist is necessary.
- Combined. With such a metabolism, a person constantly feels weak, drowsy, anxious, cannot live without sweets and is prone to obesity.
Diet
Diet for vascular atherosclerosis
- Efficacy: therapeutic effect after 2 months
- Dates: no data
- Cost of products: 1700-1800 rubles. in Week
DASH Diet
- Efficacy: therapeutic effect after 21 days
- Timing: constantly
- Cost of products: 1700-1800 rubles. in Week
Patients are prescribed a diet low in fat, simple carbohydrates and an increased intake of dietary fiber up to 40 g. In the diet of patients, the amount of unsweetened fruits and vegetables with a low starch content, vegetable oils, beans, nuts, chickpeas, soybeans, fish, whole grain products, low-fat yoghurts At the same time, red meat, processed meats and salt are reduced. The traditional diet for hypercholesterolemia is the DASH and Mediterranean . These diets are effective in reducing cardiovascular disease factors. The Mediterranean diet includes olive oil or nuts.
When following this diet, there is a 30% decrease in cardiovascular diseases. Canola, flax, corn, olive and soybean oils reduce LDL cholesterol levels.
The main points of nutrition for patients are:
- Avoiding consumption of trans fats.
- Limiting saturated fats (only 7% of them are allowed in the diet).
- Limiting the intake of cholesterol from food (less than 300 mg/day - one chicken egg covers the need for cholesterol).
- Reducing the amount of carbohydrates, it is advisable to completely eliminate simple carbohydrates from the diet. Carbohydrates have a neutral effect on low-density lipoproteins, but excessive consumption of highly refined carbohydrates indirectly (via insulin) adversely affects triglycerides and low-density lipoproteins.
- Reduce consumption of foods with cholesterol.
- Increase in dietary fiber, which has a hypolipidemic effect. Soluble dietary fiber, which is found in fruits, vegetables, legumes, and whole grain cereals, is effective in this regard. Coarse plant fiber (cabbage, lettuce, carrots, grapefruits, apples, pears) partially adsorbs cholesterol and also prevents the absorption of fats.
- Eating foods rich in phytosterols . Regular consumption of such foods reduces cholesterol levels by 10%. Phytosterols are found in corn, soybeans, lentils, peas, vegetable oils, beans, whole grains, pumpkin seeds, sesame seeds, pistachios, and walnuts.
- Consuming omega-3 PUFAs.
What processes does lipid metabolism involve?
Lipid metabolism goes through a certain sequence of stages:
- digestion of fats entering the digestive tract;
- connection with transport proteins and absorption into the blood plasma;
- synthesis of own lipids and similar binding to proteins;
- transport of fat-protein complexes to organs through blood and lymphatic lines;
- metabolism in the blood and inside cells;
- transport of breakdown products to excretory organs;
- removal of end products of metabolism.
The biochemistry of all these processes is very complex, but the main thing is to understand the essence of what is happening. To describe them briefly, lipid metabolism looks like this: having connected with carriers, lipoproteins travel to their destination, are fixed on cell receptors specific to them, and release the necessary fats, thereby increasing their density.
Next, most of the “impoverished” compounds return to the liver, are converted into bile acids and excreted into the intestines. To a lesser extent, the products of lipid metabolism are pushed directly from the cells of the kidneys and lungs into the external environment.
Considering the presented scheme of fat metabolism, the dominant role of the liver in it becomes clear.
Expert opinions - discussion of issues of diagnosis, treatment and prevention of hypercholesterolemia
Experts discuss the diagnosis, treatment and prevention of hypercholesterolemia:
A. V. Pogozheva Leading Researcher, Doctor of Medical Sciences, Professor of the Federal State Budgetary Institution “Federal Research Center for Nutrition and Biotechnology”, Moscow
Yu. V. Abakumova , Doctor of Medical Sciences, Professor, Chairman of the Saratov Regional Branch of the Academy of Medical and Technical Sciences of the Russian Federation.
