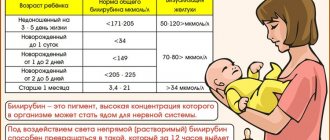
How is bilirubin formed?
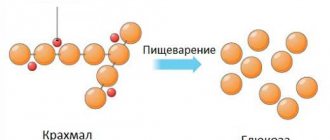
Erythrocytes - red blood cells - contain hemoglobin. It carries oxygen to the body tissues from the lungs. When old and damaged red blood cells die, hemoglobin is released and converted into bilirubin.
Bilirubin is converted hemoglobin
Newly formed bilirubin is called indirect: it is highly toxic and dangerous to humans, especially to the central nervous system (CNS). Therefore, the body then starts the process of neutralizing bilirubin - this happens in the liver. When bilirubin becomes safe - straight - the liver secretes it along with bile, and it leaves the body through the intestines.
When an analysis is made for bilirubin levels, there are three types: indirect, direct and total. For an adult under 60 years of age, the following indicators are considered normal:
- Indirect bilirubin – within 3.4-12 mmol/l;
- Direct bilirubin – within 1.7-5.1 mmol/l;
- Total bilirubin is in the range of 5.1-17 mmol/l.
If the bilirubin level is higher than normal, you need to find out the reason for the jump, because it may indicate the development of a serious illness.
Where do diffuse liver changes come from? Diffuse changes affect the structure of the liver, its main functional tissue – the parenchyma.
Complications
The most common and dangerous complications are associated not with hyperbilirubinemia itself, but with the cause that caused it. Severe adverse consequences of hyperbilirubinemia occur in newborns with kernicterus. Deep damage to the subcortical nuclei and cerebral cortex without timely treatment can lead to sensorineural hearing loss, seizures, and in some cases, death. Due to the deterioration of cholesterol excretion into bile, its plasma concentration increases, as a result of which the process of formation of atherosclerotic plaque is accelerated. This increases the risk of myocardial infarction and ischemic stroke.
Increased total bilirubin - reasons
An increase in total bilirubin in adults leads to:
- Primary biliary cirrhosis;
- Gallstone disease and other conditions with impaired bile flow;
- Parasitic diseases;
- Liver tumors;
- Any type of hepatitis (viral, drug-induced, autoimmune, etc.);
- Intrahepatic cholestasis;
- Jaundice of pregnancy;
- Accelerated breakdown of red blood cells;
- Impaired production of enzymes in the liver that convert indirect bilirubin into direct bilirubin.
What the doctor sees on an ultrasound of the liver Ultrasound is the most popular diagnostic method when the patient complains of discomfort in the right side, nausea, weakness and general loss of strength.
Treatment of Gilbert's syndrome
The mere presence of Gilbert's syndrome in children and adults is not an indication for drug treatment.
To prevent exacerbation of the disease and the development of complications, general measures are important: limiting participation in strenuous sports, prolonged exposure to the sun, consumption of alcoholic beverages and hepatotoxic drugs. Such patients need to eat right, avoid prolonged fasting, as well as foods containing indigestible fats - fatty meats, fried and spicy foods, canned foods. During an exacerbation of the clinical manifestations of the disease, plenty of fluids and a gentle diet corresponding to table No. 5 are prescribed. Conservative therapy during this period is aimed at reducing the formation and accelerating the removal from the body of excess amounts of unconjugated hemoglobin and includes:
- taking microsomal enzyme inducers (phenobarbital, zixorine);
- taking activated carbon;
- phototherapy.
For the prevention of cholecystitis and cholelithiasis in Gilbert's syndrome, the use of choleretic herbs, hepatoprotectors (ursosan, ursofalk), essential phospholipids, choleretics (cholagol, allochol, holosas) and B vitamins is recommended.
Increased direct bilirubin - reasons
The increase in the level of direct bilirubin is based on a violation of the outflow of bile. As a rule, this occurs due to the development of the following pathologies:
- Gallstone disease (GSD);
- Hepatitis: viral, bacterial, drug-induced, autoimmune, toxic, medicinal;
- Cancer of the liver, pancreas or gallbladder;
- Biliary cirrhosis;
- Rotor and Dubin-Johnson syndromes.
Why is my liver enlarged? An enlarged liver may be associated with diseases of other organs. We tell you what pathologies cause changes in the size of the body's main detoxifier.
Classification
Depending on which fraction of bile pigment is increased, there are:
- Indirect hyperbilirubinemia
. Unconjugated (unbound) bilirubin is increased. The cause is pathologies that cause suprahepatic jaundice - hemolytic anemia, benign hyperbilirubinemia. - Direct hyperbilirubinemia
. Accompanied by an increase in the level of conjugated (bound) bilirubin. The cause is diseases leading to hepatocellular and subhepatic jaundice. The most common of them are viral, alcoholic hepatitis, cholecystitis.
Bilirubin encephalopathy (kernicterus) is distinguished separately. It occurs in hemolytic disease of newborns, the cause of which is the incompatibility of erythrocyte antigens (Rh conflict) of the mother and fetus. This disease is very serious, it is characterized by damage to the subcortical nuclei and cerebral cortex and requires immediate treatment.
Increased indirect bilirubin - reasons
The amount of indirect bilirubin in the blood increases when too many red blood cells are destroyed. This occurs in the following pathologies:
- Hemolytic anemia: congenital, acquired autoimmune (against the background of systemic lupus erythematosus, rheumatoid arthritis, lymphocytic leukemia, etc.), toxic (poisoning with drugs, poisons, mushrooms, insect bites, etc.);
- Infectious diseases: sepsis, typhoid fever, malaria;
- Gilbert, Crigler-Najjar, Lucy-Driscoll syndromes.
