What is the Rh factor?
Rh factor (Rh factor) is a blood protein that is found on the surface of blood cells - red blood cells.
If this protein is present, then this means that the person has a positive Rh factor, but if it is not there, then it is negative. Rh factor is determined by antigen. There are five main antigens, but it is the D antigen that indicates Rh. 85% of the world's population have positive Rh factors. How to determine your Rh factor? It is enough to donate blood from a vein just once. This indicator does not change throughout life. The Rhesus status of the embryo is formed already in the first trimester of pregnancy. Determining this indicator is very important for the expectant mother, since in the case of an Rh-negative mother and an Rh-positive child, various pregnancy complications are possible. In this case, it will be especially important to follow the doctor’s instructions, avoid infectious and colds, as well as stress. Also on various websites there are so-called calculators that determine the Rh factor of the unborn child. It must be remembered that blood is donated on an empty stomach. A rapid Rh test can be taken at any independent laboratory where blood is taken (for example, Invitro). The price depends on the price list of the clinic itself. You can find out about the cost of the analysis immediately before delivery. You can also donate blood and find out your Rh factor for free if you become a donor. To do this, you need to fill out a form to register yourself as a blood donor at the appropriate institution.
The Rh factor also plays a big role in blood transfusions. A transfusion involves two people: the recipient (the one who receives the blood) and the donor (the one who donates the blood). If the blood is incompatible, the recipient may experience complications after the transfusion.
The most common myth among couples is that blood type (like the Rh factor) is inherited from a man. In fact, the inheritance of the Rh factor by a child is a rather complex and unpredictable process, and it cannot change during life. But it is worth remembering that in rare cases (about 1% of Europeans) a special type of Rh factor is determined - weakly positive. In this case, Rh is determined either positive or negative. This is where questions arise on forums: “why did my Rh minus change to plus?”, and legends also appear that this indicator may change. The sensitivity of the testing method plays an important role here.
An equally popular search on the Internet is “horoscope by blood type.” For example, in Japan, great attention is paid to deciphering blood type. Believe it or not - it's up to you.
In the world there is such a thing as a medical tattoo, photos of which can be easily found on the Internet. What do these tattoos mean and what are they for? Its designation is quite pragmatic - in case of a serious injury, when an urgent blood transfusion or surgery is required, and the victim is not able to give the doctor information about his blood type and Rh. Moreover, such tattoos (a simple application of the blood type and Rh factor) should be in places accessible to the doctor - shoulders, chest, arms.
Sources
- Ceniceros LC., Capitanio JP., Kinnally EL. Prenatal Relocation Stress Enhances Resilience Under Challenge in Infant Rhesus Macaques. // Front Behav Neurosci - 2021 - Vol15 - NNULL - p.641795; PMID:33854420
- Raguz MJ., Prce Z., Bjelanovic V., Bjelanovic I., Dzida S., Mabic M. 20 Years of Follow-up Alloimmunization and Hemolytic Disease in Newborn: Has Anything Changed in the Field Over the Years? // Klin Padiatr - 2021 - Vol232 - N6 - p.314-320; PMID:33063311
- Shirtcliff EA., Lubach GR., Mooney R., Beck RT., Fanning LK., Coe CL. Transgenerational propensities for infant birth weight reflect fetal growth history of the mother in rhesus monkeys. // Trends Dev Biol - 2021 - Vol12 - NNULL - p.55-65; PMID:32616989
- Deere JD., Chang WLW., Villalobos A., Schmidt KA., Deshpande A., Castillo LD., Fike J., Walter MR., Barry PA., Hartigan-O'Connor DJ. Neutralization of rhesus cytomegalovirus IL-10 reduces horizontal transmission and alters long-term immunity. // Proc Natl Acad Sci USA - 2021 - Vol116 - N26 - p.13036-13041; PMID:31189602
- Lee DS., Ruiz-Lambides AV., Higham JP. Higher offspring mortality with short interbirth intervals in free-ranging rhesus macaques. // Proc Natl Acad Sci USA - 2021 - Vol116 - N13 - p.6057-6062; PMID:30877247
