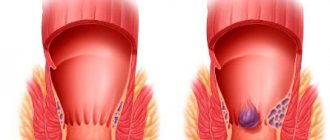
Banal hemorrhoids can cause serious discomfort. Enlarged venous nodes in the rectum cause a sensation of the presence of a foreign body and bleed. According to statistics, the described problem plagues every fourth inhabitant of the planet. There is also a modern treatment method - disarterization of hemorrhoids, which does not require surgical intervention. A minimally invasive technique can completely eliminate the problem without causing severe discomfort to the patient. Removal of hemorrhoids can be done without surgery!
About disarterization
Disarterization of internal hemorrhoids is a medical procedure that is used to treat proctological diseases. The treatment is also called hal rar. The technique does not require surgical intervention, which affects soft tissue.
The procedure is one of the most effective in the treatment of hemorrhoids; the risk of relapse after the procedure is reduced to zero. Sometimes, in parallel with disarterization, a tightening, so-called lifting, is performed. The therapy helps to strengthen the internal hemorrhoids. In the private proctology center “Proctologist 81”, surgical intervention is performed by doctors of the highest category who are able to cure the disease even at an advanced stage. Modern technical equipment is used to conduct research. The disease will be detected even in the early stages. Desarterization will eliminate the disease without affecting healthy tissue.
Most often, disarterization of hemorrhoids is performed under Doppler control. During the procedure, Doppler ultrasound is used. This method was developed back in the early 2000s, but is still popular today. For this purpose, a special surgical instrument is used, namely an anoscope, which has a built-in ultrasonic sensor.
During disarterization of hemorrhoids at the Proctologist 81 clinic, a medical specialist not only monitors the condition of the internal organs, but also diagnoses the sound of arterial pulsation. It is carried out both in the first and critical stages of hemorrhoids.
How to prepare for surgery
The main preparation consists of the patient undergoing an examination, which is prescribed by the doctor.
Before the operation, the patient undergoes an examination including:
- general blood test, biochemistry, Rh factor and group;
- analysis
- venous blood for hepatitis, HIV and a number of other diseases;
- electrocardiogram;
- fluorography.
If there are no contraindications to surgery, the doctor gives recommendations for preparation:
Compliance with the doctor’s recommendations will help to avoid difficulties during surgery and avoid complications in the postoperative period.
Performing disarterization of hemorrhoids with lifting
Before disarterization of hemorrhoids, the patient undergoes a comprehensive examination of the body. The proctologist conducts an initial examination, inserts a finger into the anus to find out the size of the hemorrhoids. Next, the patient is sent for a general blood, urine, and stool test. A blood test is taken to check glucose levels and the presence of viral and infectious diseases.
In advanced stages of hemorrhoids, the effect is produced by disarterization of hemorrhoids with mucopexy. Lifting allows not only to remove hemorrhoids, but also to tighten soft tissues that have been deformed.
Before the operation, the patient attends an examination with a proctologist. The medical examiner inserts into the anus to find out what size the hemorrhoids are. Next, the patient is sent for a general blood, urine, and stool test. It is advised to take a test for blood glucose levels and conduct research for the presence of viral infections in the body.
Computed tomography, ultrasound diagnostics, radiography using contrast fluid, electrocardiogram and other medical studies are performed. Proctologists advise following a strict diet before surgery. It is necessary to exclude from the diet foods that cause fermentation. We are talking about cabbage, legumes, and fermented milk products.
The diet should include cereals, broths, and plenty of drinking. Immediately before the procedure, the patient is given an enema to cleanse the intestines. The therapy is painless, there is no discomfort, as the person is immersed in medicated sleep. Intravenous sedation is administered. The injection is administered in the lumbar region. The painkiller takes effect almost immediately.
At the time of the procedure:
- The anal area is treated with disinfectants.
- The doctor inserts a surgical instrument called an anoscope into the rectum. There is an electronic sensor on the device. It provides information about the pulsation of hemorrhoidal arteries.
- The surgeon discovers a place that needs to be stitched. An ultrasonic sensor transmits information about the operation of damaged vessels. The vessels are stitched with a special thread, which is what the lifting procedure consists of.
