1.What is mitral valve regurgitation?
Mitral valve regurgitation
characterized by an unnatural flow of blood from the left ventricle into the left atrium during
systole
- contraction of the heart muscle.
When the heart valve is working properly, blood moves from the atrium to the ventricle. Against the background of rheumatic fever, dilation of the mitral valve ring, ischemic dysfunction of the papillary muscles and other unfavorable factors, the direction of blood flow changes in the opposite direction.
According to statistics, about 70% of the world's population is affected by mitral regurgitation. Minor manifestations of this pathological process can occur even in absolutely healthy people.
A must read! Help with treatment and hospitalization!
Short description
As you know, the main job of the heart muscle is to continuously transport blood throughout the human body and saturate it with oxygen.
In the heart itself, blood moves in a certain order from one section to another, after which it continues its movement through the veins in the systemic circulation.
With regurgitation, a reverse movement of blood occurs in various volumes, and the severity of symptoms depends on the indicators of the latter.
Regurgitation is a pathological process indicating improper functioning of the heart muscle due to a serious disease. This condition has 5 stages of development. Each of them needs to be considered:
- Regurgitation 1st degree. It is this stage that is called mild and at this moment is of greater interest. The pathological process occurring in the heart during the first stage can be described as follows: blood entering the cardiac ventricle flows out of it into the atrium through the valve leaflets.
- Grade 2 regurgitation cannot be ignored and must be treated. The flow of blood flow from the valves exceeds 25 mm.
- Regurgitation of the 3rd degree is diagnosed if the blood stream exceeds 2 cm. This phenomenon should in no case be ignored, the patient is registered.
- Stage 4 disease - blood flow exceeds 2.5 cm.
- Grade 5 is considered a physiological feature of a person. That is, if the pathology does not develop, it does not pose a threat to human life.
2.Why does mitral regurgitation occur?
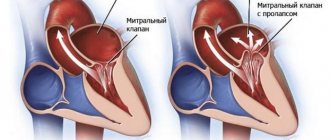
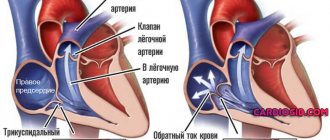
The mitral valve is a kind of valve that separates the left atrium from the ventricle. Due to various factors that impair its functioning, the valve does not fit tightly enough to the walls of the ventricle. As a result, the two connecting plates - components of the valve - cannot effectively block the reverse flow of blood, placing additional stress on the heart to normalize the circulation of blood flow. This phenomenon does not pass without leaving a trace on the human body. The consequences of mitral valve regurgitation can include diseases such as arrhythmia, heart failure and endocarditis.
There are two main forms of mitral regurgitation: chronic and acute. Let us consider in more detail their differences and features of the course.
- Acute mitral regurgitation.
Acute regurgitation of the mitral valve occurs against the background of various cardiac pathologies: dysfunction or rupture of the papillary muscles, acute rheumatic fever, infective endocarditis, rupture of the mitral valve leaflets, dilatation of the left ventricle. Acute regurgitation develops instantly. Due to possible severe bleeding caused by rupture of cardiac tissue, it can be life-threatening. - Chronic mitral regurgitation.
The causes of chronic regurgitation of the mitral valve are also associated with heart diseases - mitral valve prolapse, expansion of its ring. The chronic form of regurgitation is much more common than the acute form. It is characterized by slow and gradual development, so the disease is most often diagnosed in older people.
Visit our Cardiology page
Mitral regurgitation
Mitral valve regurgitation
(mitral regurgitation, mitral valve regurgitation, mitral regurgitation (MR))
is the inability of the mitral valve to prevent blood from flowing back from the LV during its systole into the left atrium. The term “mitral regurgitation” refers specifically to the reverse flow of blood from the LV to the left atrium, i.e. a consequence of mitral regurgitation. Nevertheless, the terms have become practically synonymous.
Etiology
The mitral valve apparatus is represented by the mitral valve leaflets, chordae tendineae, papillary muscles and the fibrous annulus of the mitral valve. Pathology of any of these structures can lead to the development of MR. The most common causes of MR are:
- rheumatic fever (in such cases, MR is almost always combined with MC);
- mitral valve prolapse syndrome;
- cardiac ischemia;
Scheme
Functional classification of mitral regurgitation according to Carpentier. Classification of the range of motion of the mitral leaflet: type I – movement is not limited; type II – excessive mobility; type III – restriction of mobility
Clinic
During the compensation period, which can last several years, mitral regurgitation may be asymptomatic. In the subcompensation stage, subjective symptoms appear, expressed by shortness of breath, fatigue, tachycardia, anginal pain, cough, and hemoptysis. As venous stagnation in the pulmonary circulation increases, attacks of nocturnal cardiac asthma may occur. The development of right ventricular failure is accompanied by the manifestation of acrocyanosis, peripheral edema, liver enlargement, swelling of the neck veins, and ascites. When the recurrent laryngeal nerve is compressed by the dilated left atrium or pulmonary trunk, hoarseness or aphonia occurs (Ortner's syndrome). In the decompensation stage, more than half of patients with mitral insufficiency have atrial fibrillation.
