One of the innovative procedures in the field of hemorrhoid treatment is laser surgery. Its effectiveness has already been noticed by surgeons. Laser removal of hemorrhoids is a virtually painless procedure. The laser beam is selective and does not harm healthy tissues that are located next to damaged ones.
Rice. 1. With hemorrhoids, internal and external hemorrhoids appear.
The essence of laser treatment:
A laser beam is created by converting electrical energy into electromagnetic energy in the optical range.
The latest solid state technology is used. To enable the surgeon to see the laser beam (since the beam itself is colorless), red light is added to it. The laser beam now passes through a series of mirrors to a handpiece that the surgeon uses. Our high-tech laser uses two modes: a narrow beam for cutting and a wide-angle beam for vaporizing tissue. In evaporation mode, the laser beam simply vaporizes the hemorrhoidal tissue. This cannot be done with surgical scissors. In cutting mode, the beam compacts and coagulates (cauterizes) which is much gentler than surgical scissors or a scalpel, and the beam only penetrates a small portion of the tissue so it does not damage underlying structures.
For this reason, hemorrhoids can be treated with laser, more completely, but without damaging the tissues and underlying structures (the anal sphincter muscles, which is most important to avoid their damage with classical techniques, which can lead to fecal incontinence).
Causes of hemorrhoids
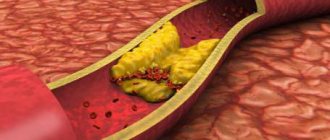
A predisposing factor to the development of the disease is impaired circulation of the venous plexuses. As a result, dystrophy develops in the muscles, connective tissue surrounding the nodes, as well as inside the anal canal. Frequent constipation or diarrhea, a sedentary lifestyle, consumption of foods containing seasonings, and alcohol contribute to the disease.
There are occupational factors, one of which is being constantly in a sitting position. Some sports – cycling, horseback riding – contribute to poor circulation. Women suffer from hemorrhoids due to frequent childbirth.
Stages of hemorrhoids
Hemorrhoids can be acute or chronic. In addition, experts spill hemorrhoids:
- interior;
- outer;
- combined.
Chronic hemorrhoids have 4 stages.
The first stage - scarlet blood is periodically released from the anus, hemorrhoids do not fall out.
The second stage - the nodes periodically fall out and are set back on their own, bleeding does not always occur.
The third stage - the nodes fall out, but they can be set on their own.
The fourth stage is characterized by the inability to independently reduce hemorrhoids.
How is laser treatment for hemorrhoids performed?
Laser hemorrhoid removal - laser hemorrhoidoplasty (LHP) - is essentially a minor operation performed on an outpatient basis and does not require hospitalization.
Anesthesia (anesthesia) is performed depending on the choice of treatment tactics and can be represented by general intravenous anesthesia, spinal anesthesia, or other methods of drug sleep. For this reason, laser can safely treat hemorrhoids in patients even with certain risk factors. The operation has virtually no contraindications.
During the operation, hemorrhoids are removed (evaporated) using a laser. By excising and removing the hemorrhoid, the laser beam immediately stops possible bleeding from small vessels, so sutures are not used. Laser techniques for removing hemorrhoids completely eliminate the risk of damage to the sphincter muscles. When choosing this technique, complications are excluded in which the patient could not control stool or gases after laser surgery.
Sometimes internal and external hemorrhoids are separated by a “bridge” of perianal skin. In this case, we will evaporate (vaporize) the internal hemorrhoids using a wide-angle laser beam and remove the external hemorrhoids using a cutting beam. This gives us a greater breadth of surgical action, which is not available with surgical removal of hemorrhoids.
Now you can understand that laser removal of hemorrhoids is much safer and less invasive than the classical hemorrhoidectomy methods currently used.
