24-hour Holter ECG monitoring is a popular method of comprehensive cardiac examination. Compared to an ECG, it allows you to identify changes in the functioning of the heart muscle, register all possible variants of arrhythmias, determine the impact of physical activity on the body and receive expert recommendations from a cardiologist. Daily ECG diagnostics can reveal manifestations of pathology that are not obvious at first glance and allow the initiation of effective therapy.
Why do you need a holter?
ECG monitoring is prescribed by cardiologists to diagnose diseases and select the most effective therapy. You can also undergo an examination to prevent various types of heart pathologies. Indications for a Holter study include:
- complaints of chest pain;
- shortness of breath, arrhythmia and general weakness;
- regular presyncope;
- dizziness;
- interruptions in heart function;
- suspicion of myocardial ischemia, etc.
Holter is the only method of its kind for assessing the effectiveness of treatment for arrhythmia and coronary heart disease. Accurate data obtained from sensors allows us to reconsider the adequacy of the prescribed therapy. Using the information obtained, you can adjust your medication intake.
What the heart holter will show:
- heart rate;
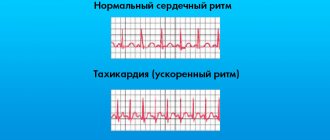
- heart rhythm disturbances;
- changes in PQ and QT intervals;
- ST segment response to physical activity;
- confirmation of arrhythmia;
- quality of conduction through the heart muscle, etc.
Since carrying a child increases the load on the cardiovascular system, a holter during pregnancy allows you to very accurately determine possible risks. It is especially important to consult a cardiologist if a woman has high blood pressure, chest pain, or arrhythmia at rest.
Request a call
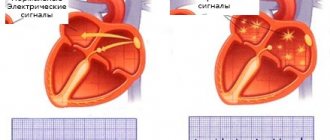
Restoring the sinus rhythm of the heart is possible in 2 ways: electrical and drug cardioversion.
The increased risk of thromboembolism (stroke) after cardioversion is well known. In this regard, antithrombotic therapy before restoring heart rhythm in AF is considered mandatory. Antithrombotic preparation for restoring heart rhythm in AF.
The increased risk of thromboembolism (stroke) after cardioversion is well known. Stroke is the most devastating consequence of AF. The cause of thromboembolic complications in AF in 75% of cases is thrombosis of the left atrium, in particular, the left atrial appendage.
The mechanism of thrombus formation is associated with a decrease in blood flow velocity in the left atrium. In AF, there is no full atrial systole, the left atrial appendage empties passively, as a result of which the speed of blood flow in its cavity decreases. With a decrease in the LV ejection fraction, the blood flow in the left atrial appendage slows down even more, up to complete stasis (stagnation) of the blood, and the size of the left atrium increases, which in turn promotes thrombus formation.
In this regard, anticoagulation is considered mandatory before elective cardioversion if AF persists for more than 48 hours or its duration is unknown.
Based on the results of cohort studies, treatment with vitamin K antagonists, maintaining an optimal INR of 2.0-3.0, should be continued for at least 3 weeks before cardioversion and 4 weeks after cardioversion. In the presence of risk factors for stroke (stroke risk index CHA2DS2-VASc) or recurrent AF, treatment with vitamin K antagonists is carried out lifelong, even if sinus rhythm is maintained after cardioversion.
If an episode of AF lasts less than 48 hours, emergency cardioversion can be performed under cover of intravenous unfractionated heparin (UFH) followed by an infusion of UFH or subcutaneous low molecular weight heparin (LMWH). In patients with risk factors for stroke, treatment with oral anticoagulants is started after cardioversion and continued for life. UFH or LMWH is used until the therapeutic INR is achieved (2.0-3.0).
The mandatory 3-week anticoagulation may be reduced if transesophageal echocardiography does not reveal a thrombus in the left atrium or left atrial appendage. Cardioversion guided by transesophageal echocardiography may serve as an alternative to 3 weeks of anticoagulation before rhythm restoration, and also in cases where early cardioversion is necessary, anticoagulation is not possible (patient refusal or high risk of bleeding), or there is a high probability of thrombus in the left atrium or its appendage.
