Accelerated metabolism and increased oxygen demands cause children's hearts to beat faster. Heart rate norms are individual for each age. If for some reason this indicator exceeds the norm for no apparent reason (emotional experiences or physical exertion, overheating), tachycardia is diagnosed. At the medical center (Moscow, Otradnoye metro station, North-East Administrative District), cardiologists diagnose and treat tachycardia in children. Therapy begins with eliminating the root cause, and along the way, doctors select medications that alleviate the condition.
Causes of tachycardia in children
Do not forget that even normally, the heart rate (HR) of a child is significantly higher than that of an adult. This is due to a more active metabolism, leading to increased oxygen consumption by the cells of a growing organism. Heart rate norms for children of different ages are indicated in the table below:
| Child's age | Average heart rate (beats/minute) |
| Newborn up to 2 days | 123 |
| 2 – 6 days | 129 |
| 7 – 30 days | 148 |
| 30 – 60 days | 149 |
| 3 – 5 months | 141 |
| From six months to 11 months | 134 |
| 12 – 24 months | 119 |
| 34 years | 108 |
| 5 – 7 years | 100 |
| 8 – 11 years | 91 |
| 12 – 15 years | 85 |
| Over 16 years old | 80 |
The causes of tachycardia in children can be both physiological and pathological; associated with heart disease or resulting from other ailments.
With a healthy cardiovascular system, an increase in heart rate can be triggered by the following factors:
- hyperthermia due to acute respiratory viral infections or other infectious diseases;
- high ambient temperature;
- increased physical activity;
- emotional overexcitation;
- thyroid diseases;
- vegetative-vascular dystonia;
- overweight;
- pheochromocytoma;
- dehydration;
- anemia.
As for heart diseases, tachycardia in children is most often observed with congenital heart defects, myocarditis, and certain types of conduction disorders. Depending on the age of the child, one or another reason comes first.
In infants
Babies in the first months of life are most often exposed to attacks of tachycardia under the influence of the following factors:
- external mechanical influences, such as inspections or changing;
- cardiovascular failure;
- congenital developmental anomalies;
- perinatal encephalopathy;
- respiratory failure;
- acute asphyxia;
- hypoglycemia;
- anemia.
Naturally, a baby is not immune from the development of infectious diseases and, first of all, colds.
For schoolchildren
The reasons why tachycardia may develop in a child who has begun to attend school differ from those in an infant. By this time, congenital developmental anomalies partially lose their positions, since they have been cured, stabilized, or have already led to a sadder result, but continue to remain in first place. The frequency of acute asphyxia is also noticeably reduced. The main reasons for high heart rate in schoolchildren are:
- autonomic disorders due to increased stress, both psychological and physical;
- thyroid dysfunction;
- hyperthermia of various origins;
- organic heart pathologies;
- excessive physical activity;
- electrolyte dysfunctions;
- neoplasms.
The task of parents of schoolchildren who want to reduce the likelihood of tachycardia in their children is to normalize the regime, minimize physical and psychological stress on the child, undergo regular medical examinations and fight against infectious pathologies that can cause inflammation of the membranes of the heart.
All carious teeth need to be cured, and if a child has a sore throat or already feels discomfort in the heart due to an elevated temperature, then no exam or new topic should be a reason to postpone a visit to the doctor.
In teenagers
Adolescence is characterized by a significant increase in the development of risks for the cardiovascular system. This time marks the beginning of increased body growth, puberty with a characteristic surge of emotions, and the first experiments with the use of psychoactive substances.
Let's figure out what reasons cause rapid heartbeat in a teenager.
Their list is as follows:
- chronic infections (caries, frequent sore throats) that provoke inflammation of heart tissue;
- imbalance in growth rate between the heart (lags behind) and the rest of the body (leads);
- general passion for tonic low-alcohol drinks;
- “small heart” against the background of an underdeveloped musculoskeletal system;
- vegetative-vascular manifestations;
- electrolyte imbalance;
- tumors.
