Lipid metabolism disorders (dyslipidemia) affect the processes of absorption, transformation and metabolism of fats in the body. In addition to their energy function, fats are an important component of cell membranes, participate in the synthesis of hormones, transmit nerve impulses, and perform a host of other vital tasks. Therefore, a violation of lipid metabolism significantly affects the condition of the entire organism as a whole and can lead to the development of severe consequences.
Causes of dyslipidemia
- Nutritional – eating large amounts of animal and vegetable fats. The norm is set individually for each person, the average is from 0.8 to 1 g. fat per kilogram of body weight per day.
- Congenital disorders of lipid metabolism. They arise as a result of mutations in genes that are responsible for the processes of synthesis, breakdown, and transportation of fats. These mutations are passed on from generation to generation, so the disease can occur in young children for no apparent reason. Examples of genetic disorders of lipid metabolism are Gaucher disease, Tay-Sachs disease, and Niemann-Pick disease.
- Secondary disorders of lipid metabolism. Caused by other diseases that can affect the gastrointestinal tract, endocrine and enzyme systems, various internal organs (liver, kidneys).
Among the provoking factors that increase the risk of developing lipid metabolism disorders are bad habits (smoking, alcohol abuse), a sedentary lifestyle, excess weight, chronic stress, and taking hormonal medications.
How does lipid metabolism disorder manifest itself?
At first glance, it may seem that a disorder of lipid metabolism necessarily manifests itself in the form of excessive deposition of subcutaneous fat in various parts of the body. This symptom can develop, but it is not specific, but is characteristic of many other conditions. The clinical picture of dyslipidemia depends on whether the concentration of fats in the blood is increased or decreased. In the first case, the following symptoms are noted:
- the appearance of cholesterol deposits on the eyelids, abdomen, face, and limbs. Externally, they look like yellowish spots, slightly elevated above the surface of the skin;
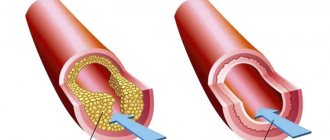
- vascular atherosclerosis, which is accompanied by pain in the heart, breathing problems, changes in heart rhythm and other signs;
- enlarged liver and spleen;
- hypertonic disease;
- cholesterol ring along the edge of the iris.
If lipid metabolism disorders lead to a decrease in the amount of fat in the body, then symptoms such as hair loss and early graying, inflammatory skin lesions, nail separation, and menstrual cycle disruption in women occur.
Features of treatment
Various approaches are used to correct lipid metabolism disorders. If the problem was caused by nutritional reasons, then the patient is transferred to the hands of a nutritionist who develops a plan for proper nutrition and exercise. If lipid metabolism disorders appear as a result of concomitant diseases, then they begin to treat them. Some diseases cannot be treated (for example, diabetes), so the doctor develops an individual list of recommendations that will help normalize lipid metabolism and improve the patient’s quality of life.
Dyslipidemia - symptoms and treatment
The prognosis of DL depends on the form and severity of the syndrome, the degree of development of atherosclerosis and the presence of atherosclerosis-related diseases.
Prevention of DL is based on behavioral measures.
A balanced diet can reduce LDL by only up to 20%, but the effect of diet on TG and VLDL is noted. In addition, a healthy diet is a significant factor in reducing overall mortality.
The amount of calories consumed from food should help maintain normal body weight. In this regard, it is recommended to limit the consumption of animal fats (no more than 10%), and the total amount of fat should not exceed 20-30% of the total daily caloric intake. The daily intake of cholesterol from food should not exceed 300 mg in persons without DL and atherosclerosis, and in the presence of these conditions - no more than 200 mg.
It is important to reduce your intake of saturated fat and not overemphasize the importance of limiting certain fatty foods, such as eggs, as they are a valuable source of many nutrients. Particularly atherogenic saturated fats are trans fats found in hard margarines and processed foods.[9][13]
Fruits and vegetables (not counting potatoes) should be consumed at least 400-500 g per day. The consumption of meat products, offal and red meat should be limited. It is better to eat more other protein foods: legumes, fish or poultry. Every day you need to consume dairy products low in fat and salt (kefir, sour milk, cheese, yogurt).