Minimally invasive / low-traumatic technologies in the treatment of hemorrhoidal disease
Hemorrhoids (from ancient Greek αἷµα - “blood” and ῥοῦς (< ῥόος) - “flow”) is a disease associated with thrombosis, inflammation, pathological expansion and tortuosity of hemorrhoidal veins that form nodes around the rectum. According to statistics, about 15% of the entire world population suffers from hemorrhoids. The prevalence of the disease is 140-160 people per 1000 adults, and its share in the structure of colon diseases ranges from 34 to 41%. An impressive figure, isn't it? And only about half of these “lucky” ones go to the doctor in the early stages of the development of the pathology. The rest are saving their time, hoping for “maybe”, or do not want to notice the annoying symptoms of the disease at all. In vain.
According to statistics, about 15% of the entire world population suffers from hemorrhoids
Causes of hemorrhoids
- gastrointestinal disorders
- errors in diet
- alcohol abuse
- sedentary and sedentary lifestyle
- pregnancy and childbirth
Hemorrhoids: symptoms and signs
Prolapse of internal hemorrhoids from the anus during defecation, discharge of blood from the anus during defecation (admixture of scarlet blood in the stool, discharge of blood in the form of drops or streams) Rarer symptoms include (or occur more often in later stages):
- feeling of discomfort
- feeling of incomplete bowel movement
- moisture in the anus
- itching, burning in the anus
- mucous discharge from the rectum
Remember! The main symptoms of acute hemorrhoids include: pain in the anus and rectum
- the appearance of a dense, painful formation(s) in the area of external and/or internal hemorrhoids
- profuse copious discharge of blood from the rectum, which does not stop with the help of conservative measures
Stages of the disease
Stage 1 – Discomfort and bleeding during bowel movements, no prolapse of nodes.
Stage 2 – stage 1 + periodic loss of nodes. The nodes recede on their own, mucous discharge, weeping and itching appear.
Stage 3 – stage 2 + but manual reduction of nodes is required
Stage 4 – Stage 3 insufficiency of the anal sphincter, severe weeping and itching, constant prolapse of the nodes, reduction is not possible.
How is hemorrhoids treated at the Grand Medica clinic?
To diagnose hemorrhoids at the initial consultation, the coloproctologist performs a visual examination, digital examination, anoscopy and, if indicated, sigmoidoscopy (painless instrumental examinations).
Most patients with stage 1–3 internal hemorrhoids, if conservative therapy is ineffective or insufficiently effective, are advised to perform minimally invasive surgical treatment methods:
- sclerotherapy
- infrared photocoagulation
- ligation of hemorrhoids with latex rings
- disarterization of hemorrhoids under ultrasound Doppler control and disarterization of hemorrhoids with mucopexy (according to the HAL-RAR method)
- traditional hemorrhoidectomy
Sclerotherapy
The method involves solving the problem of hemorrhoids by blocking the access of oxygen to the hemorrhoids. The essence of the procedure is the introduction of a special substance - sclerosant - into the space of the node, which subsequently leads to the appearance of an inflammatory process in the vein. As a result, the shell of the vessel sticks together and becomes overgrown. After the blood supply stops, the node dies
Advantages of the procedure:
- Ease of manipulation. Painless.
- During sclerosis, the patient can only feel a slight burning sensation and tingling. efficiency of the manipulation.
- Ambulatory treatment.
- It is possible to treat hemorrhoids even in older people if other methods are contraindicated for them.
- Quick results.
Infrared coagulation
An infrared coagulator acts on the pedicle of the hemorrhoid with an infrared heat wave, “sealing” the vessels. As a rule, it is prescribed for stages 1-2 of the disease, and also gives excellent results with complex treatment in combination with other methods.
Latex ligation
Latex ligation is the most common method of treating hemorrhoids without surgery. Latex ligation is one of the most popular methods of treating hemorrhoids and has a number of advantages over surgical treatment methods:
- does not require a long recovery period
- carried out quickly and painlessly
- in most cases avoids surgery
How is the latex ligation procedure performed?
