How does the left ventricle work?
The left ventricle is a cavity formation.
Its volume depends on the person’s age and type of activity, since the myocardial muscles are amenable to “training”. The thickness of the LV wall is 10-14 mm and consists of three layers in which the fibers have different directions (circular, straight and oblique). The inside of the chamber is lined with endocardium, a connective tissue membrane that forms valves near the atrioventricular openings. The shape of the left ventricle is oblong-oval, cone-shaped. There are two divisions of the structure:
- apex - a narrow part, which in a healthy person is located in the 4-5 intercostal space on the left;
- the outer edge is a rounded contour that forms the lateral (pulmonary) surface - the most massive part of the heart muscle.
Inside, the LV consists of two parts: the posterior and anterior sections, through which blood gradually moves from the chamber cavity to the aortic cone.
In the area of the atrioventricular opening there is a valve consisting of two leaflets made of endocardial tissue. The main task of this structure is to regulate blood flow and prevent regurgitation (backflow). Attached to the ventricular myocardium by papillary (papillary) muscles, the tone of which determines the amplitude of movement of the valves.
The aortic valve is represented by three semilunar valves, which are attached around the circumference of the opening between the conus arteriosus and the aorta. The coordinated operation of the valves ensures the movement of fluid into the systemic circulation during contraction of the LV myocardium and prevents regurgitation when the chamber is filled during diastole.
The excitation wave that causes the ventricle to contract passes from the atrioventricular junction along the left bundle branch and its two branches. Cardiomyocytes located at the apex of the heart receive impulses through Purkinje fibers.
Anatomy of the cardiovascular system
In order to talk about diseases of the cardiovascular system, it is necessary to understand its structure. The circulatory system is divided into arterial and venous. Through the arterial system, blood flows from the heart, through the venous system it flows to the heart. There are large and small circles of blood circulation.The great circle includes the aorta (ascending and descending, aortic arch, thoracic and abdominal sections), through which blood flows from the left side of the heart. From the aorta, blood enters the carotid arteries that supply blood to the brain, subclavian arteries, blood supply to the arms, renal arteries, arteries of the stomach, intestines, liver, spleen, pancreas, pelvic organs, iliac and femoral arteries, and blood supply to the legs. Blood flows from the internal organs through veins that drain into the superior vena cava (collects blood from the upper half of the body) and the inferior vena cava (collects blood from the lower half of the body). The vena cava drains into the right heart.
The pulmonary circulation includes the pulmonary artery (through which, however, venous blood flows). Through the pulmonary artery, blood enters the lungs, where it is enriched with oxygen and becomes arterial. Through the pulmonary veins (four), arterial blood enters the left heart.
The heart pumps blood - a hollow muscular organ consisting of four sections. These are the right atrium and right ventricle, which make up the right heart, and the left atrium and left ventricle, which make up the left heart. Oxygen-rich blood coming from the lungs through the pulmonary veins enters the left atrium, from there into the left ventricle and then into the aorta. Venous blood enters the right atrium through the superior and inferior vena cava, from there into the right ventricle and further through the pulmonary artery into the lungs, where it is enriched with oxygen and again enters the left atrium.
There are pericardium, myocardium and endocardium. The heart is located in the cardiac sac - the pericardium. Cardiac muscle - the myocardium consists of several layers of muscle fibers; there are more of them in the ventricles than in the atria. These fibers, contracting, push blood from the atria into the ventricles and from the ventricles into the vessels. The internal cavities of the heart and valves are lined by the endocardium.
- Right coronary artery
- Anterior descending artery
- Ear
- Superior vena cava
- Inferior vena cava
- Aorta
- Pulmonary artery
- Branches of the aorta
- Right atrium
- Right ventricle
- Left atrium
- Left ventricle
- Trabeculae
- Chords
- Tricuspid valve
- Mitral valve
- Pulmonary valve
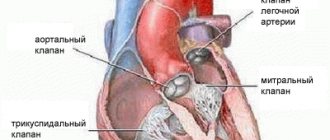
Valvular apparatus of the heart.
Between the left atrium and the left ventricle there is a mitral (bicuspid) valve, and between the right atrium and the right ventricle there is a tricuspid (three-leaf) valve. The aortic valve is located between the left ventricle and the aorta, the pulmonary valve is between the pulmonary artery and the right ventricle.