Simple sugars are needed in daily food, but their share should not exceed 10% of the total calorie intake. The total amount of salt consumed, including salt contained in prepared foods, should not exceed 5 g per day, this is especially important for people with arterial hypertension.
It is useful to eat deep-sea fish from the northern seas (selfish, sardines, mackerel, salmon) at least 2-3 times a week. This is due to the high content of ω-3 PUFAs in these varieties, which help prevent atherosclerosis. Plant sterols/stanols are found in plant seeds, nuts and vegetable oils. In doses of about 2 g per day, they do not allow cholesterol to be absorbed in the intestine.[2][4]
Reducing excess weight is a prerequisite for the prevention of DL and cardiovascular complications. Reducing body weight is achieved by prescribing a low-calorie diet and regular adequate physical activity. For anthropometric assessment, the body mass index (BMI) = weight in kg/height m2 should be used. Normal BMI is 18.5-25 kg/m2. Waist circumference (WC) is measured to assess the type of obesity. The normal WC in men is no more than 94 cm, in women – no more than 80 cm. WC over 102 cm in men and 88 cm in women is an indicator of abdominal obesity, which is associated with an increased risk of cardiovascular complications.[15]
All patients with DL, excess body weight and other risk factors are recommended to increase daily physical activity, taking into account age, fitness and existing diseases. The most physiological, safe and accessible aerobic physical exercise for everyone is walking. It is recommended to do it 5-6 times a week for at least 30-45 minutes, achieving a heart rate of 60-75% of the maximum for a person. The maximum heart rate is calculated using the formula: 220 – age (years). People with coronary artery disease and other diseases of the cardiovascular system should develop an individual training regimen, taking into account the performance of a stress test (bicycle ergometer or treadmill).[2][3]
Physical training is an important component of the prevention of DL. They reduce heart rate and blood pressure, allow adaptation to ischemic conditions, stabilize hormonal levels and tissue oxygenation. Aerobic, dynamic, cyclic loads of adequate intensity are more effective - walking, hiking, swimming, skiing and cycling.
It is important to quit smoking in any form, including passive smoking. The smoking cessation program algorithm consists of several principles:
- identification of smokers;
- assessment of the severity of the habit and readiness to get rid of it;
- an explanation of the dangers of smoking and a recommendation to quit it;
- if necessary, medical assistance, including complex therapy;
- Regular monitoring of a smoking patient by a doctor.
The most effective medication for quitting smoking is varenicline (Champix). It is a blocker of nicotinic receptors in the brain, as a result of which the craving for smoking is suppressed, the pleasure from the process is reduced and withdrawal symptoms are reduced.
A number of studies have shown that moderate alcohol consumption can have a positive effect on DL. Drinking no more than 150 ml of alcohol per week for men and 100 ml for women is considered safe for health, subject to daily consumption of no more than 20 g for men and 15 g for women. However, any doses of alcohol are not recommended for people with arterial hypertension, hypertriglyceridemia, diseases of the hepato-biliary and pancreatic zone, gout and obesity. Alcohol abuse during statin therapy can lead to myopathy and rhabdomyolysis.[6]
Preventive statin therapy is also an effective way to prevent DL. For this purpose, low doses of modern statins are often used:
- simvastatin 10-20 mg per day;
- atorvastatin 10-20 mg per day;
- rosuvastatin 5-10 mg per day;
- pitavastatin 1-2 mg per day.
Diagnostic methods
Before drawing up an examination plan, the doctor talks with the patient, determines the characteristics of his diet, finds out whether he is taking any medications, and whether there have been cases of lipid metabolism disorders in his relatives. After this, a comprehensive examination is prescribed, which may include the following methods:
- general and biochemical blood test;
- lipidogram (determination of cholesterol, high and low density lipoproteins);
- Ultrasound of internal organs;
- determination of hormone levels;
- anthropometry;
- ECG;
- ophthalmological examination, etc.
In order to identify defective genes that can lead to lipid metabolism disorders, genetic testing is prescribed. You can take it in medical genetics.
Manifestations of dyslipidemia
Depends on the location of cholesterol plaques. This is why they can look different in people with the same diagnosis.