The essence of the procedure is quite simple. Special latex rings are placed at the base of the internal hemorrhoids. No anesthesia is required. The procedure is quick and painless.
As a result, blood circulation in the tissues of the node is disrupted, and therefore the tissues begin to die. As a rule, the process begins 2-3 days after the procedure. As a result, after a few days the hemorrhoid dies and is rejected. In its place, a kind of stump is formed, covered with connective tissue. Ligation with latex rings is effective for stages 1-2 of the disease.
HAL-RAR technology
HAL execution principle
- The doctor ties each artery, reducing the flow of arterial blood to the enlarged hemorrhoid. Sutures are placed in the intestinal lumen, where there are no pain receptors. The procedure is performed painlessly.
- Next, the tissue of the internal hemorrhoid is compressed using a running stitch. Continuous lifting suture - RAR which returns to the normal position as before the disease. In this way we restore the normal functioning of the rectum.
Advantages of HAL-RAR
- No wounds or severe pain in the postoperative period.
- Only 1 day of hospital stay.
- Return to work in 1-2 days
- Very high efficiency of the method all over the world.
Traditional surgical treatment
The Milligan-Morgan operation, proposed back in 1937, still remains popular among coloproctologists in our country.
Although in most countries of America and Europe a typical hemorrhoidectomy is performed in only 17-21% of patients, the rest use minimally invasive treatment methods. Currently it is divided into two types.
Closed hemorrhoidectomy – with restoration of the mucous membrane of the anal canal. It is indicated for stage 3-4 hemorrhoids in the absence of clear boundaries between the external and internal hemorrhoids.
Open hemorrhoidectomy – involves removing the external and internal nodes en bloc, leaving an open wound of the anal canal. This operation is indicated for stage 3-4 hemorrhoids with a combination of anal fissure or paraproctitis.
A list of physical therapy exercises that are indicated for patients with sphincter insufficiency.
The starting position of the patient is on his back.
Select 4-5 exercises from the list, repeat each 7-10 times 2-3 times a day.
- Hands on the lower back: contracting the gluteal muscles, forcefully pull in the anus and hold for 15-20 seconds.
- The legs are bent at the knee joints and the feet are connected. Spread and bring your knees together.
- Legs are bent, feet near the buttocks. Raise your pelvis up, leaning on your feet and shoulder girdle. At the same time, strongly strain the gluteal muscles, pulling the anus into yourself.
- Legs bent, feet near buttocks. Raise your pelvis up, leaning on your feet and shoulder girdle. At the same time, lift the straightened leg up and move it to the side.
- Extend your arms along your body, legs straight. Raise your pelvis, resting on your heels, elbows, shoulder girdle and head, retracting your anus. Returning to the starting position, relax the gluteal muscles.
- Hands under your head. Raise both straight legs up, spread to the sides, bend at the knee joints, straighten, bring together and return to the starting position.
Diet No. 3 according to M. I. Pevzner
Cooking technology: food is prepared mainly unchopped, boiled in water or steamed, baked. Vegetables and fruits are consumed both raw and boiled. Food should mainly consist of vegetables, fresh and dried fruits, baked goods, cereals, and fermented milk drinks.
Allowed:
- Bread – wheat bread made from wholemeal flour: “Doctorsky”, “Zdorovye”, crispbread (soaked), rye. The cookies are dry, unpalatable pastries.
- Soups - mainly from vegetables in meat broth, cold fruit and vegetable soups, borscht, beetroot soup, cabbage soup made from fresh cabbage.
- Meat and poultry – lean varieties of various types of meat, chicken, turkey, boiled or baked, in pieces or chopped. Milk sausages.
- Fish – low-fat types, boiled or baked; seafood dishes.