Work of the heart.
From the left and right atria, blood flows into the left and right ventricles, while the mitral and tricuspid valves are open, the aortic and pulmonary valves are closed. This phase in the work of the heart is called diastole. Then the mitral and tricuspid valves close, the ventricles contract and through the opened aortic and pulmonary valves, blood rushes into the aorta and pulmonary artery, respectively. This phase is called systole, systole is shorter than diastole.
Conduction system of the heart.
We can say that the heart works autonomously - it itself generates an electrical impulse that spreads through the heart muscle, causing it to contract. The pulse must be generated at a certain frequency - normally about 50-80 pulses per minute. In the conduction system of the heart, the sinus node is distinguished (located in the right atrium), from which nerve fibers go to the atrioventricular (atrioventricular) node (located in the interventricular septum - the wall between the right and left ventricles). From the atrioventricular node, nerve fibers run in large bundles (right and left bundle branches), dividing into smaller bundles in the walls of the ventricles (Purkinje fibers). An electrical impulse is generated in the sinus node and spreads through the conduction system throughout the myocardium (heart muscle).
Blood supply to the heart.
Like all organs, the heart must receive oxygen. Oxygen is delivered through arteries called coronary arteries. The coronary arteries (right and left) arise from the very beginning of the ascending aorta (at the origin of the aorta from the left ventricle). The trunk of the left coronary artery is divided into the descending artery (also known as the anterior interventricular) and the circumflex artery. These arteries give off branches - the artery of the obtuse edge, diagonal, etc. Sometimes the so-called median artery branches off from the trunk. The branches of the left coronary artery supply blood to the anterior wall of the left ventricle, most of the interventricular septum, the lateral wall of the left ventricle, and the left atrium. The right coronary artery supplies part of the right ventricle and the posterior wall of the left ventricle.
Now that you have become an expert in the anatomy of the cardiovascular system, let's move on to its diseases.
Main functions of the department
The left ventricle of the heart is responsible for the following functions:
- systolic - synchronous contraction of cardiomyocyte fibers ensures adequate release into the systemic circulation to supply all organs and tissues with oxygen;
- diastolic - relaxation of the walls of the ventricle, opening of the atrioventricular valve and filling the cavity with blood from the atrium.
The normal pumping function involves the coordinated work of all departments. The cardiac cycle consists of alternating states: systole and diastole, which are characterized by contraction and stretching of the muscle fibers of cardiomyocytes.
Periods of the systolic phase:
- tension with the stage of asynchronous and isometric contraction;
- expulsion (two periods - fast and slow).
The asynchronous period is characterized by an uneven distribution of the excitation impulse, so individual fibers do not contract simultaneously. This phase is necessary for complete closure of the mitral valve leaflets, after which intraventricular pressure increases (due to the ongoing contraction of cardiomyocytes). Having reached a level of 70-80 mm Hg. Art., the semilunar valves open and blood enters the aorta (at first quickly, and then more slowly). The closure of the valve is caused by high pressure inside the vessel.
Relaxation of the myocardium of the LV walls opens the mitral valve, which starts the flow of a new portion of blood. To ensure adequate ejection, it is necessary that all parts of the ventricle, leaflets, papillary muscles, trabeculae and chords are in good functional condition.
Cardiac hypertrophy
Cardiac hypertrophy
Cardiac hypertrophy is an enlargement of the heart muscle, which occurs mainly due to an increase in the number of cardiomyocytes - specialized muscle cells of the heart. This condition occurs in children, adolescents, young adults and the elderly.
Cardiac hypertrophy is a manifestation of a special state of the body: physiological or pathological. That is, it is not a disease, but a symptom.
Physiological
Physiological hypertrophy of the heart is observed in athletes and people who lead an active lifestyle. For regular physical activity, the body requires large amounts of oxygen. Oxygen is delivered through the blood. And to meet the increased oxygen needs, the heart increases the frequency and strength of contractions. And this requires greater metabolism in the heart muscle itself. This gradually increases the volume and mass of cells (cardiomyocytes). More often in athletes, cardiac hypertrophy begins from the left ventricle. Sports that can lead to cardiac hypertrophy are rowing, hockey, football, cross-country skiing, cycling, long-distance running, etc. When you stop training, this condition reverses. That is, the hypertrophied heart again becomes of normal size with normal wall thickness.