Pain in the right side: what could it be? How to recognize the disease by one symptom? We are studying which organs can cause pain in the right hypochondrium.
Prognosis and prevention
The prognosis and life expectancy for hyperbilirubinemia is determined by the cause, i.e. main disease. For example, hemolytic disease of newborns, viral hepatitis B, C, and some forms of hemolytic anemia (hemoglobinopathies) are characterized by a high incidence of death. Benign hyperbilirubinemia and chronic cholecystitis, on the contrary, have a favorable prognosis and do not affect life expectancy in any way.
To prevent hyperbilirubinemia, you should limit the consumption of alcohol and fatty foods. For Rh-negative pregnant women, anti-Rhesus immunoglobulin (anti-D immunoglobulin) is administered to prevent the development of HDN.
Signs of increased bilirubin
The liver is the main link in the production and removal of bilirubin from the body. Therefore, most diseases that provoke an increase in the amount of pigment in the blood are associated with the liver. In liver pathologies, increased bilirubin manifests itself as follows:
- Discomfort in the right side;
- Nausea, belching after eating (especially after fatty foods);
- Dizziness, loss of strength, bad mood;
- Light stool and dark urine;
- With viral hepatitis, increased body temperature.
The following symptoms are observed in gallstone disease:
- yellowness of the skin and mucous membranes;
- pain in the right side;
- bloating, abnormal stool;
- skin itching.
To failure: how liver diseases progress In the initial stages, liver diseases are completely reversible, but there are conditions when medications are powerless and only a transplant can save the patient’s life.
Pathogenesis
Features of the pathogenesis (mechanisms of occurrence) of hyperbilirubinemia are determined by the cause. Free (indirect, unconjugated) bilirubin is poorly soluble in water, but has high lipophilicity, i.e. soluble in fats. Therefore, it can interact with phospholipids of cell membranes, especially brain cells, due to which it penetrates the blood-brain barrier, where it uncouples the processes of oxidative phosphorylation and reduces ATP synthesis.
This explains the toxicity of free bilirubin to cells of the nervous system. This is most pronounced in newborns. Bilirubin can color the skin, visible mucous membranes, urine, and feces a characteristic yellow or dark brown color. With prolonged cholestasis, which causes an increase in the concentration of conjugated bilirubin, catabolism and cholesterol excretion may be impaired, which leads to its accumulation in the blood and the progression of atherosclerosis.
What to do if there are signs of increased bilirubin
It will not be possible to normalize bilirubin levels without laboratory tests, because first of all you need to find out the reason for the change in the amount of pigment in the blood. This means that you need to check the level of ALT and AST enzymes, do an analysis for viral hepatitis and an ultrasound of the liver.
If the increase in bilirubin is caused, for example, by cholelithiasis, then cholecystectomy (removal of the gallbladder) or drug therapy with ursodeoxycholic acid is indicated. If viral hepatitis occurs, antiviral therapy is necessary. If a person has a parasitic disease, the helminths must be destroyed. Those. the scheme of action depends entirely on the condition that led to the increase in bilirubin.
Main indicators of liver tests
Let's consider the main indicators of liver tests, as well as their norms and reasons for deviations from reference values.
Alanine aminotransferase (ALT) and aspartate aminotransferase (AST)
ALT and AST are enzymes that are synthesized intracellularly, take part in carbohydrate and protein metabolism, support the functioning of many organs, and play a key role in the metabolism of one of the most important amino acids - alanine and aspartic acid. In the absence of pathologies, enzymes are present in the blood only in small quantities ⇓⇓⇓
| Age | ALT norms, units/l | AST standards, units/l |
| < 5 days | < 49 | < 97 |
| 5 days-6 months | < 56 | < 77 |
| 6-12 months | < 54 | < 82 |
| 1-3 years | < 33 | < 48 |
| 3-6 years | < 29 | < 36 |
| 6-12 years | < 39 | < 47 |
| 12-17 years old (girls) | < 34 | < 25 |
| 12-17 years old (boys) | < 27 | < 29 |
| over 17 years old (women) | < 31 | < 31 |
| over 17 years old (men) | < 41 | < 37 |
Despite some similarities, ALT and AST also have differences:
- ALT is produced to a greater extent in the liver, and to a lesser extent in the muscles, heart, pancreas, kidneys and other organs. In this regard, high levels of the enzyme primarily indicate liver disease.
- AST is found in the same cells as ALT, but in the myocardium its concentration is much higher. That is why the main reasons for increased AST are not only liver pathologies, but also heart diseases.
In what cases does ALT increase?
The main reasons for increased ALT include:
- death of hepatocytes (liver parenchyma cells) caused by viral hepatitis and exposure to toxic substances;
- Liver cirrhosis is a chronic pathology in which healthy organ tissue is replaced by connective tissue or stroma;
- intrahepatic cholestasis - insufficient secretion of bile due to a violation of its production by liver cells;
- fatty hepatosis is a syndrome accompanied by the accumulation of fat in the liver tissue;
- liver oncology.
Less common causes of high ALT values:
- heart failure;
- myocardial infarction;
- inflammation of the heart muscle;
- inflammation of skeletal muscles;
- severe burns;
- shock;
- alcoholism.
Also, the ALT value may be increased when taking hepatotoxic drugs, which include some antibacterial, anabolic, contraceptives, and drugs containing salicylic acid. As a rule, the increase in ALT in this case is temporary.