- Aljuhaysh RM., El-Fetoh NMA., Alanazi MI., Albaqawi AS., Alanazi WM., Alanazi NS., Alanazi RM., Alanazi AM., Alnemer EM., Alenezi RA., Alabdullatif TK., Alanazi RA., Alanazi SS., Alsultan KS., Alanazi IM., Alsunayni DS. Maternal-fetal Rhesus (Rh) factor incompatibility in Arar, northern Saudi Arabia. // Electron Physician - 2021 - Vol9 - N12 - p.5908-5913; PMID:29560141
- Bishop CV., Stouffer RL., Takahashi DL., Mishler EC., Wilcox MC., Slayden OD., True CA. Chronic hyperandrogenemia and western-style diet beginning at puberty reduces fertility and increases metabolic dysfunction during pregnancy in young adult, female macaques. // Hum Reprod - 2021 - Vol33 - N4 - p.694-705; PMID:29401269
- Krendl C., Shaposhnikov D., Rishko V., Ori C., Ziegenhain C., Sass S., Simon L., Müller NS., Straub T., Brooks KE., Chavez SL., Enard W., Theis FJ ., Drukker M. GATA2/3-TFAP2A/C transcription factor network couples human pluripotent stem cell differentiation to trophectoderm with repression of pluripotency. // Proc Natl Acad Sci USA - 2021 - Vol114 - N45 - p.E9579-E9588; PMID:29078328
- Dettmer AM, Woodward RA, Suomi SJ. Reproductive consequences of a matrilineal overthrow in rhesus monkeys. // Am J Primatol - 2015 - Vol77 - N3 - p.346-52; PMID:25382028
- Dizik GM., Pavliuk RP. . // Klin Khir - 2011 - Vol - N9 - p.69-72; PMID:22168031
Rh factor and pregnancy
Compatibility of Rh factors during pregnancy is one of the tests that is carried out in the antenatal clinic. When a woman registers with a gynecologist, she will need to donate blood to determine her group and Rh factor. It can significantly affect the course of the next nine months. If the baby inherits the positive Rh of the father, and the mother has a negative Rh, then the protein in the child’s blood is unfamiliar to the mother’s body. The mother's body "considers" the baby's blood a foreign substance and begins to produce antibodies, attacking the baby's blood cells. If there is a Rhesus conflict during pregnancy, the fetus may experience anemia, jaundice, reticulocytosis, erythroblastosis, hydrops fetalis and edematous syndrome of the newborn (in the latter two cases there is a high probability of death of the child).
How does the Rh factor of parents affect the child?
It is known that if a woman has a Rh factor of “-” and a man has a Rh factor of “+,” then a serological conflict arises.
How does the Rh factor affect the unborn child?
Serological conflict is a disorder primarily affecting women with the Rh- blood type who have children with an Rh+ male. This phenomenon causes hemolytic disease of the fetus or newborn. The essence of the problem lies in the mother's production of antibodies that destroy the fetus's red blood cells. This leads to anemia and many other serious complications.
It should be noted that a serological conflict rarely occurs during the first pregnancy, since the mother's immune system does not yet produce antibodies to the Rh factor.
Rh conflict during pregnancy appears no earlier than 16 weeks after conception. If antibodies are not detected by 20 weeks of pregnancy, they are unlikely to appear.
Rhesus - conflict resembles a mechanism of defense against viruses, when resistance is formed by the immune system to destroy the “enemy”. While in the case of pathogenic microorganisms the phenomenon has a beneficial effect, in the case of a serological conflict the effect is completely opposite, since it causes pathological conditions in the child.
As a result of inheritance, the fetus receives antigenic characteristics from both the mother and the father. During pregnancy, due to the penetration of fetal blood cells into the mother's blood circulation with the antigenic characteristics of the father (which the mother does not have), the mother begins to produce antibodies directed against these antigens.
The most famous and important example of serological conflict is the difference in Rh cell antigens in the fetus and mother. The formation of antibodies in a woman's circulation occurs when the fetus inherits the father's "D" (Rh+) antigen and the mother has the "d" (Rh–) antigen.
The resulting antibodies to the Rh factor enter the baby's circulation and cause damage to blood cells, leading to hemolytic disease.