Pathological
Pathological hypertrophy of the heart occurs due to various diseases of the body. The human heart consists of four sections: two atria and two ventricles. The atria are reservoirs where blood enters from the body's circulation (blue vessels). The ventricles are a buoyant force that pushes blood through the vessels (red vessels). So each department has its own reasons for increasing.
Causes:
- Left ventricle – enlarges due to arterial hypertension, aortic valve stenosis, aortic atherosclerosis, general obesity, diabetes mellitus
- Right ventricle – due to congestive heart failure, chronic pulmonary failure
- Left atrium – with arterial hypertension, general obesity, aortic and mitral valve defects
- Right atrium - due to pulmonary diseases (when there is stagnation in the pulmonary circulation).
Development
The above reasons force us to maintain normal blood flow by increasing the mass of the heart. It must be taken into account that an increase in one part of the heart leads to hypertrophy of another. In addition to cardiomyocytes, the heart also contains connective tissue. With cardiac hypertrophy, it also grows, and this leads to a decrease in the elasticity of the walls and disruption of the heart.
If the load on the heart does not decrease, then the myocardium is gradually depleted because the blood flow cannot cope with the nutrition of the enlarged heart. This can lead to disruption of nerve impulses (arrhythmia), sclerosis and atrophy of the heart muscle.
Symptoms
- An asymptomatic course of cardiac hypertrophy is possible.
- If the left half of the heart is affected: pain in the heart area (increases after physical activity), arrhythmia, loss of consciousness, shortness of breath, dizziness.
- If the right half of the heart is affected: cough, shortness of breath, cyanosis (cyanosis) or pallor of the skin, swelling, arrhythmia.
Diagnostics
- Ultrasound examination of the heart
- ECG (electrocardiography)
- X-ray of the chest organs.
Treatment It is necessary to eliminate the cause of cardiac hypertrophy.
If it is arterial hypertension, it is necessary to take antihypertensive and diuretic drugs. Severe heart valve defects require surgical treatment and prosthetics. Respiratory diseases require anti-inflammatory and bronchodilator therapy. In any case, the approach is always individual. To monitor blood pressure and early detect arrhythmia, I recommend using automatic tonometers from the manufacturer Microlife, presented in our online store.
The author of the article is a practicing neurologist Maxim Nikolaevich Starshinin.
Diagnosis of diseases: what methods will determine the problem?
There are two types of left ventricular dysfunction (dysfunction):
- Systolic, which is characterized by a decrease in the ejective capacity of the LV. Most often, pathology develops when contractile cardiomyocytes are damaged during myocardial infarction, inflammatory or autoimmune disorders.
- Diastolic. It is characterized by the inability of muscle fibers to completely relax and create the required volume of the chamber (the condition is most often diagnosed with pathologies of the pericardium or neighboring structures).
If you have complaints of shortness of breath during exercise or at rest, swelling in the legs, cough, pain in the heart area, you should contact a cardiologist and undergo a comprehensive examination to find out the cause.
ECG
Using electrocardiography (ECG), it is possible to identify not only the correct rhythm and heart rate, but also disturbances in the functioning and structure of the left ventricle. Signs of ECG changes in various LV pathologies:
- Hypertrophic changes in the walls of the left ventricle, regardless of the cause:
- displacement of the electrical axis of the heart to the left (angle α ranges from -90 to 0°);
- intraventricular conduction disorders (complete or incomplete blockade of the left bundle branch);
- repolarization disorders – deformation of the T wave in I, aVL, V5, V6.
- Scarring in the area of the left ventricle:
- altered Q wave in leads I, II, aVL, as well as in V1-6;
- location of ST on an isoline;
- low and flattened T wave.
Ultrasound
Ultrasound or echocardiography (echocardiography) helps determine the size of the heart chambers and the thickness of their walls, assess the functional state of the valves, and the efficiency of myocardial contraction. Each department has its own standard indicators.