- The vessels are stitched with a certain suture to interrupt the blood supply. Hemorrhoids are moved into the anus. This procedure prevents them from falling out.
- Two weeks after the operation, the tumors die and fall out of the anus. After surgery, bleeding no longer occurs. The growth of hemorrhoids has been stopped.
Immediately after the procedure, the patient goes home. Further inpatient treatment is not used.
It is worth noting that in advanced cases the procedure is ineffective. If the size of hemorrhoids exceeds three centimeters, then hemorrhoidectomy is performed, in which the lumps are removed along with the site of formation.
Postoperative period
The rehabilitation period begins immediately after completion of the operation. Since surgery involves the circulatory system, the patient is under the supervision of qualified medical personnel for the first 3-4 hours after the procedure.
To relieve pain, which cannot be avoided since the operation is performed rectally, analgesics are taken. Severe pain subsides after a few hours. The unpleasant symptoms will completely disappear after 3 days. If there are no complications, then after eliminating the discomfort the patient can lead a normal life.
In order to speed up tissue recovery, the development of complications or relapse, surgeons advise in the first month:
- eat liquid food;
- stick to four meals a day;
- all meat products are prepared by stewing;
- consume fiber in the form of vegetables, fruits and berries (certain types) and protein and plant foods;
- exclude the intake of any products that can provoke irritation of the walls and mucous membrane of the gastrointestinal tract;
- exclude fried and fatty foods;
- do not drink alcohol and stop smoking;
- drink more fluids;
- do not do enemas;
- do not take a hot bath or use a sauna;
- take laxatives;
- exclude sexual intercourse.
The surgeon will prescribe the necessary medications and also explain how to treat the operated area.
Recovery after disarterization
The proctologist prescribes analgesic and painkillers to the patient to relieve pain. A personalized diet is prescribed. During the rehabilitation period, it is also worth excluding legumes, vegetables, baked goods, and exotic fruits, which can slow down bowel function.
It is worth rinsing the anal area with warm water after each bowel movement. This is necessary in order to prevent the development of infection. Apply antiseptic medications to the affected area twice a day. Hot water irritates the rectal mucosa.
It is strictly forbidden to have sexual activity for a month after the operation. Anal sex can lead to bleeding and anal fissures. It is necessary to exclude physical activity and ensure complete rest.
During rehabilitation, it is recommended to visit the proctologist several times to avoid postoperative complications. During this period, the patient takes laxatives and uses Vaseline oil. As a rule, there are no complications after disarterization, but if any complaints appear, you should immediately consult your doctor.
Recommendations for nutrition after surgery. Relapses
When disarterization of hemorrhoids is performed, recovery takes at least 30 days. The patient should eat 4 times a day. You should not refuse food for fear of feeling pain in the toilet. Foods that cause bloating are prohibited, including legumes and dishes with hot spices. The diet should consist of proteins, fruits and vegetables. Meat should be consumed, but only boiled or baked. Be sure to drink a lot, especially water and juices. Alcohol and cigarettes are completely prohibited.
It is important to take medications that improve intestinal motility. For 30 days after surgery, physical activity is prohibited; lifting more than three kilograms is prohibited. Even if disarterization of hemorrhoids is performed correctly, relapses are observed in some patients. Severe bleeding, unbearable pain or fecal incontinence during the recovery period are reasons to immediately consult a proctologist.
After childbirth or from a sedentary lifestyle, many people develop hemorrhoids. The disease cannot be treated on its own or through traditional methods. After disarterization of hemorrhoids, a patient is able to recover within a month. This is the most gentle and effective method. The operation is painless, the only difficulty is the rehabilitation period. You must follow your doctor's instructions for successful healing. Contact the proctology center for qualified assistance.
Benefits of the procedure
Desarterization is one of the most popular medical procedures for the treatment of hemorrhoids. The operation is known for a number of advantages, including:
- Efficiency. The effect of the hal rar method appears immediately after the procedure. The bleeding stops, the hemorrhoids do not fall out, and their growth is stopped. The patient does not suffer from itching and burning in the anus. In addition, this procedure not only relieves the patient of pain, but eliminates the source of the disease and eliminates the cause of inflammation.