From this list, parents, even without contacting doctors, can cope with a good third of the reasons.
Boys and girls should be taught the negative effects of drinks containing caffeine and other stimulants. If he or she really wants alcohol before a disco, let him or her drink wine or vodka rather than Red Bull or Jaguar.
Symptoms
Symptoms of tachycardia largely depend on its type, form, root cause, age of the child and severity.
- Frequent heartbeat with normal blood pressure
Symptoms of an increase in heart rate in young children, even if they are caused by physiological reasons, may include the following:
- moodiness;
- restless behavior;
- loss of appetite or refusal to eat.
Older children may complain of weakness, dizziness and nausea, audible and tactile heartbeat, and chest discomfort. Episodes of physiological tachycardia in some cases are also accompanied by shortness of breath, pallor, sweating, loss of strength and even fainting.
With pathological tachycardia, the following symptoms are observed:
- pale skin;
- weakness;
- increased sweating;
- feeling of lack of air;
- swelling of the veins in the neck;
- nausea;
- frequent or less frequent urge to urinate;
- dyspnea;
- dizziness;
- feeling of fear of death;
- arterial hypotension or increased blood pressure;
- clapping heart sounds (with supraventricular paroxysmal tachycardia).
All of the above-described manifestations are variable and are determined by the form of the resulting tachycardia or its variety. The severity of these symptoms may also vary. Ventricular forms of tachycardia are very difficult to tolerate. They are especially dangerous in a newborn!
Tachycardia in a child is treated using conservative or surgical techniques.
What tachycardias are most common in children?
In a child, palpitations are divided into two main types:
- sinus;
- paroxysmal.
The first type occurs most often and, as a rule, against the background of a healthy heart.
Paroxysmal tachycardia is a whole group of diseases characterized by:
- sudden onset;
- high heart rate;
- spontaneous restoration of normal heart rhythm;
- preservation of the normal sequence of cardiac complexes on the ECG;
- short duration of the attack, from a few seconds to several days.
Frequency of occurrence in the pediatric population: 1 in 25,000 people, which is an average of 15% of all arrhythmias. Paroxysmal tachycardia is divided into the following forms:
- atrial;
- ventricular;
- atrioventricular.
Pathology develops as a consequence of such factors:
- congenital or acquired during childbirth pathology of the central nervous system;
- unfavorable family and social situation;
- congenital malformations of the child’s heart;
- cardiac surgery;
- some infectious pathologies;
- installation of a catheter in the heart cavity;
- heart trauma (closed);
- angiocardiography.
Another attack can be triggered by:
- mental stress;
- physical overload;
- hyperthermia;
- stress.
A child with paroxysmal tachycardia presents the following complaints:
- palpitations starting with a “push” behind the sternum;
- pain in the area of the heart and in the pit of the stomach;
- feeling of lack of air;
- dizziness;
- headaches;
- insomnia;
- weakness;
- nausea;
- fear.
As for changes on the ECG, they differ depending on the form of the disease and are indicated in the table below:
| Form of paroxysmal tachycardia | Changes on the cardiogram |
| Supraventricular | The P wave is associated with an unchanged QRS complex or is not detected, and can also have a wide variety of shapes. A sequence of extrasystoles of atrial origin is observed. Heart rate is from 160 beats/minute. |
| Ventricular | Short (five or more) sequences of extrasystoles of ventricular origin, alternating with short-term sinus intervals. The QRS complex is deformed, widened to 0.1 seconds or more. The P wave most often overlaps with other elements and is therefore almost never detected. |
This disease can be life-threatening for the child and requires emergency treatment.