- Vegetable dishes and side dishes - various types of vegetables and herbs, non-acidic sauerkraut, beets are especially recommended. Dishes and side dishes made from flour, cereals, legumes, crumbly and semi-viscous porridges, puddings, casseroles. Pasta, boiled and in the form of casseroles, dishes made with buckwheat are especially recommended. Legumes: green peas, bean curd.
- Eggs – no more than one egg per day, it is better to add them to dishes.
- Fruits, berries, sweet dishes and sugary products - melons, plums, figs, apricots, prunes, sugar, jam, especially rowan, honey, compotes (especially rhubarb), mousses, fruit candies are especially recommended.
- Milk, dairy products and dishes made from them - milk (if tolerated - sweet), sour cream, cottage cheese, yogurt, one- and two-day kefir, acidophilus milk, cheeses.
- Sauces and spices - milk, sour cream with vegetable broth, fruit and berry sauces.
- Fats – butter, vegetable oils from dishes.
- Appetizers - raw vegetable salads, vinaigrettes with vegetable oil, vegetable caviar, fruit salads, mild cheese, low-fat ham, soaked herring, jellied meat and fish.
- Drinks - tea, coffee substitutes, rosehip and wheat bran decoction, fruit and vegetable juices (plums, apricots, carrots, tomatoes).
Prohibited:
Bread made from premium flour, puff pastry and pastry, fatty meats and fish, duck, goose, smoked meat and fish, canned fish and meat, (limit rice and semolina), radish, radish, garlic, onion, turnip, mushrooms, jelly, blueberries, quince, dogwood, chocolate products with cream, hot and fatty sauces, horseradish, mustard, pepper, cocoa, black coffee, strong tea, animal and cooking fats, alcoholic beverages.
The clinic's coloproctology service has the most modern equipment and technologies for diagnosing and treating a wide range of diseases of the colon and rectum.
Make an appointment with a proctologist by phone or leave a request on the website.
Our advantages:
- Experienced doctors - proctologists who are proficient in laser treatment techniques - will work with you
- have modern equipment for minimally invasive treatment of rectal diseases at their disposal.
- Adequate pain relief will be provided by our highly qualified anesthesiologists.
- Short preparation time for surgery and rehabilitation
- Sick leave for the entire period of incapacity.
In our clinic you will receive qualified assistance: accurate diagnosis and effective treatment in complete confidentiality. We work every day, without days off. Make an appointment!
Benefits of laser hemorrhoid removal
- reduced operation time;
- the operation can be performed both under general or regional anesthesia and under local perianal anesthesia;
- there is no danger of bleeding, because the laser beam coagulates all vessels;
- during the intervention process, a coagulation film is formed in the surgical area, which prevents the penetration of infection;
- laser treatment of hemorrhoids can be performed on an outpatient basis - without prolonged hospitalization;
- healing in the postoperative area occurs without the formation of rough scars;
- Relapses after laser treatment of hemorrhoids are uncommon.
Laser coagulation of hemorrhoids in Voronezh: postoperative period
To avoid relapses and complications, several clear rules should be followed:
- Personal hygiene. After each bowel movement, you should wash the surface of the anus with cold water.
- For unpleasant sensations and to speed up healing, the use of suppositories with sea buckthorn oil or dressings with a special ointment is recommended. If pain occurs, you must take painkillers.
- Dieting. The diet must contain fermented milk products and a sufficient amount of plant fiber. You should avoid eating spicy and spicy foods and refrain from drinking alcohol.
- If constipation occurs, you can take medications that facilitate bowel movements (Mucofalk, Lactulose, etc.).
- You should not lift weights - laser coagulation of hemorrhoids in Voronezh is still a serious treatment method.
To receive qualified assistance, we invite you to. Here you can visit not only a proctologist, but also a gynecologist, urologist, otolaryngologist and other specialists. Within the walls of our clinic you can undergo body diagnostics using high-precision devices. And for women, our cosmetologist with many years of experience will conduct a unique lymphatic drainage facial massage, diagnose the condition of your skin and give truly effective care recommendations!
RESULTS OF TREATMENT OF HEMORRHOIDS BY SUBMUCOSAL W-LASER DESTRUCTION OF HEMORRHOIDAL PILES
Cherepenin M.Yu., Gorskiy VA, Armashov VP
Pirogov Russian National Research Medical University, Moscow, Russia
AIM: to evaluate the results of submucosal laser destruction of hemorrhoids using a W-laser.
PATIENTS AND METHODS: one-hundred twenty-four patients with chronic hemorrhoids underwent submucosal W-laser destruction of hemorrhoidal piles in September 2021 – January 2021.
RESULTS: the time of the procedure was 18-22 minutes. The hospital stay was 7-10 hours. The maximal edema of the pararectal area appeared by the 3rd days and was resolved on 13-14 days. The size of the edema depends on the volume of anesthetic. Maximum pain was observed on days 1 and 3 after surgery. The period for taking analgesics was not more than 7 days. No prolapse of hemorrhoidal piles was detected in all patients after 4 weeks postoperatively. No rectal bleeding was detected in 97.3%. The excellent result of treatment was found in 70.2%, good – in 22.6%, bad – in 7.2%.
CONCLUSION: submucosal W-laser destruction of hemorrhoidal piles showed a less pain intensity after surgery and a decrease in the complication rate, fast recovery and better quality of life.
[Key words: hemorrhoids, laser hemorrhoidectomy, submucosal laser hemorrhoidectomy, endovenous laser ablation, minimally invasive hemorrhoidectomy, minimally invasive surgical procedures
For citation: Cherepenin M.Yu., Gorskiy VA, Armashov VP Results of treatment of hemorrhoids by submucosal w-laser destruction of hemorrhoidal piles. Koloproktologia. 2020; v. 19, no. 2(72), pp. 104-111
Address for correspondence: Gorsky Viktor Aleksandrovich, Federal State Budgetary Educational Institution of Higher Education “Russian National Research Medical University named after. N.I. Pirogov" Ministry of Health of Russia, st. Ostrovityanova, 1, Moscow, 117997; tel.; e-mail: [email protected]
Recovery
Most people who undergo laser treatment for hemorrhoids typically report minimal pain or discomfort after treatment. The procedure time is also minimal, given that there is no need to cut or remove tissue. After surgery, the patient can leave the clinic approximately two hours after the intervention is completed. In the first days he may feel slight pain and discomfort.
The recovery period after laser hemorrhoid surgery is short as the patient can return to normal work after a maximum of two days of rest and then adopt a new lifestyle that includes improving the quality of food and incorporating exercise into their daily life to avoid recurrence of hemorrhoids .
Advice to patients after laser hemorrhoid surgery includes eating a fiber-rich diet as well as staying hydrated. They are very important for preventing constipation and, as a result, hemorrhoids. Sitz baths after laser hemorrhoid surgery can also relieve pain.
LITERATURE
1. De Nardi P, Tamburini AM, Gazzetta PG. et al. Hemorrhoid laser procedure for second- and third-degree hemorrhoids: results from a multicenter prospective study. Tech. Coloproctol. 2016; 20 (7): 455-459. DOI: 10.1007/s10151-016-1479-6.
2. Plapler H, Hage R, Duarte J. et al. A new method for hemorrhoid surgery: intrahemorrhoidal diode laser, does it work? Photomed Laser Surg. 2009; 27 (5): 819-823. DOI: 10.1089/pho.2008.2368.
3. Hodgson WJ, Morgan J. Ambulatory hemorrhoidectomy with CO2 laser. Dis Colon Rectum. 1995; 38 (12): 1265-1269. DOI: 10.1007/bf02049150.
4. Maloku H, Gashi Z, Lazovic R. et al. Laser hemorrhoidoplasty procedure vs open surgical hemorrhoidectomy: a trial comparing 2 treatments for hemorrhoids of third and fourth degree. Acta Inform Med. 2014; 22 (6): 365-367. DOI: 10.5455/aim.2014.22.365-367.
