Reasons for development
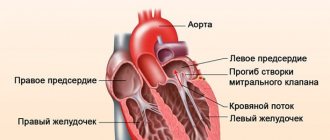
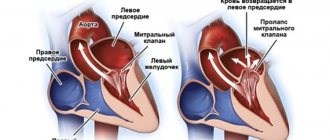
With this pathology, a small part of the blood returns to the atrium, that is, it does not enter the aorta. This condition is often asymptomatic and is usually diagnosed “accidentally” during a routine preventive examination or in connection with examinations for other problems of the cardiovascular system.
In the same way, the causes of prolapse of the anterior valve leaflet are not known for certain; some experts argue that the pathology is associated with hereditary diseases of the connective tissue - for example, it could be osteogenesis imperfecta or Marfan syndrome.
Is it possible to play sports if you have certain contraindications from the heart?
Before sending a child to a sports section, it is necessary to conduct a thorough examination, including a cardiological and medical examination. First you need to do an ECG
with functional tests.
A test with physical activity (20 squats) is carried out in addition to the main ECG to assess the resistance of the cardiovascular system to physical activity and the processes of restoration of its activity after cessation of exercise. At the beginning, the patient's blood pressure is measured and a 12-lead ECG is taken. Then you are asked to stand up and do 20 squats at a calm pace, after which the ECG and blood pressure are re-examined. The pulse is counted before exercise, immediately after exercise and during the recovery period (after 3 minutes). If the increase in heart rate is 35-50% of the original, then the load is low, if the increase is 50-70% - average (optimal), and if the increase is 70-90% - high.
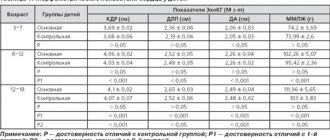
It is also necessary to do an echocardiographic study
to exclude congenital pathology, because
congenital heart defects are a contraindication for the educational and training process and participation in sports competitions at the stages of sportsmanship. The most common congenital heart pathology is atrial septal defect, ventricular septal defect, patent aortic duct, and aortic isthmus stenosis
.
Some anomalies are incompatible with life, others severely manifest themselves in the first hours, days or months of life, with others a person can live to adulthood and even old age. But at the same time, playing sports increases the load on the heart, so these forms of heart pathology are a contraindication for playing sports. To understand how the heart works, you need to know its anatomy.
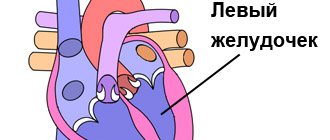
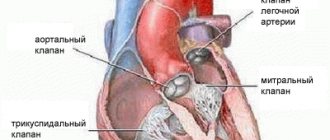
The heart consists of four separate cavities called chambers: left atrium, right atrium, left ventricle, right ventricle.
They are separated by partitions. The atria and ventricles are separated by valves that prevent backflow of blood. The pulmonary artery (pulmonary trunk) emerges from the right ventricle, and the ascending aorta emerges from the left ventricle. The left atrium and left ventricle together form the “arterial heart,” named for the type of blood passing through it; the right ventricle and right atrium combine to form the “venous heart.” The right ventricle and left atrium close the pulmonary circulation, the left ventricle and right atrium close the systemic circulation.
Under the influence of electrical impulses from the sinus node, the heart contracts: first the atrium, and then the ventricle. Blood is pushed into the aorta and spreads throughout the body. At rest, the heart of an untrained person contracts 60-70 times per minute. During exercise, the number of heart beats can increase to 160-220 per minute. After passing through the systemic circulation, the blood returns to the right atrium. At rest, the returned blood is saturated with oxygen up to 75%, and during intense exercise only up to 20%. From the right atrium, blood enters the right ventricle and then into the pulmonary artery. In the lungs, the blood is freed from carbon dioxide and saturated with oxygen. Oxygenated blood is sent to the left atrium, and then to the left ventricle, from which it is pushed into the aorta and distributed throughout the body. The blood supply to the heart occurs during diastole; blood enters it through the artery system. These arteries are called coronary arteries.
This is how a healthy heart works. And if there is, for example, an open oval window, a bicuspid aortic valve, valve prolapse, or other pathology, then the load on the heart increases. During physical work, blood pressure in the chambers of the heart increases and in response to this, the muscle layer gradually thickens. And the more the muscle fibers are stretched, the more intense the compression of the ventricles; the force of contraction of the heart muscle obeys the Frank-Starling law. This stretch cannot be unlimited, and if the increase in fiber length in cardiomyocytes is 35-38%, the myocardium weakens.