Table of contents:
Diagnosis of lipid metabolism disorders
Table 1. Criteria for diagnosing lipid metabolism disorders
The role of cholesterol
Liver and cholesterol
Where is cholesterol spent in the body?
Why do doctors keep trying to link hyperlipidemia and atherosclerosis?
Should hyperlipidemia be treated?
Healthy fats
Principles of healthy eating
Expert A.V. Pogozheva, Doctor of Medical Sciences, Professor of the Federal State Budgetary Institution “Research Institute of Nutrition” of the Russian Academy of Medical Sciences, Moscow:
A progressive and continuous relationship between mortality from coronary heart disease and serum cholesterol concentrations is considered to be proven. According to WHO, an elevated level (more than 5.0 mmol/l) of cholesterol in the blood serum - hypercholesterolemia (HCS) - is a risk factor for premature mortality in 23% of cases and causes 12.4% of lost years of healthy life among Russian residents.
GCS is divided into primary and secondary. Primary HCS is associated with a genetic disorder of cholesterol synthesis in the liver and is inherited (homo- or heterozygous type). Secondary hypercholesterolemia is associated with diseases of other organs and systems (for example, diseases of the biliary system).
A positive correlation has been established between serum cholesterol levels and mortality from cardiovascular diseases (CVD), on the one hand, and excess (more than 40% of total calories) consumption of animal fat containing saturated and trans isomers of fatty acids and cholesterol, on the other hand. .
It is believed that an increase in cholesterol consumption in the amount of 100 mg per 1000 kcal/day helps to increase blood cholesterol by 12%. At the same time, a 1% decrease in total serum cholesterol is associated with a 2% decrease in the risk of coronary artery disease. According to the recommendations of the National Cholesterol Education Program, for moderate hypercholesterolemia, the amount of cholesterol in the diet should not exceed 300 mg/day, and for severe hypercholesterolemia, 200 mg/day. In this regard, the need for dietary and drug correction of HCS is obvious.
Diagnosis of lipid metabolism disorders
To diagnose lipid metabolism disorders and monitor the effectiveness of correction, the criteria of the All-Russian Scientific Society of Cardiologists are used and the content of total cholesterol (TC), high- and low-density lipoprotein cholesterol (HDL and LDL) in the blood serum is determined, on the basis of which the atherogenic coefficient is calculated (see Table. 1).
In patients with concomitant coronary heart disease, atherosclerosis of the peripheral and carotid arteries, abdominal aortic aneurysm, and type 2 diabetes mellitus, total cholesterol and LDL cholesterol levels should be below 4.5 mmol/l (175 mg/dl) and 2.6 mmol/l (100 mg/dl) respectively.
Along with this, in case of secondary hypercholesterolemia, the functional state of various organs and systems is assessed: ECG registration, ultrasound of the abdominal organs, chest X-ray, etc.
At the Federal State Budgetary Institution "Research Institute of Nutrition" of the Russian Academy of Medical Sciences, examination of patients with hypercholesterolemia using the algorithm is carried out within the framework of the system of providing high-tech nutritional and medical care to patients with impaired lipoprotein metabolism - hyperlipidemia (GLP-ICD 10 E 78, 78.0, 78.1) - in accordance with domestic and international standards medical care.