- Speed of the procedure. On average, the procedure lasts for an hour. The patient goes home on the same day. Conservative treatment continues.
- Comfortable carrying out. During disarterization, the patient is in medicated sleep, so there is no pain.
- Versatility. This treatment technique is called universal, since it is used in both the first and fourth stages of hemorrhoids. It is carried out even in the presence of fistulas and anal fissures.
- Safety. Desarterization has virtually no contraindications and is carried out for all age categories.
- Short-term rehabilitation. Rehabilitation is two weeks. Wounds heal quickly.
- No complications. In most cases, there are no complications after surgery. There are no scars or scars, as soft tissues are not damaged.
In addition, disarterization has a positive effect on reducing the flow of arterial blood to damaged vessels. Blood circulation in the veins improves. The size of internal and external hemorrhoids decreases.
Indications for disarterization
The main indication for disarterization is diagnosed hemorrhoids. The operation is performed during an inflammatory process affecting the venous sinuses with the subsequent development of internal and external hemorrhoids.
Desarterization is also effective for pathologies:
- thrombosis of rectal vessels;
- relapse after treatment;
- lack of effectiveness of conservative therapy.
The operation can be performed even if the nodes are small, if the disease has already become chronic. Before the procedure, the surgeon must conduct an examination and refer you for diagnostics.
How the manipulation is performed
Disarterization operation
takes place in the clinic without hospitalization of the patient. Before surgery, the person is put into deep sleep, and anesthetic drugs are injected into a vein or into the spinal canals. A disposable anoscope equipped with an ultrasound sensor is inserted into the rectum. After the coloproctologist surgeon has received a signal that hemorrhoidal arteries have been detected, he stitches them with special instruments with self-absorbing suture material.
hemorrhoidal arteries are stitched and ligated
: large, medium and small.
This is necessary in order to prevent relapse of the disease. During one procedure, the doctor stitches from 3 to 10 or more arteries. The duration of the manipulation depends on how many hemorrhoidal
arteries are identified. On average, the operation lasts 20–30 minutes, and after 6 hours the patient leaves the clinic.
Features of the technology
Local anesthesia is used . The specialist uses special tools to make a running stitch from the top of the hemorrhoidal growth to its main part. The fabric is compressed using a stitch.
Thanks to the anoscope, the prolapsed tissue of the node is collected. The expert ties the ends of the threads, tightens the knot and, through a continuous seam, “tightens” the tissue, achieving a lifting .
Restoring the normal position of the tissues allows you to preserve the functions of the rectum without traumatizing its mucosa.
Stages of hemorrhoids
The hemorrhoidal plexus is strengthened by the muscle tissue of the sphincter in the rectum. An increase in intra-abdominal pressure with strong pushing during bowel movements leads to increased blood flow through the hemorrhoidal arteries to the internal hemorrhoidal plexus, which begins to enlarge, turning into a knot. If too much pressure is applied to the rectum at the time of emptying (defecation), the supporting apparatus of the hemorrhoidal plexus is stretched and subsequently ruptures, and the internal hemorrhoidal node begins to fall out of the rectum. This symptom is called “prolapse,” or prolapse of hemorrhoids. Prolapse of nodes is often accompanied by bleeding of varying degrees. Enlargement of the hemorrhoidal plexus is classified into four stages, depending on their size and the nature of the manifestation of the disease.
Stage 1: Slight enlargement of the hemorrhoidal plexus
Stage II: The hemorrhoidal plexus prolapses, but resets itself after defecation
Stage III: The hemorrhoidal plexus prolapses and requires manual reduction after defecation.
Stage IV: Prolapse of hemorrhoids that cannot be reduced after defecation
Treatment of hemorrhoids
Stage I hemorrhoids require only conservative treatment.
Stages II and III of hemorrhoids can be treated both surgically (removal of nodes) and palliative methods (sclerotherapy or latex ligation), which requires multiple repetitions and has a high rate of disease relapse.