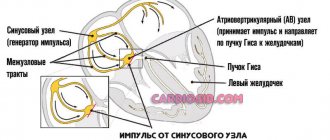
Sinus tachyarrhythmia in a child
This type occurs due to increased functioning of the sinus node. This condition can be provoked by a number of irritants:
- stress;
- dehydration;
- shock states;
- physical activity;
- an increase in the concentration of calcium ions in the blood;
- consumption of large doses of stimulants (tea, coffee);
- taking medications (caffeine, antidepressants, antiallergic drugs, theophylline and some others).
The main external distinctive signs of sinus tachyarrhythmia are:
- short duration;
- no significant discomfort;
- normalization of heart rate after removal of the influence of the irritating factor.
Tachycardia, which persists for a long time, can develop under the influence of various pathological conditions associated with both heart problems and diseases of other organs - anemia, respiratory failure, etc. In this case, an increase in heart rate is accompanied by certain complaints of moderate intensity: palpitations, sensation lack of air.
Sinus tachyarrhythmia is a condition characterized by a heart rate that exceeds the child’s age norm. It is based on the acceleration of the production of electrical impulses by the first-order pacemaker, the sinus node. In the absence of other symptoms, in addition to an increase in heart rate, sinus tachycardia is considered a normal variant.
With a significant acceleration of the heart, the child experiences the following symptoms:
- fatigue and weakness inappropriate for physical activity;
- emotional arousal;
- change in skin color;
- dizziness;
- heartbeat;
- moodiness;
- fussiness and so on.
Sinus tachycardia in most cases resolves spontaneously immediately after the influence of the provoking factor ceases.
To make a diagnosis of sinus tachycardia, the following methods are used:
- taking anamnesis;
- physical examination;
- types of ECG (regular, stress test, high resolution, Holter monitoring);
- electrophysiological study.
Differential diagnosis with other rhythm disturbances is of great importance. Sinus tachycardia of all arrhythmias has the most favorable prognosis.
Diagnostics
Diagnostic measures are based on collecting anamnesis.
The specialist asks the child’s parents when their health worsened, how it was expressed, and what measures were taken. This is followed by a physical examination:
- anthropometry;
- thermometry;
- auscultation and percussion;
- palpation.
If pathological changes in cardiovascular structures are suspected, screening examinations are recommended, namely:
- the frequency and rhythm of heart contractions can be easily observed on the ECG;
- 24-hour ECG monitoring is a safe and informative method;
- ECHO CG is performed to determine the nature of sinus disorder;
- blood tests allow you to determine endocrinological disorders, deviations in the parameters of glucose, hemoglobin, cholesterol;
- EEG allows you to exclude pathologies of brain structures.
Only the completeness of the information received by the specialist from the above diagnostic examinations allows him to conduct an adequate differential diagnosis and identify the true cause of the negative condition in the child.
How to act
When any type of arrhythmia appears in a child, parents are required to first call an ambulance. And only after the call or in parallel with it, begin to provide first aid:
- unfasten tight clothing on the child’s chest and neck;
- provide fresh air access to the room;
- Place a damp cloth on the patient's forehead.
It would be nice to try the so-called vagal tests:
- turn the baby upside down for half a minute; an older child can be helped to stand in his arms for the same time;
- ask him to tense his abdominals, strain, while holding his breath, press the child on the epigastrium (these actions are also performed for 30 - 40 seconds);
- press the root of the tongue and induce vomiting;
- Immerse the child’s face in a bath of cold water (procedure duration is from 10 to 30 seconds).
It is clear that these actions can only be performed with a child over 7-10 years old, to whom the meaning of the manipulations can be explained.
I would not recommend another test, which requires massaging the carotid sinus, without special preparation, since it is necessary to press the carotid artery.
These tests can bring a positive effect within half an hour from the onset of an attack of tachycardia.
When to see a doctor and how often to get checked
You should consult a doctor immediately after parents notice any of the above symptoms of any tachyarrhythmia. And it would be better to play it safe and bother the pediatrician in case of physiological tachycardia, which developed in response to stress or physical overload, than to miss the first “bells” indicating the onset of the development of a serious disease.