The third module (“Nutritest-IP 3”) includes a complex of clinical, physiological, instrumental, biochemical, immunochemical and genetic studies, including:
- study of basal metabolism and calculation of the oxidation rates of macronutrients (proteins, fats, carbohydrates) using intermediate indicators of non-protein energy expenditure and non-protein respiratory coefficient, as well as assessment of energy expenditure during physical and nutritional exercise Eact.;
- assessment of the component composition of the body (x-ray densitometry, computed tomography, MRI) with determination of the content of fat and lean mass, visceral fat, as well as bone mineral density;
- assessment of lipid metabolism with determination of the content of apolipoproteins A, B, lipoprotein (a), the spectrum of fatty acids, phospholipid composition of erythrocytes, etc.;
- assessment of carbohydrate metabolism disorders with determination of insulin resistance markers (Caro index, Homa-IR criterion, β-cell functional activity index, etc.);
- assessment of protein metabolism with determination of the content of homocysteine, albumin, prealbumin, transferrin, C-reactive protein;
- study of hormonal (insulin, C-peptide, glucagon, leptin, adiponectin, resistin, ghrelin, cortisol, aldosterone, ACTH, prolactin, thyroid hormones) status;
- determination of the body’s supply of vitamins (B1, B2, B6, B12, A, C, E, folic acid, etc.), macro- and microelements (magnesium, iron, potassium, iodine, selenium, zinc, chromium, etc.);
- study of immune status (immunoglobulins, TNF-α, IL-1, 2, 4, 6);
- study of antioxidant status with determination of the content of malondialdehyde and diene conjugates in plasma and erythrocytes, as well as the activity of superoxide dismutase, glutathione peroxidase, glutathione reductase and catalase. In recent years, F2-isoprostane and 8-oxo-7,8-dihydroguanine have been used as markers of oxidative stress associated with stimulation of smooth muscle cells and DNA damage;
- study of the functional state of the cardiovascular system (Holter ECG monitoring, bicycle ergometry, treadmill test, stress echocardiography, coronary angiography, ventriculography, myocardial scintigraphy with 201 T1, radionuclide ventriculography, myocardial scintigraphy with 99m Tc-pyrophosphate), kidneys, nervous and endocrine systems , digestive system;
- genotyping with assessment of the expression of genes for apoproteins APO-E, APO-B, APO-C3, lipoprotein lipase, prothrombin (FII), plasminogen activator inhibitor (PAI-1), methylenetetrohydrofolate reductase (MTHFR), NO synthase (NOS), beta-adrenergic receptors and etc.
Table 1. Criteria for diagnosing lipid metabolism disorders
| Lipid parameters | Values in mmol/l | Values in mg/dl |
| OXC | < 5,0 | < 200 |
| LDL cholesterol | < 3,0 | < 115 |
| HDL cholesterol | > 1.0 (for men), 1.2 (for women) | > 40 (for men), 46 (for women) |
| TG | < 1,77 | < 155 |
| (TC - HDL cholesterol) / HDL cholesterol | < 4 | |
You can find an example of a consultation of a patient with hypercholesterolemia conducted by A. V. Pogozheva, MD, professor of the Federal State Budgetary Institution “Research Institute of Nutrition” of the Russian Academy of Medical Sciences (Moscow), in the article “Clinical observation”, heading “Situation”.
Expert Yu. V. Abakumova, MD, professor, general practitioner of the highest category, chairman of the Saratov regional branch of the Academy of Medical and Technical Sciences of the Russian Federation:
Without a doubt, the most famous compound is cholesterol. Probably no other molecule has made a greater contribution to medicine (cardiology, nutrition, general pathology, biochemistry, etc.). Cholesterol can rightfully be called a molecule of the 20th century. Throughout the 20th century, researchers studied him, either accusing him of almost all sins, or completely justifying him. To date, the case has ended in an acquittal: high cholesterol intake does not cause atherosclerosis and coronary heart disease. The occurrence of these diseases depends on other factors.
Data obtained by scientists from the Saratov regional branch of the Academy of Medical and Technical Sciences of the Russian Federation in one of the studies also confirm the “innocence” of cholesterol. We compared the amount of dietary cholesterol in the diet of patients with active atherosclerosis (group 1) and healthy individuals (group 2). It turned out that both sick and healthy people received almost the same amount of cholesterol from food, namely about 0.4 g/day. Also, their levels of total cholesterol in the blood did not differ, which was confirmed by other researchers. Thus, neither patients with active atherosclerosis nor healthy individuals (i.e., before the disease develops) have excess dietary cholesterol.
