Intrauterine development of the atria
ASD refers to embryological pathologies, since it is in the intrauterine period that changes occur that lead to the disease. The development of the functional elements of the fetal heart occurs at 1-2 months of pregnancy.
Initially, the organ looks like a solid cavity with communicating vessels. At the end of the first month of embryogenesis, the heart completes its division into two parts. In this case, the primary atrium is protected by the interatrial septum of the same name. Only a small hole remains uncovered. Subsequent development of the septum primum leads to complete elimination of the heart defect.
But complete separation of the atria does not occur due to the appearance of a new opening - the secondary interatrial. Blood flow from one cavity to another is a vital condition for the normal functioning of the fetus. To eliminate the hole, a secondary septum grows, which has the shape of a crescent. Due to this anatomy, a so-called oval window occurs.
Classification
All ASD classifications are based on embryological aspects. In this regard, the following types of defect are distinguished:
- Ostium primum type defect (primary) - located at the very bottom of the atrial septum. Arises due to its incomplete development.
- A defect such as ostium seduncum (secondary) appears when the growth of the primary septum has completed normally, but the secondary overgrowth is not complete. It is located closer to the center, close to the oval fossa.
- Sinus venosus (Venous sinus defect - occurs near the sinus node and the entrance to the superior vena cava.
- Coronary sinus defect.
- Open oval window.
Aplasia of the septum is rarely observed. It is necessary to distinguish between developmental defects and some cardiac abnormalities that correspond to normal variants. Thus, an open oval window differs from a secondary type defect in that in the first days of a child’s life this structure is overgrown.
Signs and symptoms
Secondary ASD is the most common form of this group of heart defects. The middle part of the interatrial septum in the area of the foramen ovale does not close during fetal development. The size of the hole may vary, along with the severity of symptoms.
The primary form of ASD is less common. The lower part of the interatrial septum fails to develop normally, leaving a hole between the atria. Often the valves that separate the atria from their respective ventricles (tricuspid and mitral) are also misshapen, and the septum that separates the ventricles may also be defective or misshapen (atrioventricular septal defect). Another defect (endocardial cushion defect) possibly occurs during embryonic development in the tissue that forms the septum, dividing the heart into atria and ventricles.
A venous sinus defect , the least common form of ASD, occurs when there is a hole in the upper part of the interatrial septum. This defect is often associated with a malformation of the vein that leads from the lungs to the heart (right pulmonary vein). One of the body's main veins that returns blood to the heart (the superior vena cava) may also be damaged.
Most children with atrial septal defects have no symptoms. A few affected children may be abnormally thin and experience mild growth retardation, as well as increased susceptibility to respiratory infections. Other very severely affected children, especially those with the primary form of the defect, may experience shortness of breath, easy fatigue on exertion, and/or an irregular heartbeat (arrhythmias).
A heart murmur is the most common sign and usually the only sign of ASD in children. There may also be changes in heart sound, which represent closing of the heart valves.
Around age 40, people with an ASD may experience symptoms related to increased pressure in the blood vessels of the lungs (pulmonary hypertension). Increased pressure in these vessels causes blood to move or "shunt" through an abnormal opening in the heart. Symptoms may include a bluish discoloration of the skin (cyanosis), cracked fingertips, exercise intolerance, and/or an abnormal increase in the number of circulating red blood cells (polycythemia). Abscesses in the brain may also develop. Other symptoms may include swelling of the arms and legs and/or difficulty breathing.
Severe cases of ASD can lead to life-threatening complications such as chest pain, irregular heartbeat (arrhythmia), abnormal enlargement of the heart, fluttering of the heart (atrial fibrillation) and/or heart failure. Women with atrial septal defects who become pregnant may be at risk for blood clots. These clots (thrombi) can break away from the walls of blood vessels and travel through the systemic circulation, causing an embolism.
Clinical picture
The severity of symptoms is influenced by the following factors:
- tension in the atria;
- patient's age;
- stretchability of the atrial muscles on the right;
- area of the anomalous zone;
- number of unclosed holes, etc.