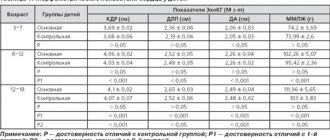
The main ultrasound parameters of the LV are presented in the table.
| Criterion | Standards | Changes |
| Muscle mass |
| Enlargement – with hypertrophy (symmetric and asymmetric growth are distinguished) |
| Myocardial mass index (LVMI) |
| |
| Interventricular septal thickness (IVS) |
|
|
| End-diastolic volume (EDV) |
| |
| Final size |
| |
| Ejection fraction (EF) | 55-60% | A decrease in the indicator is characteristic of left ventricular systolic dysfunction |
| Stroke volume (SV) | 60-100 ml |
|
Scintigraphy
Perfusion scintigraphy is a method for assessing the blood supply to the muscular layer of the left ventricle using radiopharmaceuticals that are administered intravenously and accumulate in the myocardium. The advantage of the study is the accurate detection of ischemia even in small vessels, which is not always possible to detect with angiography. Scintigraphy can be static (performed at rest) and dynamic (during dosed physical activity on a bicycle ergometer).
Indications:
- myocardial ischemia of unknown origin;
- assessment of the effectiveness of operations to restore coronary blood flow (angioplasty, bypass surgery, etc.);
- studies of myocardial blood flow in non-coronary diseases (mainly inflammatory in nature);
- with a questionable ECG (to confirm the diagnosis of acute myocardial infarction).
MRI and CT
Recently, X-ray methods for studying the heart have become in demand, which make it possible to obtain three-dimensional images of the organ and identify changes in the structure.
Computed tomography (CT) takes a series of X-rays of the heart from different angles in separate sections of the organ. Modern devices are capable of providing three-dimensional visualization of the internal structure.
Magnetic resonance imaging (MRI) has a similar principle. However, the study does not use ionizing radiation, but waves of a magnetic nature. Tissues “respond” to this influence in different ways, which is what the device records.
Both methods can provide the following information:
- LV wall thickness;
- changes due to myocardial infarction;
- condition of blood vessels, presence of atherosclerotic plaques;
- hemodynamic adequacy;
- condition of the pulmonary arteries.
Heart failure - symptoms and treatment
The following forms of heart failure are distinguished:
- left- and right-handed;
- systolic and diastolic (heart failure with reduced and preserved ejection fraction);
- acute and chronic.
Left ventricular failure
Left-sided heart failure can be left ventricular or left atrial. It is characterized by a decrease in left ventricular output and/or stagnation of blood on the way to the left parts of the heart, that is, in the veins of the pulmonary circulation.
Left ventricular failure usually develops with coronary heart disease (CHD), hypertension, cardiomyopathy, congenital heart defects, heart valve insufficiency, and left atrial failure - with narrowing of the mitral valve opening and, in rare cases, with left atrial myxoma - a benign heart tumor [14].
Symptoms of left-sided heart failure (HF): weakness, dizziness, pale skin, shortness of breath and fatigue.
Right ventricular failure
Right ventricular failure is characterized by a decrease in right ventricular output and stagnation of blood in the veins of the systemic circulation. The condition is usually caused by pre-existing left ventricular failure or severe pulmonary disease [14].
Symptoms of right-sided heart failure: peripheral edema, cyanosis and fluid accumulation in the abdominal cavity.
Isolated heart failure is rare and short-lived. Subsequently, the disorder affects all chambers of the heart and typical symptoms of the disease develop.
Some sources use the term “global heart failure” to describe heart failure of both ventricles. This formulation is incorrect and is not used by doctors. In the literature, the term “total heart failure” is used to describe this condition [17].
Systolic and dystolic heart failure
Impaired pumping function of the left ventricle can be caused by systolic and diastolic dysfunction. Systolic dysfunction is more common and is associated with decreased contractility of the myocardium, the muscle tissue of the heart. In most cases, the cause of systolic chronic heart failure is coronary artery disease, combined with arterial hypertension and diabetes mellitus.
Diastolic dysfunction is caused by impaired active relaxation or increased myocardial stiffness. Patients with this form of the disease are less likely to suffer from coronary artery disease, and more often from arterial hypertension and atrial fibrillation. Among them there are more elderly people, women and obese patients[16].
In addition to the familiar terms “diastolic heart failure” and “systolic heart failure,” the names “ heart failure with preserved LV ejection fraction (HFpEF) ” and “heart failure with reduced ejection fraction (HFrEF)” .
We are talking about the same conditions, but the use of the terms diastolic and systolic HF requires objective evidence obtained using echocardiography, magnetic resonance imaging and isotope studies of the heart. In some sources, these terms are used as synonyms [14][18].