The mildest form of hemolytic disease is the destruction of a child's blood cells. The child is born with anemia, which is usually accompanied by an enlarged spleen and liver, but this does not pose a threat to his life. Over time, the blood picture improves significantly and the child develops correctly. However, it should be emphasized that in some cases anemia is severe and requires special treatment.
Neonatal jaundice is another form of hemolytic disease. The baby looks quite healthy, but on the first day after birth, a jaundiced color of the skin begins to appear. There is a very rapid increase in bilirubin, which has a toxic effect on the child’s brain and liver.
The final and most serious form of hemolytic disease of the newborn is generalized fetal edema. As a result of the destruction of the baby's blood cells by the mother's antibodies (still at the stage of intrauterine life), blood circulation is disrupted and vascular permeability increases. What does it mean? Fluid from the blood vessels leaks into nearby tissues, causing internal swelling to form in important organs, such as the peritoneum or the pericardial sac that surrounds the heart. Unfortunately, edema is such a serious pathological condition that it usually leads to the death of the child in the womb or immediately after birth.
Blood type and Rh factor: compatibility
The cause of incompatibility may be not only Rh blood type, but also blood type.
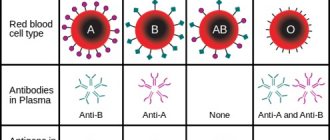
What are the different blood types? They are distinguished by the presence of specific proteins.
Four groups:
- the first (occurs most often) - O - there are no specific proteins in it;
- the second - A - contains protein A;
- the third - B - contains protein B;
- the fourth (the rarest of all) - AB - contains both type A and type B proteins.
First
(Rh negative) can provoke a conflict in the mother:
- for protein of the second group (A);
- for protein of the third group (B);
- for Rh protein (positive).
Second
(Rh negative) can provoke a conflict in the mother:
- for protein of the third group (B);
- for protein of the fourth group (B);
- for Rh protein (positive).
Third
(Rh factor is negative) the mother can provoke a conflict:
- for protein of the second group (A);
- for protein of the fourth group (A);
- for Rh protein (positive).
Fourth
does not conflict with any other group. The only case when an immune reaction is possible is if the mother has group IV and is Rh negative, and the father is positive.
Table 1. Statistics
| Blood groups parents | Possible blood type of the child (probability, %) | |||
| I+I | I (100%) | — | — | — |
| I+II | I (50%) | II (50%) | — | — |
| I+III | I (50%) | — | III (50%) | — |
| I+IV | — | II (50%) | III (50%) | — |
| II+II | I (25%) | II (75%) | — | — |
| II + III | I (25%) | II (25%) | III (25%) | IV (25%) |
| II + IV | — | II (50%) | III (25%) | IV (25%) |
| III+III | I (25%) | — | III (75%) | — |
| III + IV | — | II (25%) | III (50%) | IV (25%) |
| IV + IV | — | II (25%) | III (25%) | IV (50%) |
What blood type will the child have?
The topic for this article was suggested to us by our patients asking a question about their child’s blood type.
Very often this question is asked by young couples who want to have healthy children in order to find out about the possible risks in the presence of hereditary diseases, what the child’s blood type may be, and whether there is a possibility of developing an Rh conflict. In the international classification, it is these two indicators (blood type and Rh factor) that are most important. Every person needs to know their blood data in case of a possible emergency and the need for a donor blood transfusion, because not every blood is compatible. Blood type is an inherited trait that does not change throughout life. The most common system for dividing blood into groups is the AB0 system. Depending on the presence of certain proteins on the surface of red blood cells, called aglutinogens, and proteins found in the plasma - aglutinins, four blood groups are distinguished: 0 (zero) - first, A - second, B - third and AB - fourth. It is this system that is used to select blood during transfusion. However, having received the parental genes, the child, unexpectedly for the parents, may have a different blood type.
Division into blood groups
On what basis is human blood divided into four groups? In this case, the same genetic principles of inheritance, developed by Gregor Mendel back in 1866, apply. According to his theory, a person receives from each parent his own version of development for each characteristic: eye color, hair, nose shape, body type. One of them remains the main one - dominant, the second is suppressed and becomes recessive. But both exist in a person's genetic makeup, and either one can be inherited by a child.