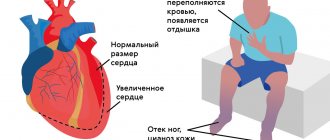
In the left parts of the heart, the pressure is 5-6 mmHg higher. Art. Atrial septal defect allows blood to flow into the right region of the heart, which overloads it. Compensatoryly, the heart is able to cope with excess blood for some time, which is not pushed into the vessels. But over time, reserves are depleted. Upon reaching 20-25 years of age, all protective mechanisms fail with the development of vivid clinical symptoms.
Atrial septal defect
Atrial septal defect (ASD) is the second most common congenital heart defect.
With this defect, there is a hole in the septum that separates the right and left atria into two separate chambers. The fetus, as we said above, not only has this hole (open oval window), but is also necessary for normal blood circulation. Immediately after birth it closes in the vast majority of people. In some cases, however, it remains open without people being aware of it. The discharge through it is so insignificant that a person not only does not feel that “there is something wrong with the heart,” but he can calmly live to a ripe old age. (It is interesting that, thanks to the capabilities of ultrasound, this defect in the interatrial septum is clearly visible, and in recent years, articles have appeared that show that among such adults and healthy people who cannot be classified as patients with congenital heart disease, there is a significantly higher number of people suffering from migraines - severe headaches. These data, however, have yet to be proven).
Unlike patent foramen ovale, true atrial septal defects can be very large. They are located in different parts of the septum itself, and then they speak of a “central defect” or “a defect without an upper or lower edge,” “primary” or “secondary.” (We mention this because the type and location of the hole may depend on choice of treatment type).
If there is a hole in the septum, a shunt occurs with blood discharge from left to right. With an ASD, blood from the left atrium partially flows into the right atrium with each contraction. Accordingly, the right chambers of the heart and lungs become overfilled, because they have to pass through themselves a larger, extra volume of blood, and one more time that has already passed through the lungs. Therefore, the pulmonary vessels are filled with blood. Hence the tendency to pneumonia. The pressure in the atria, however, is low, and the right atrium is the most “distensible” chamber of the heart. Therefore, while increasing in size, it copes with the load for the time being (usually up to 12-15 years, and sometimes more) quite easily. High pulmonary hypertension, which causes irreversible changes in the pulmonary vessels, never occurs in patients with ASD.
The vast majority of newborns, infants, and young children grow and develop absolutely normally. Parents may notice their tendency to frequent colds, sometimes resulting in pneumonia, which should be alarming. Often these children, in 2/3 of cases girls, grow up pale, thin and somewhat different from their healthy peers. They try to avoid physical activity as much as possible, which in the family can be explained by their natural laziness and reluctance to tire themselves out.
Heart complaints can and, as a rule, appear in adolescence, and often after 20 years. Usually these are complaints about “interruptions” in the heart rhythm that a person feels. Over time, they become more frequent, and sometimes lead to the patient becoming incapable of normal, ordinary physical activity. This does not always happen: G.E. Falkowski once had to operate on a patient aged 60, a professional driver, with a huge atrial septal defect, but this is an exception to the rule.
To avoid such a “natural” course of the defect, it is recommended to close the hole surgically. Unlike a VSD, an interatrial defect will never heal on its own.
Surgery for ASD is performed under artificial circulation, on an open heart, and consists of suturing the hole or closing it with a patch. This patch is cut out from the heart sac - the pericardium - the sac surrounding the heart. The size of the patch depends on the size of the hole. It must be said that the closure of an ASD was the first open-heart surgery, and it was performed more than half a century ago.
Sometimes an atrial septal defect can be combined with an irregular, anomalous entry of one or two pulmonary veins into the right atrium instead of the left. Clinically, this does not manifest itself in any way, and is a finding when examining a child with a large defect. This does not complicate the operation: the patch is simply larger and is made in the form of a tunnel in the cavity of the right atrium, directing blood oxidized in the lungs to the left parts of the heart.