Symptoms for systolic and diastolic HF are similar [13]. These forms of the disease can only be distinguished using instrumental diagnostic methods. Many patients experience both types of dysfunction simultaneously [17].
Acute and chronic heart failure
Symptoms of chronic and acute heart failure differ only in intensity and timing of development.
Stages of development of heart failure
The modern classification of chronic heart failure combines the modified classification of the Russian School of Cardiology according to stages that can only worsen (V. Kh. Vasilenko, M. D. Strazhesko, 1935), and the international classification according to functional classes, which are determined by the patient’s ability to tolerate physical activity (6-minute walk test) and may worsen or improve (New York Cardiology Classification).[2]
Classification of CHF by the Russian Society of Heart Failure Specialists
| FC | FC of CHF (may change during treatment) | NK | Stages of CHF (do not change during treatment) |
| 1FC | There are no restrictions on physical activity; increased workload is accompanied by shortness of breath and/or slow recovery | 1 tbsp | Hidden heart failure |
| 11FC | Minor limitation of physical activity: fatigue, shortness of breath, palpitations | 11a st | Moderately severe hemodynamic disturbances in one of the circulation circles |
| 111FC | Noticeable limitation of physical activity: compared with usual activities, accompanied by symptoms | 11b st | Severe hemodynamic disturbances in both circulation circles |
| 1U FC | Symptoms of heart failure are present at rest and worsen with minimal physical activity. | 111st | Severe hemodynamic disturbances and irreversible structural changes in target organs. The final stage of damage to the heart and other organs |
New York Heart Association classification of heart failure
Class I: Heart disease does not limit physical activity. Normal exercise does not cause fatigue, palpitations or shortness of breath.
Class II. The disease slightly limits physical activity. There are no symptoms at rest. Normal physical activity causes fatigue, palpitations, or shortness of breath.
Class III. Physical activity is significantly limited. There are no symptoms at rest. Little physical activity causes fatigue, palpitations, or shortness of breath.
Class IV. Marked limitation of any physical activity. Symptoms of heart failure appear at rest and worsen with any activity [15].
What pathologies most often affect the function and structure of the LV?
There are many pathological conditions and provoking factors that lead to changes in the anatomical structure and physiological dysfunction of the left ventricle. In some cases, LV hypertrophy is a normal variant, for example, in athletes or pregnant women.
Pathologies that are accompanied by dysfunction of the left ventricle:
- congenital defects: coarctation of the aorta, anomaly of the interventricular septum, combined disorders - tetralogy or pentade of Fallot;
- inflammatory diseases: endo-, myo-, pericarditis (children and adolescents are more often affected);
- acquired heart defects (more often diagnosed in adults as a consequence of rheumatism);
- IHD: angina pectoris, post-infarction cardiosclerosis, necrosis of myocardial walls;
- chronic lung pathology;
- arterial hypertension;
- atherosclerosis of the aorta;
- consequences of metabolic syndrome in combination with obesity and diabetes;
- pathologies of the kidneys, liver, thyroid gland.
Without adequate treatment and hemodynamic correction, the patient’s condition worsens: heart failure progresses, the brain and all internal organs experience oxygen starvation.
At the first manifestations of left ventricular dysfunction, it is recommended to visit a general practitioner (cardiologist) and undergo examinations to prevent further development of the pathology. Patient management depends on the underlying disease and involves the use of pharmacological drugs or cardiac surgery.
Additional therapy includes lifestyle modification and compensation for associated disorders.
Publications in the media
Single ventricle of the heart (SVC) is the absence of a septum between the ventricles of the heart. The main symptom is the communication of both atria through the mitral and tricuspid valves with a common ventricle. The structure of the heart is three-chambered. Frequency : 1.7% of all congenital heart defects (CHD).
Classification • Type A - single right ventricle (no inflow part of the right ventricle) • Type B - single left ventricle (no inflow part of the left ventricle) • Type C - undivided or common ventricle (no interventricular septum) • Type D - anatomy of the EVC is uncertain ( the inflow parts of both ventricles and the interventricular septum are absent).
Hemodynamics. In the single ventricular chamber, mixing of arterial and venous blood occurs. In the aorta and pulmonary artery (PA), which extend directly from the ventricle, the pressure is the same, which leads to the development of pulmonary hypertension.