It turns out that human red blood cells have special antigens on their surface, called A and B, and depending on how these genes are distributed and which one will dominate, the child’s blood type depends.
Inheritance of blood type from parents
According to recognized standards, blood groups are designated by a Roman numeral and the letter of the dominant antigen: I(0);
II(A); III(B); IV(AB). But, according to the laws of genetics, every person also has a recessive (suppressed) trait. It may be in the same literal expression as the dominant one, or it may be the opposite. For example: a person with the second blood group may have Aa antigens, where the first A is dominant, the second a is recessive. A may have Ab, where the first A is a dominant, determining his existing blood type, and b is a suppressed trait that does not manifest itself in any way.
But, it can be inherited and appear in the offspring if it encounters a recessive trait similar to itself. So what kind of blood inheritance will the future child receive?
It turns out that for heirs there are often several options for blood groups, and the greatest number of them are among those whose parents have the first or fourth blood group. The blood type of a child according to his parents is calculated by the laws of inheritance; according to the same laws, there are impossible options: - One of the partners has the fourth blood group, in this family a baby with the first group will never be born, regardless of the blood type of the second parent. - If, on the contrary, one of the parents has the first blood group, this family will never have children with the 4th blood group. However, exceptions are always possible. In 1952, a case was described when in an Indian family, where the parents had blood group IV, a child was born with blood group I. It turned out that the baby does not have the H antigen, the precursor of antigens A and B. This blood belongs to the first group, but in fact cannot be considered as such, since the H antigen is present in all four groups. Such blood can rather be classified as a phenomenon; such cases are quite rare. The bulk of them are residents of the Negroid race. There are other cases when the child’s blood type does not match the parents’, but this is a completely natural result of mixing the 2nd group and the 3rd. This is a unique variation in which children can have any blood type. The table clearly demonstrates the possible blood groups of a child.
Thus:
Parents with the first blood group can only have a child with the first group. Parents with the second have a child with the first or second. Parents with the third have a child with the first or third. Parents with the first and second have a child with the first or second. Parents with the first and third have a child with the first or third. Parents with the second and third have a child with any blood group. Parents with the first and fourth have a child with the second and third. Parents with the second and fourth have a child with the second, third and fourth. Parents with the third and fourth have a child with the second, third and fourth. Parents with the fourth have a child with the second, third and fourth. If one of the parents has the first blood group, the child cannot have the fourth. And vice versa - if one of the parents has a fourth, the child cannot have a first. Antigen B matures by the age of one year, so it is sometimes not detected at birth. As a result, a child with the third blood group may receive the first blood group at birth, while a child with the fourth may receive the second. By the age of one year, the antigen matures and the blood type changes.
Blood division system based on Rh factor
Another classification that is of utmost importance is the Rh factor. Blood rhesus is a protein compound found on the membranes of red blood cells. Its purpose in the body is not entirely clear, however, about 85% of the world's population has this protein as part of cell membranes. This population is called Rh-positive, those percentages that do not have it are, accordingly, Rh-negative.
A married couple, thinking about procreation, must definitely check the presence or, on the contrary, absence of this protein in each of the spouses. This is important, since a discrepancy between the maternal and fetal blood according to the Rh factor can lead to the death of the child. A woman’s immune system perceives the Rh protein of the unborn baby as an antigen that causes an allergic reaction and reacts to it by producing antibodies. Penetrating through the placental barrier, these antibodies cause destructive processes in the body of the developing fetus. However, all of the above is true for an Rh-negative mother and an Rh-positive baby. If the mother is Rh+ and the baby is Rh-, there is no conflict. Therefore, examination and blood test for Rh factor is mandatory for a pregnant woman. Rh protein is passed on to the child according to the same general rules of genetic inheritance. In most people, factor D (the presence of protein) is dominant, and factor d (its absence) is recessive.
Inheritance of Rh factor
· The most common situation is DD + DD, in this case there is no threat to pregnancy
· With the option DD + Dd, there will also be no problems from the Rh protein · The situation Dd + Dd is risky, but percentage-wise safer than the next one · Dd + dd, here a Rh conflict occurs in half of the cases. Whether a child will inherit the presence of Rh protein, and what blood type the child will have, depends on what genes the parents pass on to him. Moreover, both dominant and recessive genes play an important role.