Today, in addition to surgery, in some cases it is possible to safely close the defect using X-ray surgery
technology. Instead of suturing the defect or sewing in a patch, it is closed with a special umbrella-shaped device - an occluder, which is passed along the catheter in a folded form and opened, passing through the defect.
This is done in the X-ray surgery room, and we described everything related to such a procedure above when we touched on probing and angiography. Closing a defect with such a “non-surgical” method is not always possible and requires certain conditions: anatomical location of the hole, sufficient age of the child, etc. Of course, if they are present, this method is less traumatic than open-heart surgery. The patient is discharged after 2-3 days. However, it is not always feasible: for example, in the presence of abnormal vein drainage.
Today, both methods are widely used, and the results are excellent. In any case, the intervention is elective and not urgent. But it needs to be done in early childhood, although it can be done earlier if the frequency of colds and, especially, pneumonia becomes frightening and threatens bronchial asthma, and the size of the heart increases. In general, the sooner the operation is performed, the sooner the child and you will forget about it, but this does not mean that you should be in a particular hurry with this defect.
How to get treatment at the Scientific Center named after. A.N. Bakuleva?
Online consultations
Symptoms of ostium primum
Most often appear in childhood. The pathology accounts for about 15% of all ASDs and is characterized by a fairly large defect in the septum. A distinctive feature is the combination of the defect with other anomalies:
- mitral valve insufficiency;
- Down syndrome;
- splitting of the anterior part of the mitral valve.
Children with this disease complain of difficulty breathing, shortness of breath, which worsens during physical activity, and attacks of palpitations.
Significant defects lead to the development of early heart failure, which is characterized by the following symptoms:
- swelling of the arms, legs, anterior abdominal wall;
- cough with phlegm;
- chest pain;
- cyanosis of the limbs, nasolabial triangle, etc.
Patients with a minor degree of pathology live up to 45-50 years. In this case, all have a pronounced clinical picture.
Disorders with similar symptoms
Symptoms of the following disorders may be similar to those of atrial septal defects. Comparisons can be useful for differential diagnosis:
- Atrioventricular (AV) septal defect is a rare heart defect that is present at birth (congenital) and is characterized by abnormal development of the septa and valves of the heart. Children with a complete form of the defect usually develop congestive heart failure. Often, excess fluid accumulates in certain areas of the body, especially the lungs. This pulmonary congestion can lead to difficulty breathing (dyspnea). Other symptoms may include bluish discoloration of the skin (cyanosis), poor nutrition, abnormally fast breathing (tachypnea) and heart rate (tachycardia) and/or excessive sweating (hyperhidrosis). Adults with an AV septal defect may experience abnormally low blood pressure, irregular heartbeat, and/or rapid heartbeat.
- Ventricular septal defects (VSDs) are a group of common congenital heart defects characterized by the absence of one ventricle. Children with these defects may have 2 atria and 1 large ventricle. Symptoms of these conditions are similar to an atrioventricular septal defect and may include an abnormally fast breathing rate (tachypnea), wheezing, a fast heartbeat (tachycardia), and/or an abnormally enlarged liver (hepatomegaly). A ventricular septal defect can also cause excessive fluid to accumulate around the heart, leading to congestive heart failure.
- Triatrial heart is an extremely rare congenital heart defect characterized by the presence of an additional chamber above the left atrium of the heart. The pulmonary veins, which return blood from the lungs, drain into this additional “third chamber.” Symptoms of triatrial heart disease vary greatly and depend on the size of the opening between the chambers. Symptoms may include abnormally rapid breathing (tachypnea), wheezing, coughing, and/or abnormal accumulation of fluid in the lungs (pulmonary congestion).
- A single ventricle heart is an extremely rare congenital heart defect characterized by the absence of one ventricle. Children with this defect have two atria and one large ventricle. Symptoms are similar to those of an atrial septal defect and include difficulty breathing (shortness of breath), excessive fluid accumulation in the lungs and around the heart (pulmonary edema), and/or a bluish discoloration of the skin and mucous membranes (cyanosis). Other symptoms may include poor eating habits, abnormally fast breathing (tachypnea), and/or abnormally fast heartbeat (tachycardia).