A person receives about 400 mg of cholesterol per day from food. The body itself synthesizes about 1200 mg/day. The average total amount is about 1600 mg/day. It has now been proven that dietary cholesterol does not affect the development of hyperlipidemia and atherosclerosis!
There is no clause limiting cholesterol intake in current WHO recommendations for proper nutrition! This is absolutely true, since hyperlipidemia is formed as a result of increased formation (synthesis) of lipids in various tissues, primarily in the liver. Almost all cells and tissues of the body have cholesterol synthesis systems. Why? Because cholesterol is a vital substance, without which the cell dies. Each cell has its own cholesterol synthesis system. This property is a kind of insurance in case there is suddenly a deficiency in the supply of this substance with food or for some reason its hepatic synthesis stops.
The role of cholesterol
There are three ways the body uses cholesterol:
- Synthesis of steroid hormones (about 10% of the total cholesterol pool).
- Synthesis of bile acids, without which digestion is impossible, and synthesis of vitamin-like substances.
- Construction of the cell wall and all intracellular membranes. Without this (structural) cholesterol, the cell dies.
Cholesterol plays the role of a structural stabilizer of membranes. The membrane is a fairly “fluid”, unstable formation in which pores, ruptures, and so-called breakdown phenomena easily form. Through them there is an uncontrolled flow of various substances into the cell, and the contents of the cytoplasm can leak out. The incorporation of cholesterol molecules into the membrane strengthens it, imparts rigidity to the entire structure, stopping breakdown phenomena, ensuring controlled operation of pores and receptors.
With a deficiency of cholesterol, the risk of cancerous cell degeneration increases. Therefore, when treating a patient, you should not reduce the level of cholesterol in the blood below normal limits.
Animal products are rich in cholesterol: meat, lard, whole milk, butter, seafood (mussels, oysters, etc.). However, as follows from the above, there is no particular need for strict dietary regulation in relation to cholesterol.
Thus, the cause of hyperlipidemia is either increased cholesterol synthesis in the body (primarily in the liver) or a decrease in its use. A decrease in consumption for hormone synthesis naturally occurs in old age, which is also associated with the progression of atherosclerosis at this age.
Want more new information on nutrition issues? Subscribe to the informational and practical magazine “Practical Dietetics”!
SUBSCRIBE
Liver and cholesterol
First of all, it is necessary to pay attention to the functional state of the liver - the organ that produces cholesterol “for export”, i.e. for the whole body. Why does it suddenly produce more of this substance than it needs?
In general, cholesterol synthesis is a regulated process. This means that the liver synthetic systems form it as much as the body needs. When there is an excess of dietary intake, cholesterol synthetic systems reduce the volume of production. And vice versa. This has been proven by experiments with a radioactive label.
However, with the development of atherosclerosis, the amount of cholesterol in the body increases. That is why the term “cholesterolosis” appeared (Yu. M. Lopukhin).
For a very long time there was no answer to the question about the causes of impaired liver function. Various versions have been proposed, but all are insufficiently proven. However, in the 1970s. American researcher Catherine Fabrikant accidentally discovered that certain viruses can disrupt the cholesterol and lipid synthetic systems of the liver. These results were later confirmed by the results of extensive experiments conducted by Belarusian researchers.
The ability to disrupt the above liver systems has been noted in some viruses: respiratory (for example, influenza), enteroviruses, hepadnaviruses. But the damage they caused turned out to be more or less temporary. After a certain time, the cell restores its enzyme systems. And only damage caused by the herpes virus cannot be repaired. It is persistent and remains forever. As a result of the attack of the herpes virus, the liver cell “does not hear” inhibitory signals to stop the synthesis of cholesterol and continues to form this substance, as well as the corresponding apoproteins in large quantities.
Where is cholesterol spent in the body?