Clinical picture • Complaints - shortness of breath, tachycardia, frequent respiratory diseases, more pronounced in the absence of PA stenosis • Examination •• Cyanosis, symptoms of “watch glasses” and “drumsticks”, more pronounced in PA stenosis •• “Heart hump” •• Systolic trembling along the left edge of the sternum •• Auscultation - II sound over the PA is accentuated in the absence of its stenosis; systolic murmur in the III–IV intercostal spaces; systolic murmur over the apex of the heart (relative mitral insufficiency); rough systolic murmur over the base of the heart according to the level of stenosis.
Research methods • ECG (deviation of the EOS to the right, hypertrophy of the EVC: the presence of ECG signs of hypertrophy of both the right and left ventricles) • X-ray examination of the chest organs (increase in the diameter of the heart shadow, increased pulmonary pattern) • Cardiac catheterization (high pressure in the EVC cavity, equal to the pressure in the aorta; increased oxygenation of blood in the ventricular cavity compared to the right atrium) • An angiocardiographic study allows you to determine the anatomical structure of the EVC, the location of the great vessels, and identify associated defects • EchoCG helps to identify the absence of an interventricular septum and the presence of two atrioventricular valves that open in EZhS.
Differential diagnosis • Tetralogy of Fallot • Open common AV canal • VSD • Transposition of the great vessels.
TREATMENT
Drug treatment - see Heart failure.
Surgery. Indications: all patients with EWS.
• Palliative operations are performed in young children and patients with the impossibility of radical correction due to many concomitant defects •• Surgical narrowing of the PA is performed with sharply increased pulmonary blood flow and high pulmonary hypertension •• Aortopulmonary anastomosis according to Blalock-Taussig is performed with severe PA stenosis and severe hypoxemia.
• Radical surgery is necessary when there is an increasing deterioration in the patient’s condition due to a progressive increase in the size of the heart and pulmonary vascular resistance. Radical correction is based on the principle of anatomical restoration of the structure of the heart - the creation of a septum dividing the EVC into arterial and venous chambers, and the elimination of associated heart defects. Necessary conditions for a successful operation are a sufficiently large size of the EVC cavity, correctly formed atrioventricular valves, normal location of the great vessels or synistrotransposition of the aorta in relation to the pulmonary trunk. Due to the fact that the implanted septum does not grow with the heart, the optimal age for surgery is 10–13 years. If radical correction is not possible (due to a seated tricuspid valve or due to insufficiency, hypoplasia or atresia of one of the atrioventricular valves) or is associated with a high risk, a hemodynamic Fontan correction is performed (see Tricuspid valve atresia).
Complications • Heart failure • Pulmonary hypertension • Cardiac rhythm disturbances • Postoperative complications (rhythm disturbances; renal failure; partial separation of the patch separating the UVC).
Course and prognosis. The prognosis is unfavorable. In the first year of life, 75% of patients die. The average life expectancy in the natural course of the defect is 6–7 years. Mortality after radical correction is up to 40%, after hemodynamic correction, subject to all Schuss criteria (see Tricuspid valve atresia) - up to 10%. Long-term mortality is 8–10%.
Synonyms • Common ventricle • Three-chamber heart with a single ventricle • Single-ventricle heart • Three-chamber heart with two atria
Abbreviations • EVC - the only ventricle of the heart • PA - pulmonary artery
conclusions
Of all the parts of the heart, the left ventricle plays the greatest role in ensuring adequate blood circulation. The large chamber volume, thick muscular wall and opening into the aorta are key characteristics that determine the importance of the structure. Damage to the left ventricle by ischemic, traumatic, inflammatory processes is accompanied by severe hemodynamic defects with symptoms of heart failure. Shortness of breath, swelling, chest pain, a feeling of interruptions in the functioning of the organ are signs of serious disorders that require comprehensive diagnosis and adequate therapy.
Diagnostics
First of all, you need to contact a therapist or children's doctor (pediatrician), who will listen to your heart rhythm using a stethoscope. It is very easy to hear a heart murmur, so the therapist can easily make a preliminary diagnosis after the first examination.
Next, the patient may be referred for additional diagnostics:
- ECG at rest and after exercise;
- blood pressure measurement;
- Holter monitoring.
Thanks to the examinations carried out, it is possible to accurately determine the presence of a chord, the degree of its danger to health, as well as other diseases (if any).
Modern echocardiography, heart murmurs, pregnant women and diving
Ultrasound machine HS40
Top seller in high class.