Radiolic finds
Radiography
- Increased size of the left atrium.
- Increased size of the left ventricle.
- Signs of stagnation in the pulmonary circulation.
- Curley B lines
Ultrasound Echocardiography
To assess the degree of mitral regurgitation, there are a number of echocardiographic indicators. First of all, you should focus on such a parameter as the width of the vena contracta - the size of the convergent flow of regurgitation immediately under the leaflets. The vena contracta correlates with the diameter of the regurgitant orifice and therefore with the severity of the regurgitation. Mild regurgitation is characterized by a narrow vena contracta, the width of which is less than 3 mm; in severe MR, this parameter is 7 mm or more. More accurate indicators are obtained in the parasternal projection along the long axis of the heart. To optimize visualization of the vena contracta and increase measurement accuracy, it is preferable to use the magnification mode. Transverse section of the vena contracta is recognized as an effective regurgitant lumen and is also the recommended measurement method.
The method of assessing the proximal isovelocity surface or proximal regurgitant zone is a method of calculating the effective area of the regurgitant orifice, based on an assessment of the convergence zone of the regurgitant flow. If it is 1.0 cm or more, then MR should be considered severe. Having determined the radius of the proximal regurgitation zone at the beginning of diastole, the maximum speed of the regurgitation flow and knowing the speed at which the aliasing effect appears (the speed limit for the occurrence of the spectrum reversal phenomenon), we can calculate the effective area of the regurgitation orifice according to the formula EROA=6.28 R2 × integrated into the device Alias V / MR V. Effective regurgitation orifice area EROA 0.4 cm2 or more corresponds to severe MR, EROA no more than 0.2 cm2 indicates mild regurgitation.
Regurgitation flow area
determined by color Doppler ultrasound as the ratio of the area of the regurgitant flow to the area of the atrium with a Nyquist limit of 50–60 cm/s. The calculation of the regurgitation flow area index is obtained in a four- or two-chamber position in LV systole using a planimetric method of tracing the contours of the regurgitation flow using a correction factor (0.785) to the LA area. However, the use of this technique is limited by the possibility of error or incorrect interpretation of the data obtained. With atriomegaly, the severity of mitral regurgitation may be underestimated. If the jet is eccentric, it is impossible to assess its significance in one plane. Thus, this research technique allows one to obtain a rather rough idea of the volume of regurgitation, and is therefore considered to be uninformative and extremely dependent on signal amplification settings.
Scheme
Echocardiographic indicators for assessing the mitral valve during LV remodeling: a – normal; b – with LV remodeling, the angles of both MV leaflets increase; c – with further remodeling of the LV, the angle of the AMC (α2) can progressively increase, while the angle of the AMC (α1) decreases or the AMC – anterior mitral leaflet – does not change; PMS - posterior mitral leaflet
Echocardiography video
patient with mitral regurgitation.
Source
— Internal diseases — Volume 1 — textbook edited by Academician of the Russian Academy of Medical Sciences V.S. Moiseev, Academician of the Russian Academy of Medical Sciences A.I. Martynov, Academician of the Russian Academy of Medical Sciences N.A. Mukhina. - Radiopaedia.org - N.O. Sokolskaya, I.V. Slivneva ECHOCARDIOGRAPHIC CRITERIA FOR ASSESSING MITRAL INSUFFICIENCY OF ISCHEMIC GENESIS FSBI Scientific Center for Cardiovascular Surgery named after. A.N. Bakulev" (director - academician of the Russian Academy of Sciences and Russian Academy of Medical Sciences L.A. Bokeria).
3. Symptoms of the disease
Chronic mitral regurgitation is characterized by the absence of symptoms for many years. As a rule, patients do not know about heart disease for a long time, the symptoms of which appear gradually. The acute form of regurgitation is much more serious and is accompanied by the same symptoms as cardiogenic shock and acute heart failure.
We list the main symptoms of mitral valve regurgitation:
- constant shortness of breath;
- weakness and increased fatigue;
- dizziness;
- pain in the chest;
- confusion;
- swelling of the lower extremities.