In conclusion:
It would seem that everything has already been clarified, but questions always remain.
For example, can blood types change during life? There is no documentary data or official research on this topic. It is believed that blood is genetic material laid down at the beginning of intrauterine development, and its indicators are unchanged. However, there is evidence that some infectious diseases can cause changes in the general blood picture, which leads to the establishment of a false analysis. There is a temporary change in blood type. Similar cases of blood type changes are sometimes observed in pregnant women. What if the child's blood type does not match the parents? On this issue, it is best to consult a specialized doctor.
Rh positive during pregnancy
If you are Rh positive, then your husband’s Rh negative will not affect the course of your pregnancy. In the case when a child inherits a negative Rh factor, there is no protein in his blood that is “unfamiliar” to the mother’s immune system, and a conflict will not arise.
- Rh-positive mother + Rh-positive father = Rh-positive fetus
The child has inherited the positive Rh factor of the parents, and the pregnancy will pass without complications. - Rh-positive mother + Rh-positive father = Rh-negative fetus
Even if the parents' Rh factor is positive, the baby can be negative. In this case, we can still talk about the compatibility of Rh factors during pregnancy: the mother’s body is “familiar” with all the proteins in the child’s blood. - Rh-positive mother + Rh-negative father = Rh-positive fetus
Both the mother and the fetus are positive, and there is no conflict during pregnancy. - Rh-positive mother + Rh-negative father = Rh-negative fetus
Although mother and fetus have different Rh blood factors (mother and child have positive and negative, respectively), there is no conflict.
As already mentioned, Rh blood is a protein. And since the mother’s body already has this protein, the fetal blood does not contain components unfamiliar to the mother’s immune system.
Can incompatibility be cured?
Unfortunately, treatment of incompatibility is impossible, but, nevertheless, even with such a diagnosis there is a chance to carry and give birth to a healthy child.
The most important thing is the prevention of serological conflict and its early diagnosis. The expectant mother should be closely monitored by a doctor to undergo blood tests every few weeks, check antibody levels and check the intrauterine development of the fetus using ultrasound.
Most gynecologists, when identifying this phenomenon, prescribe the use of anti-D-immunoglobulin, which is administered by injection between 28 and 32 weeks of pregnancy, which increases the likelihood of avoiding the consequences of the conflict. A repeat dose is given 72 hours before the baby is born. After this time, the anti-D immunoglobulin vaccine will no longer serve its purpose. Administration of immunoglobulin during the first pregnancy often saves the life of the second child. The vaccine is also given after a miscarriage, abortion, amniocentesis, cesarean section, or bleeding during labor.
Rh factor negative during pregnancy
Rh negative during pregnancy is not always a death sentence for the baby. The main thing is that it is the same for both the baby and the mother.
- Rh-negative mother + Rh-negative father = Rh-negative fetus
The baby inherited the Rh factor of his parents. And since both the mother and the fetus have no protein (Rhesus) in their blood and their blood is similar, then a conflict does not arise. - Rh-negative mother + Rh-positive father = Rh-negative fetus
This is one of the cases when the Rh factor is very important: the compatibility of the blood of the mother and the fetus affects the next nine months of intrauterine life. Although a woman is Rh negative during pregnancy, it is good that the fetus is also Rh negative. There is no Rh in either the mother's blood or the fetus's blood.
Let's sum it up
When conceiving a child, the compatibility of the parents according to the Rh factor does not matter, but this is one of the important criteria that affects the successful course of pregnancy. Therefore, it is so important to thoroughly prepare the female body for bearing a child.
Pregnoton, which contains folic acid, iodine, vitamins E, C, B6, and zinc, will help with this. It eliminates the lack of micronutrients important for conception and early pregnancy, and also normalizes the functioning of the reproductive system, reduces prolactin levels in hyperprolactinemia, increases the thickness of the endometrium in women with thin endometrium and increases the likelihood of pregnancy (more information about the product can be found here).
THIS IS NOT AN ADVERTISING. THE MATERIAL WAS PREPARED WITH THE PARTICIPATION OF EXPERTS.