All loads can be divided into dynamic and static.
The dynamic type of training involves the development of endurance in runners, skaters, cyclists, and swimmers. Adaptation processes occur in the body: muscle fibers constantly contract and lengthen, blood flow in working muscles increases, peripheral arteries dilate, blood flow in working muscles increases, metabolic reactions with the participation of oxygen accelerate, the rhythm of contractions during exercise increases, the tone of the veins increases, the myocardium stretches under the influence of increased blood flow, the volume of shock ejection increases. Thus, in athletes with a predominance of dynamic (aerobic) exercise, expansion of the cardiac cavities is observed with a minimal degree of myocardial hypertrophy. And if there is a congenital anomaly of the heart, then expansion and hypertrophy will appear faster and more pronounced.
Strength loads do not change the length of muscle fibers, but increase their tone. Tense muscles compress the arteries, and the resistance of their walls increases. With this type of training, the need for oxygen is moderate, but there is no increase in blood flow through the compressed arteries, so tissue nutrition is provided by increasing blood pressure. Constant hypertension during exercise provokes myocardial hypertrophy without expansion of the cavities.
If a child begins to train intensively in preschool age, then due to the incomplete process of formation of the cardiovascular and nervous systems, adaptation reactions are disrupted. This is due to a discrepancy in the growth of internal organs compared to the musculoskeletal system, as well as a hormonal “explosion” in adolescents. It has been proven that after 7-10 months from the start of sports activities in a 5-7 year old child, the thickness of the myocardium and the mass of muscle tissue increase in left ventricle, but its stretching does not occur. In other words, the rudiments of myocardial hypertrophy begin to form already at this time. A rationally structured training process leads to a gradual increase in athletes' fitness. But early specialization in children's sports, a weekly increase in loads by more than 10%, an increase in the duration of the period of intense loads to 3 weeks or more, the inclusion of more than one type of intensive developmental work in one training session, and insufficient recovery between developmental workouts lead to overtraining.
Overtraining causes disruption of long-term adaptations and leads to disruptions in organ function and primary stress-induced damage to the myocardium. Often there is a breakdown of adaptation mechanisms when playing professional sports. A low pulse is accompanied by decreased performance, increased stress is poorly tolerated, sleep is disturbed, appetite decreases, periodic dizziness and darkening of the eyes occur, breathing becomes difficult, pressing pain in the chest appears, and concentration decreases. Therefore, when the pulse rate decreases to less than 40 beats per minute, it is necessary to conduct an examination of the heart and internal organs to identify possible pathological changes. With intense exercise, shortness of breath and a feeling of interruptions, dizziness, and chest pain occur. In heart rhythm disturbances, a significant place is given to the physiological increase in the tone of the parasympathetic nervous system, which is noted during intense sports. Ventricular extrasystole is often detected. Long-term endurance loads can cause the development of atrial fibrillation, attacks of supraventricular and ventricular tachycardia. Increased parasympathetic tone leads to a decrease not only in heart rate, but also in peripheral arterial resistance, so blood pressure in athletes is lower than in untrained peers. If compensatory mechanisms weaken, then changes in hemodynamics are not enough. Deterioration in health may be associated with infection, arrhythmia, allergic reaction, injury, or dehydration.
Taking into account such risks, it should be considered extremely important to periodically monitor the condition of the heart, and if the slightest suspicion of any serious abnormalities appears, conduct a more detailed examination: an ECG, daily monitoring of the ECG and blood pressure, echocardiography, bicycle ergometry, consultation with specialists (otorhinolaryngologist , cardiologist, neurosurgeon). If the child is healthy, then he is allowed to participate in training sessions and competitions in the selected section.
Every year the load on the body increases and the heart also reacts to this process. Enormous physical activity, frequent competitions, and training camps often lead to the appearance of a sports heart.
There are two variants of the sports heart: the physiological sports heart is more efficient, can satisfy the body’s demands when performing larger and longer loads, and the main distinguishing point of the “sports heart” is its most economical functioning at rest and under light loads and activation of the pumping function of the heart when physical activity to a significantly higher level than in untrained people. Pathological sports heart - altered, with reduced performance as a result of stress of a sports nature. The athlete does not feel the transition from a physiological sports heart to a pathological one, he simply becomes less efficient, gets tired easily and almost does not recover during rest. And sometimes it can manifest itself in the form of heart rhythm disturbances, irregular pulse or simply loss of consciousness.