If you notice at least two of the above symptoms, be sure to contact a good cardiologist. You may need immediate treatment.
About our clinic Chistye Prudy metro station Medintercom page!
Factors in the development of the disease
Doctors identify the following most common causes of the development of this disease:
- Increased blood pressure in arterial hypertension. This is due to the heavy load on the heart, the right side of which begins to function improperly over time. In most cases, the cause of the pathology is secondary hypertension. It can be caused by both concomitant complex diseases (for example, HIV) and bad habits (drug use).
- Infectious endocarditis is the presence of pathogenic pathogens in the heart muscle and, as a result, damage to the valve.
- Dilatation of the pulmonary artery is a strong dilatation of blood vessels while maintaining the functionality of the valve. This condition is considered a pathology.
- Various sexually transmitted diseases, such as syphilis.
- Rheumatism.
- Formation of malignant tumors (oncological diseases).
- Tetralogy of Fallot is a syndrome in which a person simultaneously suffers from four heart defects. These include: narrowing of the pulmonary artery, defects in the structure of the septum between the ventricles of the organ, blood flow disorders and aortic insufficiency.
Typically, tetralogy of Fallot is diagnosed in early childhood due to severe symptoms in a child who is immediately operated on. The disease in question often causes thickening of the walls of the right heart ventricle. This, in turn, can lead to the development of heart failure. In another case, an existing pathology can provoke the occurrence of this disease.
In medicine there is the concept of physiological regurgitation. This condition is called physiological only if the changes resulting from pathology are insignificant. That is, the blood flow at the valve slows down, but the heart muscle does not undergo any negative changes and remains healthy. Typically, grade 1 regurgitation is considered a physiological phenomenon.
4. Diagnosis and treatment of mitral valve regurgitation
Diagnosis of mitral valve regurgitation may include:
- medical examination;
- echocardiogram - a procedure based on the use of sound waves to determine the shape, size and structure of heart tissue;
- chest x-ray;
- electrocardiogram of the heart, which allows to detect irregularities in the heart rhythm;
- cardiac catheterization - examination of the cavities of the heart, as well as nearby blood vessels, using a hollow flexible tube.
These tests not only detect mitral regurgitation, but also determine the degree of mitral regurgitation. The information obtained during the study is the basis on which further treatment is based.
The choice of treatment for mitral valve regurgitation depends primarily on the form of the disease, as well as the degree of its progression.
For example, in chronic cases, doctors most often prescribe constant monitoring of the patient’s heart condition and the use of special medications to eliminate the symptoms of the disease. These drugs include:
- vasodilators – a group of vasodilating drugs;
- diuretics and diuretics;
- anticoagulants - drugs that prevent the formation of blood clots.
If necessary, your doctor may recommend surgery to repair or replace the mitral valve. Patients with mitral regurgitation need to radically change their lifestyle in order to reduce the load on the heart. Doctors recommend avoiding intense physical activity and emotional stress, leading a healthy lifestyle and eating right.
Diagnostics
For the initial diagnosis of mitral valve prolapse with grade 1 regurgitation, routine listening to the chest using a stethoscope is sufficient. With grade 0-1 MVP, a click will be heard immediately after ventricular contraction. If the patient is suffering from MVP with stage 2 regurgitation, then when listening with a stethoscope the blood will be heard as a “whooshing” sound immediately after the click.
But the most accurate diagnostic test is echocardiography. Only with the help of echocardiography can a cardiologist determine the degree of mitral regurgitation.
Symptoms of the disease
In most cases, stage 1 of the disease does not have clearly defined symptoms. Some patients may experience signs of heart failure.
If the sick person does not have this ailment, such symptoms may occur due to impaired functioning of the right cardiac ventricle. Regurgitation of the 1st degree as an independent pathology does not cause significant disturbances in the human circulatory system.
If a person has stage 2 or 3 of the disease, then a large amount of blood entering the right heart ventricle can lead to organ failure.
This is due to the expansion of the chambers and thickening of the walls of the heart muscle.
Despite the hidden heart defect at the first stage, some patients experience the following symptoms:
- severe shortness of breath;
- blue discoloration of the skin;
- mild hypertension;
- swelling;
- weakness;
- dizziness.
In cases where this pulmonary artery defect is congenital, the disease manifests itself in the first few months of the child’s life. Most sick children have severe symptoms due to the severe form of the disease.
If a newborn suffers from grade 4 regurgitation, then the disease cannot be corrected, in which case death is possible.
It is for this reason that both adults and children should annually undergo appropriate procedures and tests that will help identify the disease at an early stage.