All children are covered by regular medical examinations from the moment of birth, so identifying arrhythmias should not be difficult. However, unfortunately, it is not always possible to detect symptoms and prescribe treatment for tachycardia in children in a timely manner.
There are several reasons for this:
- the formal attitude of pediatricians towards mass examinations of children;
- parents' inattention to children's complaints;
- Children's fear of doctors, which is why they do not tell their parents and doctors about their problems.
The solution is simple: attention to your own child and regular ECG diagnostics, especially during attacks.
A lot depends on parents regarding early diagnosis. After all, doctors, unfortunately, are not psychics and do not sense from a distance when the baby will develop the first attack of tachyarrhythmia in his life, but dad and mom are quite capable of noticing this and contacting a doctor in time.
An electrocardiogram is the most revealing method for detecting arrhythmias. The difference between sinus and paroxysmal tachyarrhythmias is indicated in the pictures below:
In what cases is treatment required?
Only a doctor should decide whether treatment is necessary in each specific case and what it will consist of! Self-medication for tachyarrhythmias can end very sadly. Prescriptions are made by a pediatric cardiologist or, in non-critical cases, by a pediatrician after consultation with a cardiologist. Treatment is carried out in accordance with approved protocols and can be either therapeutic or surgical.
Functional rhythm disturbances do not require treatment; it is enough to organize the child’s correct schedule of work, study, and rest.
A comprehensive approach should be taken to clinically significant arrhythmias. Therapy should begin with the removal of all chronic infectious foci and treatment of diagnosed rheumatism.
In the conservative treatment of childhood tachyarrhythmias, there are three main directions:
- bringing the electrolyte balance in the heart muscle to normal levels (preparations of magnesium and potassium ions);
- taking antiarrhythmic drugs (Verapamil, Propranolol, Amiodarone, etc.);
- improvement of metabolism in the myocardium (Riboxin, Cocarboxylase).
If rhythm disturbances are resistant to the action of drugs, then the turn comes to minimally invasive surgical interventions:
- radiofrequency or cryoablation of arrhythmogenic foci;
- implantation of a cardioverter-defibrillator or pacemaker.
In the vast majority of cases, arrhythmias that developed in childhood, subject to timely consultation with a doctor, are completely cured or stabilized.
The best for children
“AiF”: – Is high-tech cardiac care available for children in our country? For example, is it possible to get into your center?
L.M.: – Absolutely. Our center has patients from several environmentally disadvantaged regions of Siberia, the European part of our country, the North and the Far East, for whom we provide comprehensive examination and therapeutic treatment at the expense of budgetary funds. But we can accept Muscovites only according to quotas: our center is under federal subordination.
“AiF”: – Is there anywhere else besides Moscow that they diagnose and treat cardiac arrhythmias in children?
L.M.: – We have several strong arrhythmology schools – in Tomsk, Novosibirsk, St. Petersburg. But this, of course, is very little for such a large country as ours. There are also problems in the provision of diagnostic and therapeutic equipment. It is necessary to more actively implement advanced protocols for the examination and treatment of cardiac arrhythmias in children, which have been successfully practiced in the world for a long time. But I am an optimist and hope that the situation will change for the better.
Should parents worry?
Regardless of whether the child has complaints, parents should be attentive to the state of his health. Indeed, in the life of a growing organism there are 4 periods of risk for the appearance of arrhythmias, through which everyone goes through:
- newborn;
- from four to five years;
- from seven years to eight;
- from twelve to thirteen years old.
Children of these age groups must undergo mandatory electrocardiographic examination. If a child presents even one cardiogenic complaint, then doctors should prescribe additional types of ECG, various tests and examinations.
If problems are identified, then you need to start treating the child without delay. Most arrhythmias have a favorable prognosis. Clear recommendations on treatment tactics have been developed; in severe cases, surgical interventions are performed. Arrhythmia is not a death sentence; it must be fought and can be defeated, returning the child to a full life.