When does Rh-conflict pregnancy occur?
Rh negative mother + Rh positive father = Rh positive fetus
Please note: no matter what group the mother has, negative Rh during pregnancy becomes a cause of conflict. In this case, the embryo inherits it from the father and brings the “new protein” into the body of the Rh-negative mother. Her blood “does not recognize” this substance: there is no such protein in the body. Accordingly, the body begins to defend itself and produce antibodies. They penetrate the placenta into the baby's blood and attack his red blood cells. The fetus tries to defend itself: the spleen and liver begin to work hard, and they increase significantly in size. If a child has few red blood cells left, he develops anemia, or anemia.
What difficulties might you encounter?
Rh conflict is possible in a situation where a woman with negative blood is carrying a positive child. In this case, there is a high probability of hemolytic disease of the fetus. This pathology progresses in stages.
First, the person is immunized. The expectant mother acquires immunity, which must fight foreign bodies. The placenta is considered an effective barrier, but there is still a risk of the baby's red blood cells entering the woman's circulatory system. The body immediately reacts by producing IgM antibodies. They are not able to cross the placenta, and therefore do not lead to the development of hemolytic disease. At the same time, antibodies increase the sensitivity of the expectant mother’s immunity. They are intensively produced during repeated penetration of red blood cells. IgG antibodies appear in the blood, which quickly cross the placenta and lead to the breakdown of the baby’s red blood cells.
For the process of sensitization to develop, it will be enough that 0.05 ml of the fetus enters the woman’s bloodstream. With each subsequent pregnancy, the risk of immunization increases significantly. After each birth of a baby, it increases by 10%. For this reason, it is important to preserve the first pregnancy and carry out preventive measures.
The likelihood of sensitization increases in the following situations:
- Pregnancy outside the uterine cavity.
- Spontaneous or induced abortion after 8 weeks.
- Detachment of placental tissue after the birth of a child, threat of termination of pregnancy.
- Negative changes in the placenta of the chronic type.
- Premature placental abruption in the last weeks of gestation.
- Difficult childbirth, which ends in operations and injuries.
The second stage of hemolytic disease is the penetration of antibodies from an adult through the placenta into the child’s bloodstream. For most mothers, this percentage is observed no earlier than 18-20 weeks. It occurs due to placental insufficiency. The risks increase as the time of delivery approaches. Antibodies can enter the fetal bloodstream during delivery. In this situation, the child will develop fully throughout pregnancy. The disease will appear only after birth.
Rarely, antibodies do not cross the placenta, and immunized women give birth to a healthy baby. Expectant mothers should not count on a positive outcome, since if the outcome is unfavorable, they will have to take care of prevention.
At the third stage, antibodies begin to act on the fetus. Having penetrated the child’s bloodstream, they attach to the surface of red blood cells, provoking destruction. In this regard, a significant percentage of bilirubin is released, which colors the mucous membrane and dermis in a yellow tint. Bilirubin can enter the brain and cause encephalopathy. Generalized fetal edema may also develop. Pathology can lead to DIC syndrome, and it often causes the death of the fetus inside the womb.
Rh negative during pregnancy
There is a vaccine - anti-Rhesus immunoglobulin, which prevents Rh-conflict during pregnancy. It binds the antibodies that the mother’s body produces and brings them out. Vaccination can be carried out during pregnancy. If you are Rh negative and your husband is positive, this is not a reason to give up motherhood. Over the course of 40 weeks, you will have to donate blood from a vein several times:
- up to 32 weeks - once a month;
- from the 32nd to the 35th week - 2 times a month;
- from the 35th to the 40th week - once a week.
If Rh antibodies appear in your blood, your doctor can detect the onset of a Rh conflict in time. In case of conflict pregnancy, immediately after birth, the newborn is given a blood transfusion: the group and Rh factor must be the same as that of the mother. This is especially important in the first 36 hours of the baby’s life - the mother’s antibodies that enter the child’s body are neutralized when they “meet” familiar blood.
What to do if there is a Rh conflict?
If the expectant mother and fetus are threatened by the consequences of Rh conflict, she should be under constant medical supervision.
In addition to regular blood tests to assess antibody levels (the more, the worse for the baby), a pregnant woman with a serological conflict should constantly undergo ultrasound examination for any signs of hemolytic disease of the fetus. Ultrasound examination allows you to measure blood flow in the artery of the child’s brain and assess the condition of the amniotic fluid and placenta. If anemia is suspected, the doctor prescribes additional diagnostic measures, most often cordocentesis. This is an accurate and commonly used test to obtain cord blood. Under ultrasound control, the umbilical vessels are dissected using a thin needle, after which about 0.5-1 ml of blood is taken. Such a blood test answers the question of what degree of anemia we are dealing with and what kind of blood the fetus has. This study allows you to plan further procedures.
When can immunoglobulin prophylaxis be carried out?
To prevent conflict in subsequent pregnancies, women with a negative Rh factor should undergo prophylaxis. This is done after:
- childbirth (within three days);
- abortion;
- analysis of amniotic fluid;
- spontaneous miscarriage;
- ectopic pregnancy;
- placental abruption;
- transfusion.
Remember: if you and your baby’s group and Rh are different, this is not an indication that there will definitely be problems. Group and Rh are just the presence or absence of specific proteins in the blood. The reaction of the body and the development of pathologies in our time can be successfully controlled with the help of medications. Your attentiveness to your body, as well as an experienced doctor, will help you bear a healthy baby.
Question 2:
I have a negative Rh factor. I recently had an abortion. Will I be able to have children? Is there a chance that the baby will be sick during the next pregnancy?
Answer
: The presence of a negative Rh factor does not directly affect conception. During an abortion (if it was performed at 9-10 weeks of pregnancy), there was a possibility of sensitization of the body to the Rh factor. Before a planned pregnancy, it is advisable to do a blood test for the presence of antibodies to the Rh factor.
How do your chances of conceiving depend on your blood type?
Quite a lot is already known about the influence of blood groups, for example, on the likelihood of developing Alzheimer's disease, cancer, blood clots, etc. However, virtually nothing was known about the effect on fertility. And finally, thanks to the efforts of Turkish doctors, research has appeared in this area.
A study published last week found that men with type O are four times less likely to develop impotence compared to guys with other blood types. Experts from Ordu University in Turkey noted that blood type is as important a risk factor as smoking, excess weight, and high blood pressure. The reason is not clear, but scientists have said that in people with type A blood, the penis has a large number of veins, the lining of which can become damaged, leading to erectile dysfunction.
Blood type also affects female fertility. Girls with the second group are more likely to bear a healthy child for a long time than with the first. Studies have shown that women in the first group quickly deplete their egg reserves early in life. But at the same time, women with type 0 have a lower risk of developing preeclampsia - high blood pressure during pregnancy, which can be dangerous for mother and baby.
Naturally, representatives of the rest of humanity (which, by the way, are a little more than half, because people of the 1st group account for a little more than 40%) should not panic either - a higher probability does not mean a 100% chance. Likewise, representatives of the “happy” group should not relax ahead of time - reduced risk does not mean zero.
Rh factor, blood group, blood protein, antibody production, anemia, immune reaction, Rh compatibility, anemia, hydrops, fetal edema, immunoglobulin
What are the consequences for mother and child?
For a pregnant woman, the development of a serological conflict does not threaten her in any way and does not affect her health in any way, which cannot be said about a child. A serological conflict can cause severe hemolytic disease (erythroblastosis fetalis), brain damage, hypoxia, and damage the central nervous system, liver and kidneys. For this reason, such a pregnancy requires careful medical monitoring.
Does blood group compatibility affect conception and gender of a child?
When planning a child, parents need to know their own blood type and Rh factor. This is important information that can affect both the course of pregnancy and the health of the unborn child.
Is blood group and Rh factor compatibility so important? The blood type itself (if you do not take into account the Rh factor) does not in any way affect the process of conception, the course of pregnancy or the gender of the child. In the practice of any reproductive specialist, there is more than one case where parents with different blood groups became parents of a healthy child.
Ideally, the Rh factor of both parents should match, otherwise there is a high risk of developing a serological conflict, when the mother’s body rejects the fetus as a foreign body.