The main symptoms of lipid metabolism disorders:
- arterial hypertension;
- angina pectoris at rest and exertion (pressing pain, burning in the heart area at rest or when performing physical work);
- sudden dizziness, noise and buzzing in the ears, memory impairment, sharp decrease in concentration;
- pain in the legs when walking;
- the formation of fat deposits in the skin (xanthoma) or in the eyelid area (xanthelasma).
If a person matches most of the points, then with a high degree of probability it can be assumed that his lipid metabolism is disturbed.
Obesity
Obesity
- excessive accumulation of adipose tissue in the body. Obesity is a multifactorial disease that is associated with numerous cardiac and metabolic risks. Body mass index (BMI) allows you to make a judgment about the content of adipose tissue. This indicator is calculated using the formula: BMI = Body weight (kg) / Height (m2).
The indicator is not informative for athletes, as well as for older people, since in the first case the muscles are overdeveloped, and in the second, on the contrary, they are atrophied.
The normal level of adipose tissue in men is 15–20% of body weight, in women – 25–30%.
Classification
There are several classifications of obesity. One of them takes into account BMI and the risk of cardiometabolic disorders.
Obesity level:
1) Normal weight, BMI < 25. 2) Overweight, BMI 25–29.9. 3) Obesity I degree, BMI 30–34.9. 4) Obesity II degree, BMI 35–39.9. 5) Stage III obesity, BMI >40.
Each group contains individuals with a metabolically healthy phenotype: WC in men ≤ 0.9; WC in women ≤ 0.85 and metabolically unhealthy phenotype: WC in men > 0.9; WC in women > 0.85, since not all obese people have metabolic disorders and, conversely, some people with normal body weight have disorders of carbohydrate and lipid metabolism. The group of “metabolically healthy obesity” includes those who, in addition to obesity, have one or less additional pathological factors against the background of normal tissue sensitivity to insulin.
According to the nature of the course, obesity can be progressive, stable and residual. The latter reflects residual effects after persistent weight loss.
Metabolism in adipose tissue and the pathogenesis of obesity
Adipose tissue is a type of connective tissue in the body. The main function of adipose tissue is to create an energy depot in the form of triglyceride reserves, provide thermal insulation, produce hormones and biologically active substances (adiponectin, leptin, etc.).
Adipose tissue is represented by a collection of fat cells - adipocytes. The number and size of adipocytes is a strictly individual indicator that varies from person to person. Under the influence of hormones such as insulin, glucocorticoids, T3, the number of adipocytes can increase.
The constancy of body mass and structure is ensured through the interaction of nervous and humoral mechanisms regulating food intake, consumption and storage in the form of energy.
The hypothalamus is the most important regulator of eating behavior, since it contains “. The hypothalamus controls the functioning of centers that control eating behavior and energy expenditure.
The hypothalamus receives signals:
- from the gastrointestinal tract about the filling of the stomach and other organs;
- about the chemical composition of blood - based on the content of glucose, amino acids, fatty acids;
- gastrointestinal hormones;
- adipose tissue hormones;
- signals from the cerebral cortex about the sight, taste and smell of food.
Some signals and substances stimulate feeding behavior, while others have an inhibitory effect. Factors regulating the amount of food consumed
In order for the amount of food eaten to actually correspond to the needs of the body, there are certain factors for the short-term and long-term regulation of food intake.
Mechanisms of short-term or rapid regulation:
1) Stomach fullness inhibits food consumption. 2) Eating stimulates the production of gastrointestinal hormones - cholecystokinin, peptide YY, glucagon-like peptide, which create a feeling of fullness. 3) The presence of food in the oral cavity, salivation, and swallowing inhibit the activity of the “hunger center” of the hypothalamus. 4) Level of ghrelin - a stomach hormone. After eating, its level decreases quickly, peak concentrations are observed before eating.
Mechanisms of long-term regulation:
1) A decrease in the concentration of glucose, amino acids, some fatty acids and keto acids leads to food motivation. When eating food, the concentration of insulin in the blood also increases. Insulin suppresses the activity of the “hunger center.”
2) Interaction with the “thermoregulation center”. Food consumption increases in cold conditions and decreases in hot conditions.