First aid
If a child has an attack of tachycardia, you should immediately call an ambulance. Until the doctors arrive, there are several ways to alleviate the baby’s condition.
Free his neck and chest from tight clothing, provide the patient with a sufficient flow of fresh air, and place a damp cloth or handkerchief on his forehead.
Case from practice
I bring to your attention a very illustrative case where a combination of a number of unpleasant circumstances and mistakes led to serious health problems for a young girl.
Thirteen-year-old K. was sent to a specialized cardiac surgery hospital with complaints of pulling and stabbing pain behind the sternum on the left, not periodic, not associated with the emotional state, physical activity and changes in body position. Painful attacks passed after taking sedatives or on their own. She had been noticing the sensations for a couple of years and came in due to the worsening of her condition.
Anamnesis of life
She was born full-term from the second pregnancy. There are no hereditary complications, bad habits, or professional hazards on the part of the parents. In the first half of pregnancy, the mother suffered from severe toxicosis. No examination for intrauterine infections was carried out.
As she grew older, she suffered from the following diseases:
- 1 year - no pathologies;
- 4 years - scarlet fever;
- 5 years - HES;
- 6 years old - lacunar tonsillitis.
At an older age, I occasionally suffered from ARVI.
Electrocardiography was not performed until the age of ten!
An ENT doctor diagnosed and observed chronic tonsillitis in the compensation stage.
Physically developed in accordance with age standards, harmoniously.
History of the disease
For the first time I felt pain in my heart when I reached the age of ten and addressed these complaints to a cardiorheumatologist.
A month later, the pain returned and began to appear more often. Extrasystole and atrial flutter appeared. This time K. was hospitalized and she was prescribed antiarrhythmic drugs, which, however, did not bring the expected effect. The girl was sent to a cardiac surgery hospital.
The ECG shows sinus arrhythmia, and the EchoCG shows enlargement of the left ventricle. Mitral valve prolapse was also detected, which at that time had not yet led to hemodynamic disturbances. The attending physician prescribed daily ECG monitoring, with the help of which attacks of atrial arrhythmia were detected.
The prescribed drug antiarrhythmic therapy was effective and led to a decrease in heart rate during attacks of atrial arrhythmia and the cessation of relapses of atrial fibrillation.
The child was observed in the clinic for six months. Despite supportive treatment, atrial tachyarrhythmia persisted. Echocardiography revealed enlargement of the right chambers of the heart. Considering that conservative treatment methods failed to achieve either a complete cure or even reliable stabilization of the condition, and the conduction system of the heart was under constant threat of inflammatory changes, it was decided to perform a biopsy of endomyocardial tissue using an intracardiac catheter.
During the examination of the biopsy specimen, tissue degeneration and the presence of a large number of leukocytes were revealed.
Subsequently, the girl was treated with cardioprotectors, antiarrhythmics, and anticoagulants.
Sluggish chronic tonsillitis was treated in order to eliminate the source of pathogenic microflora in the body.
After the entire complex of measures taken, K.’s well-being improved, relapses of arrhythmias were not observed, and the size of the heart returned to normal. However, there is dysfunction of the sinus node, and the patient is being monitored.
Conclusion
The patient came to this difficult situation for several reasons:
- lack of ECG control during periods of life that threaten the development of arrhythmias;
- the presence of an unsanitized chronic source of infection in the body;
- latent, sluggish, difficult to diagnose course of endomyocarditis.
To prevent such cases in other children, you should be more attentive to preventive examinations, observing the principle of overdiagnosis. In doubtful cases, it is better to refer the child for additional examination, which will show the norm, than to miss the pathology!
Treatment methods
The doctor determines treatment methods based on the general condition of the patient, the causes of tachycardia and its types. Depending on these factors, this may include drug therapy, physical therapy, sleep routine, and dietary nutrition. Directly during an attack, valgus techniques can be used, for example, blowing the auditory tubes using the Vasiliev method.