21.5″ high-definition monitor, advanced cardio package (Strain+, Stress Echo), expert capabilities for 3D ultrasound in obstetrics and gynecology practice (STIC, Crystal Vue, 5D Follicle), high-density sensors.
Experience in the diagnostic and treatment department allows us to divide patients who come for echocardiography into certain groups, depending on the reasons for their visit.
The first category will be pregnant women
, since an echocardiographic examination is considered mandatory and is included in the examination plan.
The second, numerous category will consist of young people
with cardialgia.
The third group will consist of patients with chronic heart pathology
who need dynamic monitoring (congenital and acquired defects, etc.) or clarification of the diagnosis.
The fourth group will consist of patients with new complaints of pain in the heart area
, shortness of breath, manifestations of heart failure.
This group of patients is the most serious, because among them one can find “acute” pathology (aneurysm of the thoracic ascending aorta, thromboembolism in the pulmonary artery system, development of aneurysm of the left ventricle, etc.). The fifth group will consist of patients with a heart murmur
. We will try to explain the capabilities of echocardiography in the diagnosis of heart pathology and differential diagnosis. To do this, we will try to analyze the above groups of patients.
Echocardiography during pregnancy
During pregnancy, a healthy woman can experience minor changes in the size of the heart cavities and changes in hemodynamics compared to the baseline. Systolic pressure in the pulmonary artery can increase to 40 mmHg. Art. The diameter of the aortic root, left atrium and left ventricle may increase by 2 - 3 mm. The heart rate increases by 25 - 30%, and already in the first trimester of pregnancy the minute volume of blood flow and stroke volume increase. Blood pressure does not change. The degree of valve regurgitation increases (on the tricuspid valve and pulmonary artery valve to degree 3, on the mitral valve to degree 2). In rare cases, a reaction of the pericardial layers can be observed - the presence of a small amount of fluid in the pericardium. The fluid disappears 1 to 3 months after birth in the absence of treatment.
One of the features in pregnant women is dynamic stenosis of the inferior vena cava. This phenomenon may be accompanied by an auscultatory picture - noise during auscultation and syncope that occurs when the body position in space changes. In some cases, during pregnancy, the oval window opens and a slight shunt of blood from left to right is noted. All of the above changes usually disappear after childbirth. Dynamics are best carried out 1 - 3 months after birth.
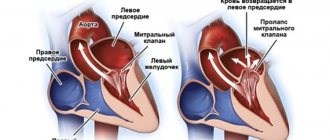
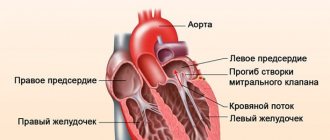
Causes of cardialgia - pain simulating pain in the heart
The most common cause of cardialgia in young people is overwork, stress and hypokalemia (potassium deficiency). Sometimes in this category of patients one can observe a slight prolapse of the anterior leaflet of the mitral valve into the cavity of the left atrium, which is a variant of the hole for young people and children (Fig. 1). This prolapse should not be confused with pathological prolapse when there are organic changes in the valves (for example, with myxomatous degeneration - Fig. 2).
Rice. 1.
Minor prolapse of the anterior leaflet of the mitral valve (normal variant).
Rice. 2.
Myxomatous degeneration of the mitral valve leaflets.
A differential diagnosis can be made at an appointment with a cardiologist or therapist. As a rule, after a conversation with the patient and auscultation, the doctor prescribes an ECG and EchoCG examination. If an electrolyte imbalance is suspected, a biochemical blood test is recommended.
In patients with chronic heart disease
, for example, rheumatic heart disease, congenital heart disease, prosthetic heart valve, etc. Echocardiography is performed once a year or once every 2 years. Echocardiography allows you to assess the condition and structure of the heart valves, the degree of defect, the condition of the prosthesis, the systolic function of the ventricles of the heart, the condition of the aortic walls, the degree of pulmonary hypertension, the condition of the pleural cavities and pericardium, etc. (Fig. 3 and 4). In some cases, patients come to clarify the degree or nature of the defect.
Rice. 3.
Rheumatic heart disease - mitral valve stenosis.
Rice. 4.
Congenital heart disease - atrial septal defect. Dilation of the right chambers of the heart, shunting blood through the defect in color Doppler mode.