If transesophageal echocardiography does not reveal a thrombus in the left atrium, then UFH or LMWH is prescribed before cardioversion, the administration of which is continued until the target INR is achieved while taking oral anticoagulants.
If a thrombus is present in the left atrium or left atrial appendage, treat with a vitamin K antagonist (INR 2.0–3.0) and repeat transesophageal echocardiography. When the thrombus dissolves, cardioversion can be performed, after which lifelong therapy with oral anticoagulants is prescribed. If thrombus persists, rhythm restoration may be abandoned in favor of ventricular rate control, especially if AF symptoms are controlled given the high risk of thromboembolism with cardioversion.
Electrical cardioversion of AF
Electrical cardioversion - stopping an attack of arrhythmia with a defibrillator discharge synchronized with an ECG (with the least vulnerable phase of the electrical ventricular systole, usually 20-30 ms after the apex of the R wave). Electrical defibrillation and cardioversion are usually combined under the term electrical impulse therapy (EPT).
Indications for external EIT for AF. • Lack of effect and/or intolerance to antiarrhythmic drug therapy; • Progressive heart failure due to paroxysmal AF; • Acute signs of hemodynamic disorders, heart failure, peripheral circulatory disorders.
Contraindications. • Rare short-term paroxysms of AF; • Intoxication with cardiac glycosides; • AF in thyrotoxicosis before correction of thyroid hormone levels; • AF in patients with complete atrioventricular block.
Preparation for planned restoration of heart rhythm in AF. Antithrombotic preparation before cardioversion, at least 3 weeks!
General guidelines include: • Last meal the evening before surgery. • The area where the defibrillation plates are applied (chest) should be shaved. • In the morning, stop taking medications.
External EIT technique.
EIT is performed in the intensive care unit or the X-ray operating room. EIT is carried out in a room equipped with: • equipment for monitoring the vital functions of the body (ECG, measuring blood pressure, respiratory rate and blood oxygen saturation) and carrying out resuscitation measures (defibrillator, breathing apparatus, monitors); • a specialized pacemaker, in case of heart block development.
Before EIT, intravenous access is established, monitoring of vital functions (ECG, blood pressure measurements, respiratory rate and blood oxygen saturation) is established, and a sedative drug is administered within 30 minutes. To perform the procedure, you lie on your back. The anesthesiologist administers medications and the patient falls asleep.
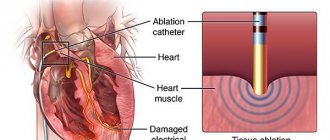
With external EIT, 2 electrodes are applied to the surface of the chest, one electrode is placed to the right of the sternum under the collarbone, and the second - in the area of the apex of the heart, and the center should be located in the sixth - seventh intercostal space along the anterior axillary line. This position is important for the coverage of the entire muscle mass of the myocardium by the flow of electrons. Figure The electrodes are coated with electrically conductive gel, pressed tightly against the chest so that there is no air between their surface and the skin, and a discharge is produced. The heart rhythm should be restored.
With a two-phase discharge, start with 100 J, and if necessary, increase the strength of each subsequent discharge by 50 J. Single-phase discharge requires 2 times more energy, that is, start with 200 J, followed by an increase of 100 J until a maximum level of 360 J is reached. .
Defibrillators that generate a bipolar pulse have a number of advantages over defibrillators that generate a monophasic pulse, because The “ability” of the discharge to eliminate fibrillation depends on the total value (in amperes) of the first and second half-waves, and the possibility of the damaging effect of the discharge is associated only with the value of the first half-wave. After EIT, you are transferred to a ward and prescribed bed rest for several hours. If you feel hungry, ask your doctor when you can eat. Check with your doctor about when to restart taking your medications, especially if you are taking glucose-lowering medications. Observation in the hospital after surgery from one day. Most patients can be safely discharged from the hospital within 24-48 hours after EIT.