5. Pletnev S.D. Lasers in clinical practice. Guide for doctors. M.: Medicine, 1996. 432 p.
6. Skobelkin O.K. Lasers in surgery. M.: Medicine, 1989. 256 p.
7. Gain M.Yu., Shakhrai S.V. Minimally invasive technologies in the complex treatment of hemorrhoids. Surgery news. 2011; vol. 19, no. 4, p. 113-122.
8. Rodoman G.V., Kornev L.V., Shalaeva T.I. et al. The effectiveness of a combined method of treating hemorrhoids using HAL-RAR and laser destruction of nodes. Surgery. 2017; No. 5, p. 47-51. DOI: 10.17116/hirurgia2017547-51.
9. Goldman MP, Detwiler SP. Endovenous 1064-nm and 1320-nm Nd:YAG laser treatment of the porcine greater saphenous vein. Cosmetic Dermatology. 2003; 16 (2): 25-28.
10. Naderan M, Shoar S, Nazari M. et al. A randomized controlled trial comparing laser intra-hemorrhoidal coagulation and Milligan Morgan hemorrhoidectomy. J Invest Surg. 2017; 30 (5): 325-331. DOI: 10.1080/08941939.2016.1248304.
11. Proebstle TM, Moehler T, Gül D. et al. Endovenous treatment of the great saphenous vein using a 1,320 nm Nd: YAG laser causes fewer side effects than using a 940 nm diode laser. Dermatol Surg. 2005; 31 (12): 1678-1683.
12. Weyand G, Theis CS, Fofana AN, Rüdiger F, et al. Laserhämorrhoidoplastie mit dem 1470-nm-diodenlaser in der behandlung des zweit-bis viertgradigen hämorrhoidalleidens – eine kohortenstudie mit 497 fällen. Zentralbl Chir. 2017; 144 (4): 355-363. DOI: 10.1055/s-0043-120449.
Restrictions on the procedure
The restrictions are general in nature and do not differ from contraindications for surgical treatment with other techniques. In any case, the proctologist surgeon decides on the procedure individually, if necessary, involving doctors of other specializations for consultation.
- Individual intolerance to anesthesia drugs;
- Severe forms of chronic concomitant diseases;
- Exacerbations, decompensation of chronic diseases;
- Acute infectious diseases.
After the procedure, you need to be under the supervision of a doctor for about an hour, at rest. In the next few days after surgery, you should not exercise, lift weights, or overheat. Hospitalization is not necessary in most cases.
Do hemorrhoids lead to cancer?
No. There is no connection between the development of this disease and malignant tumors. However, some symptoms, especially bleeding, are also characteristic of colorectal cancer and other diseases of the digestive system. Therefore, it is very important to consult a coloproctologist if any symptoms of hemorrhoids appear. Today, there are a wide range of medications available in pharmacies that can reduce the symptoms of hemorrhoids, but you should not treat them yourself.
At an appointment with a coloproctologist surgeon, after a qualified examination and assessment of symptoms, you will be prescribed adequate treatment.
Indications for surgical treatment
Hemorrhoids in the early and middle stages of the disease are treated with traditional methods. Surgical intervention is used only in the presence of complications:
- Prolapse of hemorrhoids
- Diffuse bleeding from the veins of the rectum
- Thrombosis of nodes
- Heavy infrequent bleeding from the anus
If blood is constantly released in small doses, this can lead to anemia. Prolapse of hemorrhoids puts additional stress on the skin, which leads to inflammation in the anal area. Mucus released from the surface of the nodes irritates the skin and reduces its protective properties. The risk of microbial or viral infection increases.
In some cases, patients themselves ask doctors for surgery. Their hemorrhoids reach such a stage that people can no longer tolerate itching and severe pain in the rectum.