3) Signals from leptin - a hormone in adipose tissue that transmits a signal from adipose tissue about the body’s energy reserves. The increase in leptin levels is proportional to the increase in the amount of adipose tissue. An increase in the concentration of leptin in the blood promotes the development of a feeling of satiety and leads to a decrease in food consumption. In the hypothalamus, leptin initiates several responses at once, the essence of which is to reduce fat stores. Leptin inhibits the release of neuropeptide Y, which causes hunger; increases the activity of the sympathetic nervous system, increasing metabolic activity and energy expenditure; reduces insulin secretion by pancreatic b-cells.
Pathogenesis of obesity
If more energy contained in food enters the body than is consumed, then body weight increases.
The way to store energy is by storing fat. Therefore, the reason for the excess amount of adipose tissue is the excess of the intake of energy sources over its consumption. It does not matter what substances were supplied in excess quantities - proteins, fats or carbohydrates. Carbohydrates are a preferable source of energy than fats. When available, carbohydrates perform a fat-saving function. Excess carbohydrates that are not used for energy resources are converted into fats and stored. The same thing happens with excess proteins. Every 9.3 kcal of excess energy intake leads to the deposition of 1 gram of fat in the body. Fats accumulate under the skin, mainly in the thighs, buttocks and in the visceral spaces - in the omentum, mesentery. The liver and other organs also store small amounts of fat, but in smaller quantities. Recent studies have shown that new adipocytes can differentiate from progenitor cells at any period of life, and the development of obesity in adults is associated with an increase not only in the size of fat cells, but also in their number. Hormonal regulation of fat use 7 hormones have a strong regulatory effect on fat metabolism:
1) Adrenaline and norepinephrine are two hormones that work in stress reactions. Short-term and severe stress, heavy physical activity cause the mobilization of fats from the depot.
2) ACTH. The release of the hormone also increases under stress, while under the influence of ACTH the release of cortisol increases. Cortisol is a hormone of planned stress, unlike adrenaline and norepinephrine. Cortisol has a ketogenic effect on fat mobilization. If stress is long-term, then a prolonged and persistent increase in cortisol leads to obesity, which is accompanied by Cushing's syndrome/disease.
3) Growth hormone. Activates lipolysis and thereby increases the breakdown of fats. In obesity, the concentration of the hormone decreases due to an increase in the concentration of free fatty acids and insulin.
4) Thyroid hormones. They stimulate the mobilization of fats because they increase basal metabolism in cells. With a deficiency of triiodothyronine, thyroxine, hypothyroidism, obesity is observed, as the level of basal metabolism in cells decreases.
5) Insulin. Activates the process of synthesis and storage of fat - lipolysis.
Causes of obesity
There are a complex of reasons leading to obesity. There is a genetic determination of the intensity of energy metabolism and food consumption, but sometimes environmental factors and lifestyle play a dominant role in the development of obesity. 1) Reduced energy expenditure, including insufficient physical activity. In obese people, little physical activity is associated with weight loss and increased body fat. About 25–30% of daily energy expenditure comes from energy expenditure associated with muscle function. Therefore, regular physical activity and training increases muscle mass and reduces the amount of fat tissue. Even a single bout of exercise increases basal energy expenditure for several hours after cessation of exercise.
2) Eating disorder. Despite the presence of physiological mechanisms in the body that regulate food consumption, many harmful eating habits can cause the development of obesity. It has been proven that fat-rich foods predominate in the diet of obese people. Such products stretch the walls of the stomach to a lesser extent, have excessive calorie content, and do not require long chewing. Foods rich in fat taste better because they contain fat-soluble aromatic molecules that determine its taste. Additionally, the body requires less energy to store fats than carbohydrates. 3) Psychogenic factors. Some people develop obesity due to psychological factors. A sharp increase in body weight is observed during or after stress, as the sensitivity of the “saturation center” decreases. For example, the loss of a close relative, dismissal, serious illness and depression often cause overeating. For such a person, food becomes a means of reducing emotional stress.
4) Overfeeding children. The rate of formation of new fat cells is especially high in the first years of life. The higher the rate, the more adipocytes will differentiate in the body, the higher the risk of obesity.