- Mitral valve stenosis is a rare heart defect that can be present at birth or acquired. It is characterized by an abnormal narrowing of the opening of the mitral valve. In the congenital form, symptoms vary greatly and may include cough, difficulty breathing, rapid heartbeat and/or frequent respiratory infections. With acquired mitral valve stenosis, symptoms may also include weakness, abdominal discomfort, chest pain (angina) and/or intermittent loss of consciousness.
Atrial septal defect can occur in association with a variety of other disorders, including:
- Down syndrome;
- Ellis van Creveld syndrome;
- Smith-Lemli-Opitz syndrome;
- Costello syndrome;
- chondroectodermal dysplasia;
- fetal rubella;
- Holt-Oram syndrome;
- Hurler syndrome and others.
Clinic of anomalies of the ostium secundum and sinus venosus type
The pathology can be combined with hypoplasia of the fingers, mitral stenosis, narrowing of the pulmonary valve, disruption of the sinus node, and abnormal location of the pulmonary veins on the right. In women, pathology is detected 2 times more often than in men. A minor degree of the disease may occur without clinical manifestations.
If there is a large defect, then patients complain of shortness of breath, weakness, a feeling of interruptions in the functioning of the heart, frequent episodes of bronchitis, and acute respiratory viral infections. It is extremely rare to experience bluishness of the face and changes in the shape of the fingers like “drumsticks” when the nail phalanges expand.
Forecast
Although life expectancy is not normal for patients with ASD, patients typically survive into adulthood without surgical or percutaneous intervention, and many patients live to an advanced age. However, natural survival after age 40–50 is less than 50%, and the rate of attrition after age 40 is about 6% per year. Long-term pulmonary hypertension rarely occurs before the third decade. Late complications include stroke and atrial fibrillation.
Course of the disease in the absence of treatment
Patients with an atrial septal defect of up to medium size live to the age of 35-55 years with satisfactory general health. The severity of the condition is determined by the development of complications in patients in the form of pulmonary hypertension. It is characterized by the following changes:
- high pressure in the pulmonary artery;
- increased load on the right ventricle;
- hypertrophy of the right heart;
- inability of blood circulation to cope with increasing loads.
Mature patients have a high risk of embolization of the pulmonary arteries and vessels of the systemic circulation. In the presence of a combination of ASD and pulmonary hypertension, Eisenmenger syndrome develops, significantly increasing the mortality rate.
Causes
Most cases of atrial septal defects occur on their own for no apparent reason (sporadic). The exact nature of the developmental defect or defects that may occur during embryonic development (embryogenesis) remains unclear.
Some cases of ASD run in families. In such rare cases, the two types, ostium primum and ostium secundum, appear to be inherited as autosomal dominant genetic traits. To further complicate matters, genetic analysis suggests that there are at least two different genetic disorders associated with ASD, which involve mutations in a gene called Nkx2-5.
Chromosomes, which are present in the nucleus of human cells, carry genetic information for each person. Cells in the human body usually have 46 chromosomes. The pairs of human chromosomes are numbered 1 to 22, and the sex chromosomes are designated X and Y. Men have one X and one Y chromosome, and women have two X chromosomes. Each chromosome has a short arm, designated "p", and a long arm, designated "q". Chromosomes are further divided into many numbered bands. For example, "chromosome 6p21.3" refers to band 21.3 on the short arm of chromosome 6. Likewise, "chromosome 8p23.1-p22" refers to the region between bands 22 and 23.1 on the short arm of chromosome 8. The numbered bands indicate the location of thousands of genes that present on every chromosome.
Genetic diseases are determined by the combination of genes for a particular trait that are found on chromosomes received from the father and mother.