Cholesterol comes from the liver into the blood as part of lipoproteins. Lipids are not present in free form in the blood, because they are water insoluble. To impart hydrophilicity and for transport through the bloodstream, they bind to special carrier proteins (apoproteins) and become lipoproteins. In addition to the transport function, apoproteins isolate the active centers of certain fat molecules, for example, fatty acids, which are active saponifiers (without the insulating effect of apoproteins, they would quickly saponify all blood vessels from the inside).
The fixation of cholesterol in blood vessels depends on the ratio of saturated and polyene fatty acids in lipoproteins, since cholesterol ester with a saturated fatty acid is difficult to remove by high-density lipoprotein. When studying the characteristics of fatty acids in lipoproteins, it was found that in LDL and in the cells of patients with atherosclerosis (A), the level of polyenoic acids is reduced.
But the consumption of fatty acids is a food factor! Depending on the nature of the foods and fats, the body receives fatty acids with different properties. With some (unsaturated) cholesterol esters it is easy to remove from tissues, but with others (saturated) it is very difficult. Consequently, the choice is up to the quality (and quantity) of dietary fats - triglycerides (TG), which contain fatty acids.
Triglycerides, or true fats, contain fatty acids. These are long, most often single-chain compounds containing up to 22 carbon atoms. Their chemical formula is approximately this:
H3C - CH2 - CH2 - CH2 - CH2 - - CH2 - CH2 - CH2 - COOH
It is they that “burn” in the body, releasing the energy of the chemical bond “CH2 - CH2”. The body uses them as fuel, like “gasoline,” and practically does not use them as plastic material. The chemical bond energy in fatty acids is very high. Oxidation (“combustion”) of 1 g of fatty acids provides 9 kcal of energy, i.e. almost the same as gasoline - 10.5 kcal / g (for comparison: carbohydrates - 4 kcal). Triglycerides are found in many foods: meat, lard, vegetable fats. Actually, vegetable oils are triglycerides.
Recently, special attention has been paid to myristic acid. This fatty acid is part of milk fats. The special chemical properties of this acid lead to the growth of LDL in the blood, which is deposited in tissues and is difficult to remove from the body.
European experience
According to a number of researchers, in European countries there is a clear connection between the consumption of dairy fats and the prevalence of cardiovascular diseases. These data served as the basis for a national program of measures to change the nutrition of the population in Finland. The experience of this country, which has achieved a significant reduction in the incidence of CVD, is very important both for similar programs in other countries, and for every family, every person shaping their diet.
In Finland, as in other Nordic countries, a unique diet has historically developed with a high consumption of meat, whole milk, dairy fats and a low consumption of vegetables, fruits, fish, and vegetable oils. Morbidity and mortality from CVD were very high.
Since 1972, a nationwide program for the prevention of these diseases began to operate in Finland. Among the measures carried out within the framework of this program was a fundamental change in diet. As a result of the implementation of the national program, the consumption of vegetables increased 3 times, fish - 2 times. Two facts deserve special attention: firstly, a sharp reduction in the use of whole non-skimmed milk and the transition to skimmed milk and, secondly, the transition to the use of vegetable rapeseed oil instead of butter. While before 1972, about 80% of the population consumed skim milk and butter and only 5% consumed skim milk and vegetable oil, by 1997 only 20% of the population continued to consume high-fat dairy products. It is clear that the implementation of the Finnish national project has led to a sharp reduction in the consumption of myristic acid. Quantity turned into quality: mortality from CVD fell by 60%. Such a vivid experience of Finland can serve as an example both for large social groups and for an individual family or individual.
Be careful with medications!
Fixation of cholesterol in the vascular wall depends on various changes: liver dysfunction, hypothyroidism, diabetes mellitus, nephrotic syndrome, iatrogenic factors.