5) Leptin resistance. In obese people, leptin levels are high, but the hypothalamic receptors become insensitive to its signals or the signal transmission process is disrupted. As a result, the sensitivity of the “satiety center” decreases, and a tendency to overeat appears. This condition is called leptin resistance. It is fraught with the fact that it contributes to the development of insulin resistance. Both conditions are risk factors for developing cardiovascular disease and type 2 diabetes. 6) Neurogenic disorders. Conditions such as tumors and injuries to the pituitary gland and hypothalamus can disrupt the regulatory systems that control eating behavior. 7) Genetic predisposition. Obesity often occurs as a family disease. The likelihood of developing overweight if your parents are obese is 70–80%. Concomitant diseases
Complications and diseases associated with obesity include:
- impaired glucose tolerance (IGT), impaired fasting glucose (IFG), or a combination thereof (any of the three positions characterizes the state of prediabetes);
- diabetes mellitus type 2;
- arterial hypertension;
- hypertriglyceridemia/dyslipidemia;
- obstructive apnea syndrome (syndrome of temporary cessation of breathing during sleep);
- non-alcoholic fatty liver disease;
- polycystic ovary syndrome;
- osteoarthritis;
- stress urinary incontinence;
- gastroesophageal reflux disease (GERD);
- limitation of mobility and social adaptation;
- psychoemotional disorders and/or stigmatization.
There is still no clear understanding of whether these conditions are a consequence or a cause of obesity, so it is customary to classify them as associated. Diagnosis of obesity
The diagnosis of obesity and further management of the patient are based on anamnestic data and data obtained as a result of an external examination, laboratory and instrumental examination.
When collecting anamnesis, the doctor clarifies the time of onset of obesity, is interested in the dynamics of weight changes, whether relatives have obesity, what kind of lifestyle, physical activity, and nutrition the patient has.
During the examination, the waist size, hip size must be measured, and the WC/TB ratio and body mass index are calculated.
Depending on the type of distribution of adipose tissue, obesity is:
- Visceral. Deposition of adipose tissue in the chest and abdomen, like an “apron”. Associated with a high risk of developing cardiovascular disease and type 2 diabetes. Waist to hip ratio >1.0.
- Peripheral. Deposition of adipose tissue in the buttocks and thighs. Associated with diseases of the spine and joints. Waist to hip ratio <1.0.
- Mixed. Characterized by an even distribution of adipose tissue.
If there is a need to evaluate in more detail the nature of the distribution of adipose tissue, the doctor will refer you to perform CT, MRI and ultrasound.
Standard for minimum laboratory examination for diagnosing metabolic disorders in obesity:
- Determination of the blood lipid spectrum (TC, HDL, LDL, ).
- Determination of carbohydrate metabolism indicators (fasting blood glucose, GTT, HbAC).
- Leptin, adiponectin.
- Indicators of liver and kidney function: ALT, AST, GGT, uric acid, creatinine.
- ECG.
Obesity caused by excess supply of energy resources must be distinguished from secondary or symptomatic obesity.
As a rule, it is associated with hereditary, endocrine and other somatic pathologies. Therefore, making a final diagnosis often requires the help of several specialists - a cardiologist, endocrinologist, neurologist, nutritionist, psychotherapist. To carry out differential diagnosis of various forms of obesity, special diagnostic algorithms are used: To exclude the hypothalamic genesis of obesity:
- examination by an endocrinologist, examination by a neurologist.
To exclude hypercortisolism:
- examination by an endocrinologist;
- dexamethasone test;
- laboratory tests: cortisol in 24-hour urine, ACTH.
To rule out PCOS:
- examination by a gynecologist;
- Ultrasound of the pelvic organs;
- blood hormones: , FSH, prolactin, testosterone, estradiol, DHEA-S, 17-hydroxyprogesterone (17-OP), SHBG;
- biochemical blood test: fasting plasma glucose, lipid spectrum, HOMA-IR.
To rule out hypothyroidism:
- examination by an endocrinologist;
- blood pressure measurement;
- laboratory tests: TSH, BC, lipid profile.
To exclude hyperprolactinemia:
- examination by an endocrinologist, examination by an ophthalmologist;
- laboratory tests: prolactin, lipid profile;
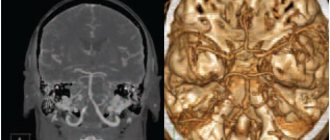
- MRI of the brain.