Thus, before sending a child to a sports section, parents need to weigh the pros and cons. Physical activity is good for the heart, but only initially healthy people should engage in professional sports.
S.A. Timoshenko, cardiologist, BU "Clinical Medical and Physical Education Dispensary" branch in the city of Surgut
How does mitral valve prolapse manifest?
Despite the fact that this disease is characterized by an asymptomatic course, some health problems may be a reason for a full examination. Symptoms of grade 1 mitral valve prolapse without regurgitation are especially pronounced:
- periodic pain in the left side of the chest that cannot be relieved with Nitroglycerin;
- the patient constantly tries to take a deep breath, as he does not have enough air, shortness of breath develops;
- constantly present rapid or slow heartbeat;
- regularly occurring fainting and severe dizziness;
- temperature rise to insignificant levels;
- headaches that occur predominantly at night and/or in the morning.
Criteria for suitability for service of a young man with MVP
At first glance, it may seem that mitral valve prolapse and the army are incompatible things. Indeed, this is essentially a heart defect. How can a young man with such a disease be recruited into the army? However, not everything is so simple.
Based solely on the presence of mitral valve prolapse in a person, it is impossible to determine whether he should be admitted to emergency service or not.
I often hear the question: do they enlist in the army with grade 1 mitral valve prolapse? According to the legislation of the Russian Federation, there are the following criteria for the suitability of people with MVP for service:
- mitral valve prolapse of the 1st degree with regurgitation of the 1st degree;
- the conscript has no signs of chronic heart failure or serious heart rhythm disturbances;
- no cases of sudden cardiac death associated with prolapse in close relatives.
Such conscripts are assigned category “A” - fit for military service. They can even serve under a contract.
If there is a MVP with regurgitation of the second degree, the conscript is assigned category “B” - fit with minor restrictions. The young man is sent to a type of military service in which service does not involve performing heavy physical activity - defense of missile combat systems, radio engineering units, etc.
If a person has MVP with grade II regurgitation and functional class I heart failure (this is when symptoms of CHF appear only during very intense and prolonged physical work), he is assigned category “G” - temporarily unfit for military service. The conscript is given a deferment and a referral for cardiac treatment, after which (6-12 months) he again undergoes a military medical commission.
In the case of prolapse with II degree of regurgitation, signs of severe CHF (II-IV functional class), dangerous heart rhythm disturbances, category “B” is established - limited fit for military service. This means that the young man is not subject to conscription in peacetime.
What documents to collect and what examinations to do?
List of documents:
- Passport.
- Medical insurance policy.
- SNILS.
- Registration certificate.
- Outpatient card from the clinic with doctors' notes on the presence of mitral valve prolapse.
- Research protocols (electrocardiography, echocardiography) with conclusions confirming the presence of MVP, severe arrhythmias or heart failure.
It is very important to take with you documents, certificates and medical records confirming the presence of mitral valve prolapse.
General principles of treatment
Once an accurate diagnosis has been established, the cardiologist will select the appropriate treatment tactics. If the pathology occurs without visible symptoms and does not affect the patient’s life, then the specialist will simply monitor his state of health. And treatment of mitral valve prolapse of the 2nd degree with regurgitation can also be carried out surgically - problems with breathing and heart function can cause a lot of inconvenience to the patient. The danger of this particular degree of development of the pathology lies in the fact that the valve at one not entirely perfect moment may either not close or not open - and death is quite likely. True, for such a development of events, several provoking factors must come together - for example, a severe infectious disease, pathologies of the respiratory system, injuries and surgical intervention for any reason.
Surgery for the diagnosis of mitral valve prolapse consists of valve replacement or valve repair. It is performed by cardiac surgeons, is considered a routine procedure and is practically not accompanied by complications.
Prohibited sports that require approval
Despite the absence of strict prohibitions for a number of patients, the disease remains at risk of loss of consciousness and fainting for the following sports disciplines:
- horseback riding;
- diving to a depth of more than a meter;
- motorcycling;
- long swimming, including synchronized swimming.
The following disciplines have a high level of safety from the point of view of cardiology:
- sprint;
- various types of martial arts;
- ball games (volleyball);
- ping pong and other active board games;
- various gymnastics options.