When looking for the causes of hyperlipidemia in a patient, special attention should be paid to taking medications. Thus, the use of progestins and oral contraceptives, which have sharply increased recently and are often prescribed by gynecologists without good reason, leads to pronounced changes in lipid metabolism and hypercholesterolemia. After their abolition, normalization of lipidemia does not occur immediately, but over a long period of time. The use of diuretics (except indapamide) and beta-blockers, i.e., drugs most often prescribed to patients with coronary artery disease and atherosclerosis, is also one of the factors of hypercholesterolemia.
Medical misconceptions
To assess lipidemia, the patient undergoes a comprehensive study - a lipid profile, total cholesterol (2.2–5.3), HDL, triglycerides, and LDL are determined. Both the absolute values of these indicators and their relationships with each other are important. Thus, with total cholesterol greater than 6.22 mmol/l and an LDL:HDL ratio greater than 5:1, the risk of developing atherosclerosis is considered high. In contrast, the level of triglycerides is not directly related to the development of atherosclerosis and the progression of hypercholesterolemia, but rather reflects dietary fat intake and pancreatic dysfunction, which must be taken into account when prescribing treatment.
A lipidogram carries very limited information: more or less lipids of a certain type in the blood. The attention of practitioners to lipid profiles and hyperlipidemia is often unreasonably great. They are trying to associate the development of atherosclerosis with changes in the lipid profile and hyperlipidemia, and to judge from it the degree of atherosclerotic vascular damage. However, such conclusions cannot be drawn! In practice, combinations often occur:
- the patient has hyperlipidemia, but without atherosclerotic vascular lesions;
- severe atherosclerotic vascular damage without hyperlipidemia.
As a result of scientific research conducted by scientists from the Saratov regional branch of the Academy of Medical and Technical Sciences of the Russian Federation, it was found that the average levels of cholesterol in the plasma of patients and healthy people differ little (5.04 ± 0.9 and 4.9 ± 0.6, respectively, with p > 0.05). Undoubtedly, there is a certain relationship between cholesterol levels and the development of atherosclerosis. However, as Professor E. Sh. Halfen, who spent his entire life working on this very issue, once said at a scientific conference: “I don’t know what connection this is.”
Why do doctors keep trying to link hyperlipidemia and atherosclerosis?
Because until recently, the lipid concept of the development of atherosclerosis was generally accepted; more precisely, until now it has not been possible to replace it with any more compelling theory. At first, its essence was expressed by the phrase “without cholesterol there is no atherosclerosis”, and then - “without lipoproteins there is no atherosclerosis”.
How are atherosclerosis and hyperlipidemia related (if related)?
Atherosclerosis is a disease, a characteristic feature of which is the formation of atherosclerotic plaques in the walls of arteries - pathological formations, unique in their structure and cellular composition, the development of disturbances in the blood supply to internal organs, damage to their structure and function. In the pathogenesis of this disease, disturbances in thrombus formation, energy production, and disturbances in lipid and carbohydrate metabolism are important. Internal organs are characterized by the development of heart attacks, as well as ischemic and diffuse sclerotic changes. As can be seen from this (incomplete) definition, hyperlipidemia is one of the factors in the pathogenesis of atherosclerosis, and is not at all determining. It (hyperlipidemia) may or may not be present in a patient with atherosclerosis or coronary heart disease, ischemic brain disease, etc. Atherosclerosis develops regardless of its presence or absence. With some caution, hyperlipidemia can be considered as a marker of the development of atherosclerosis, but even then it is not very sensitive.
Should hyperlipidemia be treated?
Rather, it is necessary to treat atherosclerosis. However, recently the number of patients in whom hyperlipidemia is combined with hepatic steatosis in the absence of atherosclerotic changes has increased. Most likely, we are talking about a kind of debut of atherosclerosis, when there are metabolic changes, but not (yet) structural ones. Although there may be other pathological processes. In this case, the use of appropriate diets gives good results and hyperlipidemia is a convenient marker for monitoring the dynamics of the process.
How to treat?
Firstly, do not use statin drugs until the last possible opportunity due to their hepatotoxicity and serious side effects.
Secondly, apply diets, primarily individual ones, taking into account the characteristics of a particular patient. The first step in creating a diet is to provide the body with quantitatively adequate protein that is complete in amino acid composition. After this, issues of quantity and quality of fats are resolved.
Dangerous products
What other nutritional components, nutrients, foods, dishes have the greatest impact on human health, promote or prevent the development of cardiovascular pathology?
Trans fatty acids are fatty acids with an unusual structure. The main amount of trans fats is produced in the food industry using the technology of hydrogenation of vegetable and fish oils to produce margarine and a number of oils. Food products prepared with trans fats have a long shelf life and do not go rancid (chips and other crunchy foods, for example). Trans fats significantly change the fat and carbohydrate metabolism of the human body and significantly potentiate the development of cardiovascular diseases and cancer.
According to WHO experts, the epidemic of cardiovascular diseases can be explained by high consumption of saturated fatty acids and trans fats. Thus, it is not the total fat intake that is important, but the nature of the fat in a person's diet. WHO recommends significantly limiting the consumption of foods that contain trans fats and saturated fats, especially myristic acid.
Healthy fats
Among the fats, which are very diverse in their chemical structure, role in the body and effect in relation to various diseases, there are also those that prevent the development of cardiovascular diseases.
There are some types of fatty acids that are not used for energy supply, but are involved in the synthesis of a number of important compounds. These are the so-called polyunsaturated fatty acids (linoleic, linolenic, etc.) and branched-chain fatty acids.
Their structure contains double bonds:
H3C - CH2 - CH2 = CH2 - CH2 - CH2 = CH2 - CH2 - COOH
They are found in vegetable oils (especially flaxseed, soybean), nuts, seeds, and fish oil. Introducing them into the diet in sufficient quantities is mandatory to maintain health and prevent disease. The so-called polyunsaturated fatty acids of the omega-3 class also prevent the development of CVD. These fats are found in the greatest quantities in nuts and in the fat of northern sea fish (tuna, herring, salmon, etc.). Today it has been proven that omega-3 polyunsaturated fatty acids have a multifaceted effect on the human body at different age periods.
Firstly, they are necessary for the proper development of the brain of children (of different ages).
Secondly, they are necessary for the normal functioning of the immune system throughout a person’s life.
Third, eating these fats reduces triglyceride levels in the blood and prevents the development of CVD.
Fourthly, omega-3 polyunsaturated fats reduce the tendency to form clots in the blood, minimizing the process of thrombosis. This is very important, because increased thrombus formation is an independent risk factor for the development of myocardial infarction and stroke.
Fifthly, omega-3 polyunsaturated fats stabilize the heart rate, and this is considered their most remarkable property. In fact, studies have shown a significant - 45-70% - reduction in the likelihood of sudden death from cardiac arrest. However, low intake of omega-3 fats is associated with a high incidence of sudden death from cardiac arrest.
According to WHO analytical reports, it has been established that “consumption of omega-3 fatty acids is a key determinant of the prevalence of coronary heart disease, reducing the likelihood of sudden death from cardiac arrhythmia.”
Sources of polyunsaturated fatty acids of the omega-3 class are fish oil, fatty sea fish, and nuts. To achieve an adequate intake of omega-3 fats, it is recommended to either adopt a Mediterranean-type diet rich in nuts and fish, or consume fish oil, or use special omega-3 fatty acid supplements.
In 2002, experts from the WHO European Bureau set targets for nutrients that are necessary to achieve a good level of public health. Some of them are given in table. 2.
Based on the targets, the WHO Regional Office for Europe has developed 12 principles of healthy eating (see “Principles of healthy eating”).
Historical fact
In conclusion, I would like to turn to history, with which it is worth starting the study of any issue.