Dominant genetic disorders occur when only one copy of the abnormal gene is needed to cause the disease. The abnormal gene may be inherited from either parent or may be the result of a new mutation (gene change) in the affected person. The risk of passing the abnormal gene from the affected parent to the offspring is 50% for each pregnancy, regardless of the sex of the child.
Recessive genetic disorders occur when a person inherits the same abnormal gene for one trait from each parent. If a person receives one normal gene and one disease gene, the person will be a carrier of the disease, but usually asymptomatic. The risk of two carrier parents both passing on the defective gene and therefore having an affected child is 25 percent in each pregnancy. The risk of having a child who is a carrier as the parents is 50 percent with each pregnancy. The chance for a child to receive normal genes from both parents and be genetically normal for that particular disease is 25 percent. The risk is the same for men and women.
All people carry 4-5 abnormal genes. Parents who are closely related (brother and sister) have a higher chance than unrelated parents of having the same abnormal gene, increasing the risk of having children with a recessive genetic disorder.
Atrial septal defect can also occur in association with a variety of other congenital heart defects, or in newborns that are relatively small or premature. The primary form of the disease often occurs in people with Down syndrome or Ellis van Creveld syndrome.
Physical examination
During examination of infants, underweight and lethargy may be noted. Sometimes hypoplasia (underdevelopment) of the fingers is detected. In this case, there is no bulging of the neck veins or their pulsation. The pulse on the wrists is normal, without any abnormalities.
Examination of the chest reveals a bulging right atrium. In some cases, increased pulsation of the wall of the pulmonary artery is noted in the 2nd intercostal space on the left.
Percussion (tapping) confirms the fact of expansion of the cardiac boundaries due to the right sections. In this case, the left part is enlarged due to the displacement of the neighboring one by the right ventricle.
Auscultation (when listening with a stethoscope) determines the following changes:
- strengthening of the first tone. The sounds produced by the tricuspid heart valve are heard;
- bifurcation of the second tone;
- in the second intercostal space to the left of the sternum there is an ejection click and a systolic murmur, which is often confused with normal;
- mesodiastolic murmur in the second and third intercostal spaces occurs with significant defects. The appearance of the auscultation pattern is associated with insufficiency of the pulmonary valve apparatus.
If an atrial septal defect is suspected, the doctor will refer the patient for further examination.
How does pathology manifest itself?
Health complaints are mainly due to decompensation of blood flow. The stronger the overload of certain parts of the system, the more pronounced the symptoms will be. Patients begin to worry about shortness of breath, fatigue, and frequent colds, especially in children.
When listening to the heart, a systolic murmur is heard with a source above the pulmonary artery. The sounds are caused by difficulty when too much blood flows through the lumen of the pulmonary trunk. The ECG shows signs of overload on the right side of the heart with hypertrophy in this area.
Prices for services
| Name | Time | Price | |
| Appointment with a cardiologist, treatment and diagnostic, primary, outpatient | 1500 | ||
| Treatment and diagnostic appointment with a cardiologist, repeated, outpatient | 1000 | ||
| Preventive, outpatient appointment with a cardiologist | 550 | ||
| Comprehensive consultation with a cardiologist ECG with interpretation + Echo-kg | 3650 | ||
| Call a doctor to your home (Khimki, Starbeevo, Ivakino, Naberezhnye) | 5350 | ||
| Calling a doctor to your home (Skhodnya, Podrezkovo, Novopodrezkovo, Planernaya station, Firsanovka) | 6450 | ||
| Call a doctor to your home (Kurkino, Novogorsk) | 5900 | ||
| Call a doctor to your home (Left Bank, Moscow, within the Moscow Ring Road) | 7500 | ||
| Medical consultation | 3300 | ||
| Extract from outpatient card | 660 | ||
| Consultation (interpretation) with analyzes from third parties | 1300 | ||
| Consultation on treatment adjustments | 550 | ||
| Repeated reception of CMN | 1600 | ||
| Initial reception of CMN | 2000 | ||
| Express test for determining the level of Troponin in the blood. | 1900 | ||
| Expand all prices | |||
ECG diagnostics, echocardiography and x-ray
An important component of any cardiac diagnosis is an ECG and echoCG. These simple and accessible methods allow us to determine the following changes in patients with congenital heart disease:
- deviation of the normal axis of the heart to the right and left;
- prolongation of the PQ interval;
- P wave in the third lead below the isoline;
- atrioventricular nodal and lower atrial pathological rhythms;
- incomplete blockade of the right branch of the His bundle.