Patients with new complaints of pain in the heart area and clinical manifestations of heart failure
are the most serious group of those examined and often require a more detailed examination (for example, coronary angiography) or consultation with a cardiac surgeon or vascular surgeon (Fig. 5).
Rice. 5.
Aneurysm of the ascending aorta.
The causes of heart failure are varied. The echocardiography technique allows for closer verification of the diagnosis, and in some cases, an accurate diagnosis.
Heart murmurs
One of the most common reasons for referral to echocardiography is the presence of a heart murmur.
In the “pre-echocardiographic” era, it was in some cases difficult to distinguish normal functional murmur from pathological one. Let's try to list the causes of the most common normal functional murmurs in the heart area. They are especially good for children, teenagers and thin people.
Additional chord in the cavities of the ventricles (false chord or false chord)
- a filamentous structure located in the cavity of the left or right ventricle. Located between the interventricular septum (IVS) and the wall of the heart, the head of the papillary muscle and the wall, etc. The base of the accessory chord does not thicken during systole. The number of chords may vary. Occurs in 98% of cases (Fig. 6).
Rice. 6.
A minor developmental anomaly is an additional chord in the cavity of the left ventricle (normal variant).
Additional muscle trabecula in the ventricular cavity (false trabecula)
- a muscular structure located in the cavity of the left or right ventricle. Often located parallel to the interventricular septum or transversely between the walls of the ventricle. The base of the accessory muscle trabecula thickens during systole. Occurs in 85% of cases (Fig. 7).
Rice. 7.
A minor developmental anomaly is an additional muscle trabecula in the cavity of the left ventricle and two additional chords (normal variant).
Eustachian valve of the inferior vena cava
- vestigial valve. Does not play any role in cardiac hemodynamics. Occurs in 20% of cases.
Hiari network
- rudiment, continuation of the Eustachian valve of the inferior vena cava into the coronary sinus. Occurs in 2% of cases.
Aneurysm of the interatrial septum
Atrial septal aneurysm (ASA)
- a congenital feature of the development of the interatrial septum. The membrane of the fossa oval is elongated and bulges to the side (Fig. 8). There are a number of types of atrial septal aneurysm:
- type L - bulging of the fossa ovale membrane towards the left atrium.
- type R - bulging towards the right atrium (Fig. 9).
- Type R - L - bulges to the right and then to the left.
- Type L - R - bulging to the left and then to the right - occurs in 5% of cases.
Rice. 8.
Aneurysm of the interatrial septum.
Rice. 9.
Aneurysm of the interatrial septum - type R.
If the aneurysm is very large and protrudes significantly into the atrium cavity, it can be regarded as a congenital defect of the interatrial septum (extremely rare). If there is an atrial septal defect in the area of the atrial septal aneurysm, the situation is regarded as a congenital heart defect.
Aneurysm of the membranous part of the interventricular septum
- rare (0.5 - 1% of cases).
Accessory heads of papillary muscles
- their number can be different and, according to anatomists, can reach 16, the sizes of the heads are also different. The more papillary muscles in the ventricular cavity, the more chordae extend from them.
Non-closure of the oval window
- a variant of the development of the membrane of the fossa oval, occurs in 25% of people. The valve of the fossa ovale membrane covers the oval window. There is no shunting of blood, but it can occur in a number of situations (for example, with a sharp increase in pressure in the cavity of the left or right atrium).
Patent foramen ovale
- occurs less frequently (1 - 2% of people).
Currently, in pediatric practice
there is an overdiagnosis of an open oval window. In this case, blood shunting occurs from left to right, is intermittent, and the volume of the shunt is small. There is no pulmonary hypertension or dilatation of the right chambers. Color Doppler allows you to clarify the presence or absence of an open oval window. These patients require observation once every 2-3 years.
Contraindications for diving
The only contraindication for people with a patent oval window is diving (scuba diving). In any case, whether you are going to Egypt or Thailand and want to plunge into the enchanting world of the seabed, or spend time in the city, do not be lazy to go to a cardiologist and undergo an echocardiographic examination. This will avoid tragic consequences.
Ultrasound machine HS40
Top seller in high class.
21.5″ high-definition monitor, advanced cardio package (Strain+, Stress Echo), expert capabilities for 3D ultrasound in obstetrics and gynecology practice (STIC, Crystal Vue, 5D Follicle), high-density sensors.