In exceptional cases, the cause of palpitations in a minor may be an organic heart disease. A very common option is the appearance of additional pathways. In this case, surgical intervention is required.
Doctor's advice
In conclusion, I want to give some simple advice to those parents who want to minimize the risk of developing arrhythmias in their child:
- do not hesitate to ask the doctor for a referral for an ECG during the risky periods of the child’s life listed above;
- interpretation of children's ECGs from periodic examinations should be carried out in the department of functional diagnostics;
- sanitize all foci of chronic infection - carious teeth, diseases of the ENT organs, respiratory tract, skin;
- the child should sleep enough, eat well, drink plenty of fluids, and avoid eating synthetic and GMO foods;
- he should, if possible, be protected from unnecessary stress and heavy physical activity;
- At the slightest complaint, the child should be shown to specialists.
And remember that any disease, especially arrhythmia, is much easier to prevent than to treat.
Normal heart rate during sports activity
All athletes, not just children, must monitor their health. The easiest way is to measure your heart rate before and after exercise. In this case, you need to especially pay attention to the frequency of the beats and their rhythm. It is obvious that there is a certain connection between sports activity and the number of heart beats per minute. The higher the load, the faster the heart beats. Calculation formula: (HRmax-NPP)* %HRmax+NPP
- HRmax – maximum heart rate according to the Roberges-Landwehr formula. 205.8-(0.685*age).
- %HRmax is the percentage of the maximum heart rate. 50-60% is a warm-up. In untrained people, such a pulse may appear during normal walking. 60-70% is the fat burning zone. At this time, the overall endurance of the body is developed. It is recommended to stay in it most of the time during training.
- 70-80% – aerobic zone or cardio zone. At this time, the stroke volume of the heart increases.
- 80-90% is anaerobic zone. Speed, strength and muscles increase.
- 90-100% is the competition zone. This is the maximum load zone. You shouldn’t let it get to this point, it’s simply unhealthy.
- RPP – resting heart rate. Measured immediately after waking up in the morning. As described above, subject to change.
Tables can be found on the Internet. In athletic children, the pulse is restored 10 minutes after stopping the exercise.
But the most important advice for parents is that parents need to monitor the child’s health. If unusual abnormalities occur, contact your doctor immediately. The child’s body recovers from illness quite easily, so even in serious cases, therapy usually ends in the child’s recovery.
Increasing acetone
A rapid deterioration in the child's condition can be caused by acetonemic intoxication. In this case, a rapid heartbeat appears in a child of 5 years or another age. You can also determine the pathological condition of the baby by some other signs. We will list the main ones in this article, since the disease is very dangerous, you should know exactly about its signs in order to recognize it in time and immediately seek qualified medical help.
An increase in the level of acetone in the body in a minor can be determined by the following symptoms:
- Cardiopalmus.
- Abdominal pain in the form of cramps.
- Severe and sharp vomiting, repeated many times.
- Weakness, nausea, pale skin.
- Pungent odor of acetone in urine, vomit and on breath.
- Dehydration of the body.
- Increased body temperature.
- Retardation of movements, convulsions, photophobia, loss of consciousness.
If a child has acetone in his urine, you should consult a doctor as soon as possible. During the treatment period, alkaline drinking, a special diet, and restoration of normal glucose levels in the child’s body are recommended.
Requirements and recommendations
In order for the child’s treatment to be as productive and effective as possible, adults must adhere to all medical recommendations received, as well as organize the correct diet and appropriate daily routine for the young patient.
Coffee, tea, spicy and salty foods, and products containing cocoa must be excluded from the patient’s diet. The diet should be rich in fiber, nutritious, and rich in light carbohydrates. Particular attention should be paid to protein foods - their quantity should be limited.
In some cases, parents can use traditional medicine to combat arrhythmia. Such methods should only be used if the disease does not have a functional origin. In addition, you should definitely consult your doctor.