The above-described disciplines are not prohibited even for patients with second-degree prolapse, but before seriously engaging in any of these sports areas, it is necessary to consult with a specialist.
If the patient has a third degree of impairment, then sports may be prohibited until the course of the disease is completely stabilized. Even if the cardiologist makes certain loads acceptable, you must remember that you need to exercise in moderation. It is very important for the patient to monitor his or her health, following medical recommendations and contacting a specialist in case of any deterioration. This will prevent the progression of the disease.
The most popular questions about mitral valve prolapse
Since the pathology in question is rarely diagnosed and is asymptomatic in most cases, people ask many questions:
- Can they join the army with mitral valve prolapse? In most cases, these concepts are quite compatible, but if grades 2 and 3 of the disease are observed, then doctors will conduct a more complete examination and individually determine suitability for military service. It is impossible to give an unambiguous answer to the question posed.
- Is it possible to play sports with mitral valve prolapse? Professional studies will have to be abandoned, and visits to gyms and fitness classes are quite possible, but you must inform your trainer about the diagnosis - he will select the permitted loads, which will not deteriorate your well-being.
- How are pregnancy and the disease in question combined? Gynecologists and cardiologists do not consider this pathology as a contraindication to conception - pregnancy with minor mitral valve prolapse proceeds within normal limits, the disease does not affect the intrauterine development of the unborn child, but the woman will be under the supervision of medical professionals.
- Is it possible for complications to develop if left untreated? Yes, despite its asymptomatic course, mitral valve prolapse can lead to the development of myocarditis, endocarditis (inflammatory diseases of the heart tissue), persistent arrhythmia and mitral insufficiency. Any of these complications requires surgical treatment to replace the valve.
Only specialists can answer all your questions in more detail, and they will also provide information on how to treat primary mitral valve prolapse. You can make an appointment with a doctor on our website Dobrobut.com.
Related services: Cardiac Check-up Diagnosis of heart rhythm disorders by ECG monitoring
Physical restrictions and loads during MVP
A mitral valve defect in itself is not a contraindication to physical activity and sports.
It all depends on the degree of regurgitation, the presence of signs of chronic heart failure (CHF), cardiac arrhythmias, and episodes of loss of consciousness. All people with MVP with stage I regurgitation are prohibited from the following physical exercises:
- boxing;
- sports that require jerking movements - javelin or discus throwing, shot put, wrestling, jumping;
- lifting weights.
Types of sports and physical exercises that are allowed for MVP with I degree of regurgitation:
- Athletics;
- sport swimming;
- exercise in the gym - lifting weights not exceeding your own body weight is recommended. Preference should be given to aerobic exercises (cardio exercises);
- dance training - only those types of dance are allowed that do not involve lifting a partner;
Sports allowed for stage II regurgitation:
- table tennis;
- figure skating (without lifting your partner and sudden jumps);
- swimming (amateur);
- gymnastics;
- a ride on the bicycle.
Any type of sport and physical activity (except physical therapy) is strictly prohibited in the following situations:
- mitral regurgitation degree III;
- pain in the heart area;
- there are serious heart rhythm disturbances: prolonged QT interval, paroxysmal tachycardia, atrial fibrillation, frequent polytopic extrasystoles;
- the presence of signs of congestive heart failure - swelling in the legs, heaviness in the right hypochondrium, difficulty breathing during physical work;
- there were episodes of loss of consciousness (fainting).
For patients with the above symptoms, intense physical activity can sharply worsen their health and cause dangerous complications, which without urgent medical intervention can end very badly.
As for physical therapy (physical therapy), it will be useful for patients with any degree of mitral regurgitation. These exercises are based on increasing endurance and aerobic reserves of both the whole body and the heart.
Examples of exercises:
- high raises of bent legs;
- circular movements of the arms forward and backward;
- circular movements of the hips;
- body turns;
- walking or running slowly.
General recommendations for exercise therapy classes:
- Maintain a moderate pace of movements.
- Breathing should be smooth.
- The duration of one workout should not exceed 30 minutes.
- The total training time per week is about 150 minutes.
- During exercise, you need to monitor your heart rate. It shouldn't be too high. Calculating the limit that cannot be exceeded is quite simple - you need to subtract your age from 200. If the pulse is higher than this value, you should take a short break (1-2 minutes) and continue at a more relaxed pace.