Stage IV hemorrhoids require surgical treatment. Any method of removing the hemorrhoidal plexus (hemorrhoidectomy operation) is associated with pain, regardless of what instruments are used to remove the nodes (ultrasonic scalpel, Liga-Sure device). In any case, post-operative wounds can be painful. The stay in a hospital bed ranges from seven to ten days.
The development of complications, regardless of the type of intervention after hemorrhoidectomy, occurs in 34-41% of patients. The average period of disability after hemorrhoidectomy is at least 4 weeks.
Many patients prefer to live with the problem of hemorrhoids rather than see a doctor.
“Now there is an alternative to traumatic methods of surgical treatment of hemorrhoids - the innovative HAL-RAR technology. Today this is the safest, most effective and least traumatic method of treatment at all stages of hemorrhoids.”
It is based on ligation of the hemorrhoidal arteries, the same ones that feed the hemorrhoidal node, under the control of Doppler ultrasound in combination with tightening-lifting of the hemorrhoidal nodes.
Introduction
Hemorrhoidal disease is widespread in industrialized countries of the world. Surgical intervention is the method of choice in the treatment of hemorrhoids, which do not respond to conservative therapy or various types of low-traumatic treatment. The “gold standard” for the treatment of hemorrhoidal disease is considered to be an operation aimed at eliminating the three main groups of hemorrhoids; it was introduced into surgical practice by E. Milligan and G. Morgan in 1937 [23]. The main disadvantage of the operation is severe pain and prolonged wound healing, which does not allow patients to return to work in a short time [17]. In 1995, K. Morinaga et al. [25] proposed a new technology for the treatment of hemorrhoids - transanal Doppler-controlled disarterization of internal hemorrhoids as an alternative to hemorrhoidectomy or stapled hemorrhoidopexy. While the treatment of patients with stage II hemorrhoids is highly effective [1, 7, 32], the technology turned out to be less effective in stages III and IV of the disease [4, 9, 26]. Analysis of treatment results indicates residual mucosal prolapse in 8% of patients with stage III hemorrhoids [4, 9, 26] and in approximately 50% of patients with stage IV hemorrhoids [32].
In order to overcome this drawback of the method, it was proposed to supplement the operation with mucopexy. In this case, the principle of mucoplication of dilated internal hemorrhoidal tissue was used, based on the proposal of A. Farag [8] and the mucopexy technique developed by A. Hussein et al. [14], and the method of suturing was changed [33]. By combining the disarterization technique with mucopexy, a technology emerged called HAL-RAR (hemorrhoidal artery ligation with transanal repair mukopexy) - ligation of hemorrhoidal arteries with mucopexy. A change in surgical technology required the development of a new proctoscope and a special attachment for lifting the mucosa. Since 2006, technology has been used in the treatment of patients with stage III and IV hemorrhoids. We report on the long-term results of using HAL-RAR technology in the treatment of patients with stage III and IV hemorrhoids.
Material and methods
From January 2007 to August 2008, 180 patients with chronic hemorrhoids were treated at the ON CLINIC medical center. Stage III of the disease was in 128 (71.1%), stage IV - in 52 (28.9%) patients. The age of patients ranged from 18 to 68 years (average 43.8±9.13 years). There were 128 men (71.7%) and 52 women (28.9%). The duration of the disease is from 2 to 20 years (average 9.14±4.26 years). Clinical signs of the disease in patients included in the analysis are presented in Table. 1.