We will not be mistaken if we say that the development of medicine throughout the 20th century took place under the banner of cholesterol and this same substance was the basis of many scientific myths.
Isolated in its pure form at the end of the 19th century, cholesterol, after experiments on animals, was suspected of being the cause of the development of atherosclerosis. The experiments of N. N. Anichkov and S. S. Khalatov (1912) are best known to society. It is generally accepted that these scientists managed to obtain experimental atherosclerosis. However, this is not quite true.
At a meeting of the Society of Russian Doctors in St. Petersburg, N. N. Anichkov reported that after feeding with cholesterol, rabbits exhibit severe fatty degeneration of the liver and bone marrow (which does not happen with atherosclerosis). At the same time, foci of cholesterol deposition were identified in the intima of the aorta, but without changes in the condition of other vessels. In areas of cholesterol infiltration, smooth muscle infiltrates and other elements of the atherosclerotic plaque, sclerosis and vascular deformations characteristic of spontaneous human atherosclerosis were not found. It is noteworthy that rabbits with experimental atherosclerosis do not develop myocardial infarction. These differences in experimental atherosclerosis can be associated with the peculiarities of the endothelial structure and cholesterol metabolism of the rabbit. Thus, it is clear that atherosclerosis was not obtained. Since the rabbit is a herbivore in its metabolism, does not receive cholesterol from food and cholesterol is a foreign substance for it, then after the experiments with rabbits, experiments were carried out with carnivorous and omnivorous animals: dogs, pigs, rats, i.e. with animals similar to humans in their exchange. They showed that dietary intake of cholesterol, even in very large quantities, does not lead to atherosclerosis or any deposition of cholesterol in blood vessels, and the changes obtained in herbivores are a storage disease. By the end of the 1920s. The inconsistency of the theory of food origin of atherosclerosis was absolutely clear. However, in the absence of another, I had to accept this theory as at least a working concept.
Principles of healthy eating
- Eat a nutritious diet based on a variety of foods, mostly plant-based rather than animal-based.
- Eat bread, grain products, pasta, rice, potatoes several times a day.
- Eat a variety of vegetables and fruits several times a day, preferably fresh and locally sourced (at least 400 g/day).
- Maintain your body weight within the recommended range (BMI 20–25) through moderate exercise, preferably daily.
- Control your fat intake (no more than 30% of daily energy) and replace most saturated fats with unsaturated vegetable oils.
- Replace fatty meats and meat products with beans, legumes, lentils, fish, poultry or lean meats.
- Consume milk and dairy products (kefir, curdled milk, yogurt, cheese) that are low in fat and salt.
- Choose foods that are low in sugar and eat less refined sugar by limiting how often you consume sugary drinks and sweets.
- Choose foods low in salt. Total salt consumption should be no more than 1 tsp. (6 g) per day, including salt found in other foods.
- If alcohol consumption is allowed, it should be limited to two drinks (10 g of alcohol each) per day.
- Prepare food in a safe and hygienic manner. Steaming, baking, boiling or microwaving foods can help reduce the amount of added fat.
- Promote exclusive breastfeeding and the introduction of safe and adequate complementary foods from 6 months, with breastfeeding continuing throughout the first years of life.
Source: CINDI Nutrition Program Guide (EUR/00/5018028, E70041R).
Table 2. Some target indicators for developing a healthy lifestyle
| Index | Target value |
| Physical activity level | > 1,75 |
| Adult body weight | BMI 21–22 |
| Proportion of energy obtained from: complex carbohydrates | > 55 % |
| amount of fatty acids | < 30 % |
| saturated fatty acids | < 10 % |
| trans fats | < 2% |
| Omega-3 | 2 g/day linoleic acid |
| Very long chain fatty acids | 200 mg/day |
| Vegetables and fruits | > 400 g/day |
| Table salt NaCI | < 6 g/day |
| Exclusive breastfeeding | About 6 months |