These signs can be combined with each other or occur as single symptoms.
During an ultrasound, expanded contours of the heart and abnormal motor activity of the interventricular septum are detected. Ultrasound examination allows you to reliably assess the anatomical and functional abilities of the heart in real time.
Currently, the study is included in the gold standard for detecting congenital malformations. It can also be used to determine the status of a patent foramen ovale in newborns and the presence of an ASD.
A general X-ray of the chest also determines that the boundaries of the heart are expanded. If there is an anomalous confluence of the right pulmonary veins, the “Turkish saber” effect can be seen on the radiograph - a radiographic shadow at the edge of the right atrium. An intensification of the pulmonary pattern is often noted.
Diagnosis and treatment of AMPP
The main, effective method for detecting aneurysm of the interatrial septum in children is ultrasound examination of the heart, which is also called echocardiography. This procedure is characterized by absolute safety and the absence of any painful sensations for the child being examined. All clinics of the medical network in Makhachkala use the most modern ultrasound machines, which are staffed by highly qualified specialists, which makes it possible to reliably diagnose even the smallest patients with hidden, asymptomatic forms of pathologies.
If mild forms of aneurysm are detected in children, no special treatment is required. Such babies need to undergo a consultation with a cardiologist once a year after undergoing ultrasound diagnostics. Young patients are recommended to undergo gentle physical activity, avoid psycho-emotional stress, walks and games in the fresh air, good, long sleep and a balanced diet rich in vitamins, protein and microelements necessary for the child. Psychotherapy sessions and auto-training are very useful for children with AMPP. To improve cardiac activity, the attending physician usually also prescribes electrophoresis procedures with magnesium.
Invasive methods
Medical information about patients with concomitant pathologies such as pulmonary hypertension and coronary artery disease can be supplemented using cardiac catheterization and coronary angiography. The first procedure involves passing a catheter through an opening in the septum between the atrium cavities. If the tube passes, you can suspect the presence of pathology. But in the case of an open oval window, the situation will be identical.
To clarify the information, blood flow rates and the degree of oxygen saturation are determined. If the latter value in the right atrium is 10% greater than the superior vena cava, we can speak of an ASD.
Standard Treatments
Treatment is usually surgical with medications limited to the period during which the patient awaits surgery. In the case of very young patients, "watchful waiting" is often sufficient as the hole closes as the child grows.
- Surgical intervention.
Until recently, surgery to close the hole in the heart was the favored form of treatment. Open heart surgery was designed to stitch the edges of the hole and close it. In some cases, the hole can be patched and closed with a graft or prosthesis. The success rate is high for these surgical procedures. In the primary form of ASD, surgery can be performed to repair or replace the atrioventricular valves. The success rate for this complex procedure is significantly lower. The operation is optimally performed between the ages of 3 and 6 years.
In recent years, a less traumatic method of closing the septal opening has been developed using catheters to which is attached a special device designed to close the septal opening. During this procedure, a long, thin tube (catheter) is inserted into a large vein at the top of the child's leg and carefully advanced through the blood vessel until it reaches the heart. When the catheter reaches the desired point, a defect closure device is fed through its tip, which opens and seals the hole.
Treatment of patients with medications
Treatment of pathology with drugs is aimed at relieving symptoms and complications. However, it cannot be called pathogenetic, i.e. eliminating the cause of all changes in health status. To treat right ventricular failure, diuretics may be prescribed. Beta blockers are used to relieve arrhythmias.
Antibiotic therapy is used to prevent infection and the development of endocarditis before and after surgery.