Complications of external EIT for AF. – Thromboembolism (stroke). If AF persists for more than 48 hours or its duration is unknown, it is extremely important to take antithrombotic drugs to maintain an INR of 2.0-3.0 for at least 3 weeks to prevent thromboembolism. – Skin burns occur due to poor contact of the electrodes with the skin.
Medical cardioversion of AF
Drug cardioversion – stopping an attack of arrhythmia by administering antiarrhythmic drugs.
Indications. – Treatment strategy to control and maintain sinus rhythm. – Preparation for planned restoration of heart rhythm in AF. – Antithrombotic preparation before cardioversion, at least 3 weeks!
Technique of drug cardioversion.
Drug cardioversion of AF is carried out in an intensive care unit equipped with equipment for monitoring vital body functions (ECG, blood pressure, respiratory rate and oxygen saturation measurements). To perform the procedure, you lie down in bed on your back.
After drug cardioversion, bed rest is prescribed for 1-2 hours. If you feel hungry, ask your doctor when you can eat. Check with your doctor about when to restart taking your medications, especially if you are taking glucose-lowering medications.
Complications of drug cardioversion of AF. – Thromboembolism (stroke). If AF persists for more than 48 hours or its duration is unknown, in order to prevent thromboembolism, taking antithrombotic drugs with maintaining an INR of 2.0-3.0 for at least 3 weeks is extremely important. – Arrhythmogenic effect of antiarrhythmic drugs.
Revishvili A. Sh. “Clinical cardiology: diagnosis and treatment”, 2011. edited by Bockeria L.A., Golukhova E.Z.
How does a Holter ECG work?
In order to obtain diagnostic data, a cardiologist attaches several electrodes to the patient’s skin. The number of leads will depend on the characteristics of the device and in most cases varies from 3 to 12. The more electrodes are used, the more accurate the resulting Holter data on the heart.
Today, patients are offered several options for Holter monitoring:
- 3-channel Holter – used to detect rhythm and conduction disturbances of the heart;
- 12-channel Holter - used to detect rhythm and conduction disturbances, as well as to diagnose coronary heart disease and angina.
Holter: preparation for research
After connection, the operation of the equipment is tested, the patient is asked to take various body positions. After this, the examined patient can lead a normal lifestyle. Minor restrictions include the impossibility of water hygiene procedures and sports. In most cases, the examination lasts from one day to a week and varies between 22-28 hours. The patient is also recommended to keep a diary in which to record all the unpleasant sensations in the heart.
Modern technology is reliably protected from any interference and provides accurate data. Experts recommend using underwear that does not generate static electricity. It is important to understand how a halter is placed on women. Patients should wear short shirts, and outer clothing should not have tight sleeves.
Request a call
Implantation
Thanks to modern technology, the operation of implanting a cardiac pacemaker has become much easier. This procedure usually takes less than an hour. Typically, your doctor will apply local anesthesia to the area under your right collarbone. The electrode is then carefully inserted through a vein into the heart. Typically, the correct placement of the lead in the right atrium or ventricle is monitored by X-ray imaging. Only after a thorough check of the correct operation of the pacemaker is the electrode secured in the pacemaker. The pacemaker itself is implanted under the skin, in a small pocket below the right collarbone, and then the doctor places several stitches in the incision.
How to wear a halter correctly
During the diagnostic period, it is necessary to ensure that the device is not overcooled and does not come under the influence of a magnetic field. You need to follow your doctor's recommendations and ensure that the electrode is firmly attached to the body. In rare cases, the cardiologist decides to use a portable recorder for diagnosis, recording data “on demand”.
It is very important to understand how to remove a halter correctly. You need to check with your doctor in advance about the order in which you should proceed. In most cases, it is enough to simply peel off the sensors and remove the device. Even when the battery is disconnected, the received data remains in memory.