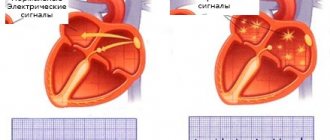
Arrhythmia is a violation of cardiac conduction, in which there is a change in the frequency, rhythm and regularity of contractions of the heart muscle. The heart may beat faster or, conversely, slower, or simply irregular.
Arrhythmia can be provoked by:
- disturbances in the formation of an electrical impulse in the sinus node (sinus tachycardia, bradycardia);
- violations of intracardiac impulse conduction. Occur as a result of a decrease or cessation of impulse transmission through the conduction system (blockade, premature excitation of the ventricles of the heart);
- combined rhythm disturbances. Combine disturbances in the conduction of electrical impulses and heartbeat rhythm.
Causes of cardiac arrhythmia
The causes can be divided into several blocks:
Extracardiac causes - not related to the heart itself:
- disorders of the thyroid gland;
- disruption of the cardiovascular and/or respiratory system;
- renal and/or liver failure;
- increased intracranial pressure;
- bad habits.
Intracardiac – organic or functional heart disorders:
- associated with the development of the conduction system of the heart
- SVC syndrome, nodular,
- atrial and ventricular extrasystole,
- some types of atrial and ventricular tachycardias.
atrioventricular tachycardia,
- heart failure;
myocardial infarction;
Physiological:
- heavy and prolonged physical activity;
- emotional overstrain.
Causes of arrhythmia
Arrhythmias can be caused by both heart pathologies and diseases of other organs and systems. Among the main reasons are the following:
- diseases of a cardiovascular nature (coronary heart disease, cardiomyopathy, hypertensive crisis, etc.);
- states of shock;
- intoxication (poisoning with alcohol, drugs, food poisoning);
- diseases of the endocrine system (diseases of the thyroid gland, adrenal glands);
- heart surgeries, heart injuries, and many others.
The danger of arrhythmia is that even in the absence of pronounced clinical manifestations and discomfort, without treatment it can lead to serious complications. In particular, a complication of atrial fibrillation is the development of acute heart failure, pulmonary embolism, and cerebrovascular accidents.
Symptoms of arrhythmia
The main symptom of arrhythmia is a change in the frequency or rhythm of the pulse, which is accompanied by a change in the patient’s well-being. However, a number of arrhythmias are hidden and may not be felt by the patient. Such arrhythmias are detected during preventive examinations or during diagnostic studies for another disease. The main method for diagnosing arrhythmia is an ECG.
There are “classic” manifestations of this disease, these include:
- heartbeat;
- heart sinking;
- feeling of “heart somersault” in the chest
- discomfort in the chest area;
- weakness;
- suffocation;
- dizziness;
- loss of consciousness.
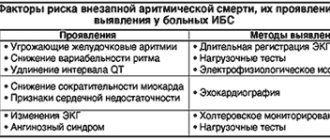
A number of diseases can cause quite serious complications. They can lead to the development of life-threatening arrhythmias (ventricular fibrillation and flutter), which threatens an unfavorable prognosis for the patient. If you notice any symptoms, contact a specialist immediately. At the Cardiology Center of the Federal Scientific and Clinical Center of the Federal Medical and Biological Agency, doctors with many years of experience will help identify the cause of your symptoms and conduct a full examination of your heart. The examination program of our center can be found here
Diagnosis of arrhythmia
Even a healthy person can experience arrhythmia. To prevent the disease, it is necessary to undergo an annual examination and check the functioning of the cardiovascular system, especially for older people.
At the initial appointment with a physician or cardiologist, the patient undergoes a physical examination. The doctor listens to the heart, examines the pulse, asks for complaints, studies the medical record and pays attention to what medications are prescribed.
After collecting anamnesis, the specialist prescribes an instrumental examination - ECG, ultrasound of the heart.
The most accurate method for diagnosing arrhythmia is considered to be Holter monitoring - an electrocardiographic study that is carried out throughout the day. In this case, the patient must record all his actions hourly. This is necessary to identify external influences that affected changes in heartbeat (physical activity, emotional stress). When interpreting the ECG, doctors will be able to assess the heart rhythm, its frequency and regularity. Afterwards the conductivity of electrical impulses is assessed.
Also used in diagnosis:
- treadmill test (step test) – conducting an ECG with physical activity. Used in the absence of constant attacks in order to correct the course of treatment;
- tilt test (passive orthostatic test) – is carried out on a special rotary table in the presence of doctors in compliance with full safety precautions. The patient is placed on the table in a horizontal position, pulse and blood pressure are measured. Then the table is raised up at an angle of 60 degrees and the patient’s pulse and blood pressure continue to be monitored;
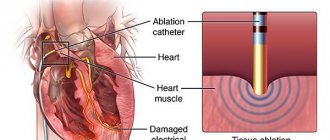
- invasive examination - surgical examination of the heart, during which special radiopaque catheters (probes) are inserted into the blood vessels;
- transesophageal electrophysiological study (TEPS) - performed through the esophagus to electrically stimulate the heart. A sterile electrode is inserted through the nose or nasopharynx to a depth of 40 cm, to the location of the esophagus closest to the heart. Weak electrical impulses begin to be sent.
The Cardiology Center of the Federal Scientific and Clinical Center of the Federal Medical and Biological Agency has a therapeutic department where they will help you determine the type of heart test and prescribe medication.
How to treat cardiac arrhythmia
To determine the treatment method, it is necessary to establish the cause of the disease. The selection of therapy and medications is carried out under systematic ECG control. Depending on the degree of arrhythmia, the doctor may prescribe a conservative treatment method using medications or cardiac surgery.