Of the 180 patients who underwent transanal disarterization with mucopexy, 22 (12.3%) had previously undergone minimally invasive treatment that did not lead to a final cure: sclerotherapy - 5 (2.8%), ligation of internal hemorrhoids with latex rings - 12 ( 6.7%), infrared photocoagulation - 3 (1.7%), transanal disarterization (HAL) - 2 (1.1%). Hemorrhoidectomy was previously performed in 2 (1.1%) patients. 2 (1.1%) patients had previously undergone excision of anal fissure. When performing transanal Doppler-controlled disarterization of internal hemorrhoids with mucopexy, the HAL-Doppler-II device from AMI (Austria) was used. Treatment was carried out on an outpatient basis in a one-day hospital setting. All operations were performed according to the method described in our previous work [2], using a combination of deep sedation with propofol and posterior perianal block according to P. Nystrom et al. [27]. Disease symptoms were assessed using a structured questionnaire [11]. The questionnaire survey included the following signs of the disease: bleeding, prolapse of internal hemorrhoids, pain, itching, mucus discharge. A questionnaire was conducted before surgery and at each follow-up examination after surgery. The degree of prolapse of internal hemorrhoids was assessed based on examination and anoscopy. Signs of incontinence were assessed using the Jorge-Wexner scale [18] on a scale from 1 to 20 points.
Statistical analysis
Statistical analysis was performed using SPSS (v. 11, Chicago, IL). Digital data corresponding to a normal distribution are presented as means with standard deviation. To compare treatment results, the Wilcoxon test for two dependent samples was used. The test result was considered significant at p<0.005.
Results and discussion
Long-term results of treatment were monitored after 1-2 years and 5 years. The average follow-up period was 42.9±8.9 months (36-60 months) for all 180 patients. Comparative treatment results are presented in table. 2 and 3.
After 12-24 months, prolapse corresponded to stages II and III of hemorrhoids. Elimination of prolapse in 6 (3.3%) cases required two sessions of sclerotherapy; in 2 (1.1%) cases hemorrhoidectomy of the solitary hemorrhoid was performed. In 4 (2.2%) cases, repeated disarterization with mucopexy (HAL-RAR) and excision of the external hemorrhoid was performed. After surgery, external hemorrhoids remained in 19 (10.6%) patients; in 6 (3.3%) cases this caused difficulties in performing hygienic procedures, which required excision of external hemorrhoids under local anesthesia.
40 months after surgery there were no bleedings in 160 (88.9%) patients. Periodic bleeding was observed in 11 (8.6%) patients with stage III and 6 (11.5%) patients with stage IV of the disease. The bleeding was insignificant and was observed against the background of periodic constipation, no more than once every 3-4 months.
During a questionnaire survey, 25 (13.8) patients complained of prolapse of internal hemorrhoids: 13 (10.1%) with stage III and 12 (23.0%) with stage IV of the disease. However, objective examination and anoscopy showed that true prolapse was present in 20 (11.1%) patients: 11 (8.6%) with stage III and 9 (17.3%) with stage IV of the disease. During anoscopy, the prolapse corresponded to stages I and II of internal hemorrhoids. The discrepancy between subjective complaints and data from objective examination and anoscopy is explained by the fact that patients do not distinguish between the prolapse of internal hemorrhoids and the presence of scarred external hemorrhoids. Enlarged external nodes were detected in 13 (7.2%) patients: 6 (4.7%) with stage III and 7 (13.5%) with stage IV of the disease. Prolapse in 9 (5.0%) patients was stopped by two sessions of sclerotherapy in combination with phlebotonic therapy with Detralex. In 11 cases conservative therapy was required. In 5 (2.8%) cases, enlarged external hemorrhoids were removed for cosmetic reasons. The nature of additional manipulations performed 12-24 and 40 months after surgery is presented in Table. 4.
After 40 months, pain syndrome occurred in 2 (3.8%) patients with stage IV, which is associated with the phenomena of cryptitis, which required only drug therapy. Itching and burning were noted by 4 (2.2%) patients with stages III and IV of hemorrhoids. Discharge from the anal canal was present in only 3 (1.7%) patients with stage IV hemorrhoids. When assessing signs of incontinence on the Jorge-Wexner scale, none of the patients we observed had scores higher than 3 points after surgery. Throughout the observation period, signs of incontinence did not progress. When comparing the clinical results of treatment after 24 and 40 months, there was no progression of disease symptoms, which was statistically significant (p>0.005; Table 5).
Hemorrhoidectomy is still considered the “gold standard” of treatment, based on the results of which all other treatment methods are evaluated. However, the incidence of postoperative complications with this type of treatment ranges from 10 to 15% [12].
Staple hemorrhoidopexy was developed by A. Longo [20] as a minimally invasive alternative to hemorrhoidectomy. In order to eliminate prolapse of the mucous membrane and hemorrhoidal tissue, a transverse incision of the mucous-submucosal layer between the ampulla of the rectum and the anal canal is used, followed by stitching of the rectal and anal mucosa over the anorectal ring using a circular stapler. Excision of the mucous membrane at the specified level involves the intersection of the terminal branches of the superior hemorrhoidal artery in order to block arterial blood flow from the cavernous tissue.
Randomized studies showed that pain was significantly less severe and the rehabilitation process was shorter than with standard hemorrhoidectomy [5, 19, 35]. However, more recent studies indicate an increase in the frequency of relapses of the disease requiring reoperation - hemorrhoidectomy. Publications over the past 10 years have reported fatal complications (development of rectovaginal fistulas, rectourethral fistulas, peritonitis) requiring colostomy, which does not occur with standard hemorrhoidectomy [6, 13, 15, 21, 24, 28, 29, 31]. Studies conducted in recent years show that the use of this technique does not allow achieving complete disarterization of the internal hemorrhoidal plexus, since the level of entry of the terminal branches of the superior rectal artery is below the level of intersection of the mucous-submucosal layer when applying a stapler, this explains the recurrence of the disease in the long term period [3].
Transanal Doppler-controlled disarterization is a low-traumatic treatment for hemorrhoidal disease due to the short rehabilitation period and the absence of complications that occur with stapled hemorrhoidopexy. The treatment technology is based on the modern concept of the development of hemorrhoidal disease. Doppler-guided ligation of the distal branches of the superior rectal artery reduces abnormal arterial inflow to the cavernous tissue of the internal hemorrhoidal plexus, allowing the cavernous tissue to return to normal size. However, in patients with stage III and IV hemorrhoids, this does not completely occur, since the supporting apparatus of the cavernous tissue is destroyed due to irreversible degenerative changes in the Parkes ligament and Treitz muscle.
Based on the experience of using HAL technology in 2005 [5], we expressed the opinion that it is necessary to apply mucaplication sutures in the presence of stage III and IV hemorrhoids in order to reduce the dilated cavernous tissue of the internal hemorrhoidal plexus, which allows fixing the plexus in a normal anatomical position. However, this was difficult to accomplish with the first generation proctoscope. Improvement of treatment methods contributed to the awareness of the need to combine disarterization with mucopexy, which required changes in the design of the surgical proctoscope and the creation of a special attachment for mucopexy and mucosal lifting. The first results of treatment indicate that the technique is actually low-traumatic, has a small number of complications and a short rehabilitation period [4, 9, 16, 22, 30, 36, 37]. The low invasiveness of the manipulation allows treatment to be carried out on an outpatient basis or in a one-day hospital setting [2, 34, 36, 38]. By January 2008, we had 10 months of experience in treating 85 patients with stage III and IV hemorrhoids [38]. Early treatment results showed that a true relapse of disease symptoms was observed in 2 (2.4%) patients and was relieved with sclerotherapy.
In 6 (7.1%) patients, swelling of the external nodes was noted, which was perceived by patients as prolapse of the internal nodes. Due to the fact that the swelling of the external nodes interfered with hygiene, they were removed under local anesthesia; the patients had no further complaints. To date, there is only one publication in the literature based on the mid-term results of treatment of 100 patients with stage IV hemorrhoids using the HAL-RAR technology [10], which indicates the high effectiveness of the method. In the long-term follow-up period, 9% of relapses were detected, which required a repeat HAL-RAR procedure in 3 cases, Milligan-Morgan hemorrhoidectomy in 3 cases, and conservative measures in 3 cases.
To date, we have experience in treating 180 patients, with the duration of observation ranging from 30 to 60 months (42.9±8.9 months). Analysis of treatment results indicates the effectiveness of the operation with long-term follow-up. There were no symptoms of the disease in 160 (88.9%) patients: with stage III - in 117 (91.4%) and with stage IV disease - in 43 (82.7%). The main symptoms of the disease, such as bleeding, were absent in 163 (90.6%) patients: in 117 (91.4%) with stage III and in 46 (88.5%) with stage IV of the disease. Prolapse of internal hemorrhoids was not observed in 160 (88.9%) patients: in 117 (91.4%) with stage III hemorrhoids and in 43 (82.7%) with stage IV hemorrhoids.
Relapses of the disease that occurred during the first 2 years are associated with the period of mastering the technique. Prolapse of the internal nodes was eliminated using a repeat operation HAL-RAR, hemorrhoidectomy of the solitary hemorrhoid and sclerotherapy. A subsequent observation period of 30-60 months showed that prolapse of internal nodes, observed in 20 (11.1%) patients, corresponded to stages I and II of hemorrhoids. Sclerosing and phlebotonic therapy in combination with the normalization of intestinal function made it possible to eliminate this condition.
Subsequently, the patients had no complaints. Observation of patients who underwent manipulation indicates a significant reduction in external nodes after the first stage; mucopexy in most cases allows for complete reduction of the anoderm into the anal canal. In some situations, the hope of reducing significantly enlarged and scarred external hemorrhoids into the anal canal is futile, which requires limited removal of the scarred anoderm. A control study after 3-4 months reveals scar tissue in the area where disarterization and mucopexy were performed, which does not allow the plexus to move. Desarterization with mucopexy significantly reduces, but never completely blocks, arterial blood flow to the hemorrhoidal cushions. The scar tissue that occurs around the ligated arterial branch prevents the artery from dilating, thus preventing abnormal arterial inflow. Preservation of arterial inflow does not cause postoperative necrosis in hemorrhoidal tissue. This explains the preservation of the holding function. None of the patients we observed showed signs of incontinence, since the hemorrhoidal plexuses remain in a normal anatomical position, maintaining the function of holding. This is confirmed by studies by P. Walega et al. [37].
The use of technology allowed us to formulate a concept for the treatment of hemorrhoidal disease stages III and IV. Existing classifications of hemorrhoids do not reflect the changes occurring in the system of internal and external hemorrhoidal plexus. This is due to the characteristics of arterial blood flow, the number of arteries supplying blood to the cavernous tissue, and the degree of their dilatation [3], as well as the degree of degenerative changes in the Treitz muscle and Parkes ligament. Preoperative assessment of local status, based on examination, exploration and anoscopy, may change during anesthesia. One or two internal hemorrhoids may correspond to one stage of the disease, and the third node to another stage.
The classification does not reflect the degree of changes in the external hemorrhoidal plexus; this is especially important in a situation in which their circular enlargement is detected. In this regard, in our opinion, standard hemorrhoidectomy in three segments is unjustified, and manipulation should begin with disarterization of the cavernous tissue and performing mucopexy, which will block the pathological arterial inflow into the tissue of the internal hemorrhoidal plexus.
Carrying out segmental mucopexy will make it possible to return the cavernous tissue to its normal anatomical position. After completion of the manipulation, the size of the enlarged external hemorrhoids is significantly reduced, which either will not require their removal, or will require the removal of only the most enlarged scar tissue in a certain segment of the perianal region in order to preserve the anoderm of the anal canal as much as possible intact.
The fact that external nodes or hemorrhoidal fimbria remain after the manipulation should not be regarded as an ineffective result. If necessary, they can be removed immediately or after 3-4 months. Other experts share the same opinion [30, 36]. The purpose of disarterization and mucopexy is to restore normal arterial blood flow and the position of the internal hemorrhoidal plexus.
Thus, transanal Doppler-controlled disarterization of internal hemorrhoids with mucopexy and mucosal lifting (HAL-RAR) is a minimally invasive alternative to the standard surgical treatment of stage III and IV hemorrhoidal disease. The first mid-term and long-term results of treatment indicate the high effectiveness of the technique for hemorrhoids of stages III and IV. However, we plan to continue the study over a longer period, and also consider it advisable to conduct prospective multicenter randomized studies to obtain more objective results.