Only highly qualified doctors will be able to determine the diagnosis and prescribe the correct surgical treatment. Contact the Federal Scientific and Clinical Center FMBA, our specialists will select the treatment method that is suitable for you:
- electrocardiostimulation;
- implantation of a cardioverter-defibrillator;
- radiofrequency ablation.
Signs of heart rhythm disturbances on the ECG
With arrhythmia, the rhythm and frequency of the heartbeat changes, becoming more or less than normal. Irregular contractions and disturbances in the conduction of electrical impulses along the myocardial conduction system are recorded. A combination of more than two signs is possible. The localization of the pacemaker may migrate, causing it to become non-sinus.
One of the criteria for arrhythmia is the frequency of contractions and its form, constant or intermittent paroxysmal. The department in which the violation occurs is also taken into account. Pathological heart rhythm is divided into atrial and ventricular.
Sinus arrhythmia when the intracardiac impulse is disrupted in the focus of the sinus node is manifested by tachycardia or bradycardia:
- Tachycardia is characterized by an increase in contraction frequency to 90-100 per minute, while the rhythm remains correct. It occurs with increased automatism in the sinus node (SU), against the background of endocrine, cardiac and combined psychosomatic pathology. It can be respiratory, disappearing on inspiration. Tachycardia on the cardiogram - P waves precede each ventricular complex, equal R - R intervals are maintained, the contraction frequency increases from the age norm of an adult or child (more than 80-100 per minute). Arrhythmia looks like this on an ECG:
- Bradycardia is characterized by a decrease in beat rate to less than 60 beats per minute while maintaining the rhythm. Occurs when automatism in the nervous system decreases; the provoking factors are neuroendocrine diseases and infectious agents:
- on the ECG there is a sinus rhythm with preserved P, equal intervals R - R, while the heart rate decreases to less than 60 beats per minute or from the age norm.
- The sinus type of arrhythmia occurs when impulse transmission is disrupted, which is manifested by an irregular rhythm, more frequent or rare. It happens spontaneously in the form of paroxysm. When the atrial sinus is weakened in the focus, sick sinus syndrome develops:
- rhythm disturbance on the ECG manifests itself in the form of irregular sinus rhythm with a difference between the R - R intervals of no more than 10-15%. Heart rate decreases or increases on the cardiogram.
- Extrasystole indicates additional foci of excitation, in which heart contractions are recorded out of sequence. Depending on the area of excitation, atrial, atrioventricular or ventricular extrasystoles are distinguished. Each type of dysfunction has characteristic features on the electrocardiogram.
- Atrial supraventricular extrasystoles appear with deformed or negative P, with intact PQ, with a disturbed R-R interval and the coupling segment zone.
- Anti-ventricular extrasystoles on the ECG are detected in the form of the absence of P waves due to their overlap with the ventricular QRS with each extraordinary contraction. A compensatory pause occurs in the form of an interval between the R wave of the complex of the preceding extrasystole and the subsequent R, which looks on the ECG as:
- Ventricular ones are determined in the absence of P and the subsequent PQ interval, and the presence of altered QRST complexes.
- Blockades occur when the passage of impulses through the cardiac conduction system slows down. AV block is recorded when there is a failure at the level of the atrioventricular node or part of the His trunk. Depending on the degree of conduction disturbance, four types of arrhythmia are distinguished:
- the first is characterized by a slowdown in conduction, but the complexes do not fall out and PQ remains > 0.2 sec;
- the second - Mobitz 1 is manifested by slow conduction with a gradual lengthening and shortening of the PQ interval, loss of 1-2 ventricular contractions;
- the second type, Mobitz 2, is characterized by impulse conduction and loss of every second or third ventricular QRS complex;
- the third - complete block - develops when impulses do not pass from the upper sections to the ventricles, which is manifested by sinus rhythm with a normal heart rate of 60-80 and a reduced number of atrial contractions of about 40 beats per minute. Individual P waves and the manifestation of pacemaker dissociation are visible.
- The most dangerous are mixed arrhythmias, which occur when several pathological foci of excitation are active and chaotic contractions develop, with loss of coordinated functioning of the upper and lower parts of the heart. The disorder requires urgent help. There is flutter, atrial fibrillation or ventricular fibrillation. ECG data for arrhythmias are presented in the photo with interpretation below:
- with atrial fibrillation, arrhythmia appears on the ECG as frequent f waves of various shapes or sizes in the absence of the P wave. Against the background of large-wave heart rate, the heart rate reaches 300-450 per minute, with small-wave heart rate - more than 450 beats;
- with ventricular fibrillation, frequent contractions on the cardiogram are recorded in the form of the absence of habitually differentiated and associated complexes. Instead, chaotic waves of more than 300 beats per minute are detected. Shown in the ECG below:
- Arrhythmia in the form of flutter manifests itself as characteristic changes on the cardiogram:
- with atrial flutter, the ECG shows a non-sinus rhythm with sawtooth waves instead of P, a frequency of more than 300 per minute and F waves between the ventricular complexes. In contrast to the atrial fibrillation form, a sign of arrhythmia on the ECG is rhythmic atrial contractions with preserved QRS;
- with ventricular flutter, frequent and regular contractions (more than 150-200 per minute) are determined on the cardiogram. High and wide waves without the usual P waves and QRS complex, but almost equal in amplitude and shape. Continuity of a wavy line occurs when flutter waves transition from one to another, which manifests itself on the ECG as:
Arrhythmia looks like this on a cardiogram: