Cardiac hypertrophy is an increase in heart size. This is a heart condition that can lead to serious problems with the structure and functioning of the heart. The heart enlarges due to the fact that cells, cardiomyocytes, proliferate. They make up about 25% of all cells in this organ.
It is known that the heart is a hollow organ consisting of four chambers: the left atrium and ventricle, the right atrium and ventricle. Blood circulates in these chambers. Blood enters the atria and is expelled from the ventricles. In a normal process, the picture will be like this: the pressure in the left side of the heart is always normally higher than in the right chambers. This happens because the chambers of the left side of the heart participate in the systemic circulation, and the right ones participate in the pulmonary circulation.
With heart pathologies, this pattern can change to one degree or another. Doctors note hypertrophy of different parts of the heart chambers, although the incidence of hypertrophy of one or another part of the heart in children varies.
Geneticists are studying the topic of hereditary causes of hypertrophy in children and adults. Previously, it was believed that this disease in patients of different ages was associated with different genetic backgrounds. At this stage, it has been established that mutations can cause hypertrophy in both children and older patients.
of cardiac hypertrophy in children include:
- right ventricular hypertrophy
- left ventricular hypertrophy
- hypertrophy of both atria
- left atrial hypertrophy
- right atrial hypertrophy
Right ventricular hypertrophy
This pathology occurs more often in children than in adults and is associated with an increase and lengthening of muscle fibers as a result of increased functioning. Often the pathology is physiological in nature and is associated with the fact that in the first months of life the load on the parts of the stomach increases. However, more often there is a relationship between hypertrophy and congenital heart defects, which lead to the right ventricle receiving more blood than it can process (with a defect, blood flow may be disrupted). This leads to overload of the right ventricle.
The enlarged myocardium loses its physiological properties. Electrical conductivity is disrupted, which in turn causes arrhythmia, changes in contractility and other disorders.
It should be noted that when hypertrophy of the right ventricle , the vessels associated with it are also negatively affected, which ultimately can lead to their sclerotization and disruption of the functioning of the pulmonary circulation.
The main methods for diagnosing the disease are electrocardiography and echocardiography (ultrasound). The first method may indicate a disturbance in the electrical conductivity of the heart and is considered an indirect method. The second method is more informative. It indicates the exact size of the heart, the presence of stenosis, the location of defects, allows you to estimate the pressure in the chambers, etc. These two methods complement each other, because the diagnosis of right ventricular hypertrophy cannot always be confirmed by ultrasound.
Arrhythmogenic right ventricular dysplasia
Terminology
Arrhythmogenic right ventricular dysplasia (ARVD) is a relatively rare cardiac disease, regarding which many questions and conflicting ideas remain to this day.
The first clinical description belongs to the outstanding Italian thinker, doctor, anatomist Giovanni Maria Lancisi (all other transcriptions of the Italian surname Lancisi, namely “Lancisi”, “Lancisi”, etc., are incorrect). He also wrote avant-garde works for that time (XVII-XVIII centuries) on the neuro-brain organization, on malaria, on the connection between syphilis and vascular aneurysms, and on epizootics in cattle. The date of writing the cardiological study “De Motu Cordis et Aneurysmatibus”, where J.-M. Lancisi described in detail ARVD as a hereditary disease in four generations of one family, domestic sources call it either 1736 or 1745, without any reservations regarding the fact that Lancisi himself died in 1720. In fact, the publication was posthumous and was published in 1728.
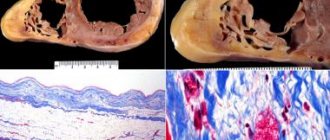
All this may seem unimportant, but there are other ambiguities regarding arrhythmogenic pancreatic dysplasia. The modern formulation of the diagnosis of ARVD was proposed only in 1977, but already five years later (1982) the synonymous diagnosis “arrhythmogenic right ventricular cardiomyopathy” came into use, which is used, in particular, in ICD-10 (heading “Other heart diseases / Cardiomyopathies” ). The disease is usually called hereditary, but often in the same text it is reported that the genetic factor is traced in less than half of the cases. Epidemiological data are incomplete and inaccurate; arrhythmogenic pancreatic cardiomyopathy is classified as a rare disease, but it is the second most common cause of sudden cardiac death at a young age.
The essence of this pathology is that the parenchymal (functional, specialized) tissue of the right cardiac ventricle is gradually replaced by fatty and connective tissue; this steato-fibrous process is usually localized in the “triangle of dysplasia”, the vertices of which are the apex of the heart, the inlet and outlet valves of the ventricle. Statistical estimates of occurrence in the general population vary very widely, with a range of two orders of magnitude: from 0.01% to almost 1% (the latter applies to the Mediterranean region, where ARVD is recorded much more often). Men predominate among those affected - again, some authors limit themselves to this statement, others talk about a threefold predominance. Only one case out of five is diagnosed over the age of 40, the remaining 4/5 occur in children and young people. Sudden cardiac death in 25-26% of people under 20 years of age is caused by arrhythmogenic cardiomyopathy of the pancreas. Similar statistics (25%) are observed in athletes who suddenly died. In total, in the age group under 40 years, ARVD as a direct cause of cardiovascular mortality is detected in 20% of cases. However, it should be emphasized that all these data were obtained from small samples; Of course, they need clarification, and the disease itself needs intensive further research (which is currently being carried out), since until recent decades the clinical and medical-social relevance of this problem, apparently, was seriously underestimated.
Left ventricular hypertrophy
With this pathology, the wall of the ventricle thickens. It happens that the septum between the right and left gastric chambers thickens. The thickening may be uneven, which determines the course of the disease.
This is a fairly common condition among childhood heart diseases with the following pathologies:
- arterial hypertension of the systemic blood circulation
- congenital heart defects
- acquired heart defects
- carditis
- myocardial dystrophies
The characteristic signs of left ventricular hypertrophy are heterogeneous. The patient may not know that he has this disease. Genetics note a high probability of transmission of the disease by inheritance, so a competent doctor studies the family history.
Diagnosis of left ventricular hypertrophy in newborns is quite difficult because they have a predominance of right ventricular mass. In modern pediatrics and cardiology, the diagnosis of left ventricular hypertrophy is highlighted as a separate area of study. The most informative are both electrocardiography (ECG) and echocardiography.
Treatment of this disease can be either surgical or medicinal. During the operation, the septum is brought to its normal physiological state.
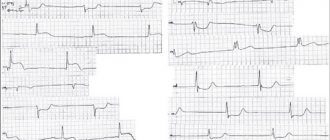
On the issue of ECG diagnosis of right ventricular myocardial infarction
The article draws attention to the importance of diagnosing right ventricular myocardial infarction. ECG diagnosis of right ventricular myocardial infarction is carried out by removing the so-called additional right chest leads V3R-V6R, which reveals pathological Q, ST segment elevation, negative T. The motivation for removing additional right chest leads are both the features of the clinical picture of the disease and mainly, the presence of ECG signs of inferior diaphragmatic or posterobasal myocardial infarction.
To question about ECG diagnosis of myocardial infarction of right ventricle.
The article pay attention to the importance of diagnostics of myocardial infarction of the right ventricle. ECG diagnosis of myocardial infarction of the right ventricle is carried out when removing the so-called additional right precordial leads V3R-V6R, in this case show pathological Q, rise segment ST, negative T. The motivation for the withdrawal of additional right precordial leads are both features of clinical disease and, mainly, the presence of ECG-signs inferior phrenic or posterobasal myocardial infarction.
Recognition of right ventricular myocardial infarction in widespread practice is casuistic. At the same time, its frequency is about 3%. A large number of patients have simultaneously myocardial infarction of the left and right ventricles, while right ventricular myocardial infarction is especially common in patients with damage to the lower wall of the left ventricle (up to 30% of patients). 13% of patients have a combination of myocardial infarction of the right ventricle and the anterior wall of the left ventricle. At autopsy, combined lesions of both ventricles are detected in 14-84% of the deceased (N.A. Mazur, 2009). Unfortunately (in terms of diagnosis), in patients with right ventricular myocardial infarction there are no clear specific differences in the clinical manifestations of the disease. ON THE. Mazur (2009) notes that some patients experience rapid development of right ventricular failure without stagnation of blood in the pulmonary circulation. At the same time, A.V. Shpector and E.Yu. Vasilyeva (2008) draw attention to the fact that in the acute stage of right ventricular infarction, right ventricular failure is usually manifested not by stagnation of blood in the systemic circulation, which develops later as fluid accumulates, but by hypotension. This is due to the fact that a feature of the mechanics of the right ventricle is its high dependence on preload. And therefore, if a patient with signs of right ventricular myocardial infarction has reduced blood pressure, he needs massive infusion therapy. At the same time, vasopressors are dangerous because, by increasing systemic pressure, they increase the pressure in the vessels of the pulmonary circulation, which sharply increases the load on the affected right ventricle. The volume of required infusion for hypotension associated with right ventricular myocardial infarction often reaches several liters. This is quite safe if there is an isolated lesion of the right ventricle, because with a healthy left ventricle, pulmonary edema does not develop. However, if there is combined damage to both ventricles, then the infusion must be carried out under the control of wedge pressure in the pulmonary artery to avoid overload of the pulmonary circulation. Due to the increased sensitivity of the right ventricle to preload, another feature of the treatment of right ventricular myocardial infarction is extreme caution in the use of nitrates and diuretics (as they reduce preload). Caution is also necessary in the use of morphine in such patients, because morphine has a moderate vasodilating effect.
Is it necessary to use thrombolytics for right ventricular myocardial infarction? No special studies have been conducted on this issue, but there is expert agreement on the advisability of their use, especially in the case of hypotension; Angioplasty is also indicated for patients with right ventricular myocardial infarction. It should be noted that the occurrence of atrial fibrillation in patients with right ventricular myocardial infarction leads to rapid deterioration of the condition; in such cases, urgent electrical cardioversion is necessary.
How is right ventricular myocardial infarction diagnosed in routine clinical practice using an ECG?
It is known that the right coronary artery is the common source of blood supply to both the posterior parts of the left ventricle and the right ventricle. Therefore, up to 1/3 of posterior left ventricular myocardial infarction is combined with right ventricular myocardial infarction. With the extreme right type of coronary circulation, the branches of the right coronary artery can extend to the lateral wall of the left ventricle and to the apex. A.V. Shpector and E.Yu. Vasilyeva (2009) note that 75% of patients with myocardial infarction have multiple lesions of the coronary arteries, which often leads to the development of collateral circulation. At this stage, the extent of myocardial infarction may not correspond to the classical anatomy of the coronary bed. Thus, if the patient had subtotal stenosis of the anterior interventricular artery and the blood supply to its zone was provided largely by collaterals from the right coronary artery, then thrombosis of the right coronary artery can lead to the development of a huge circular myocardial infarction.
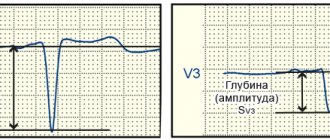
Right ventricular myocardial infarction is diagnosed on the ECG using additional ECG leads - the so-called right chest leads: V3R-V4R-V5R-V6R. These leads must be removed in all cases of posterodiaphragmatic and posterobasal myocardial infarction, as well as when the localization of myocardial infarction according to standard ECG leads is unclear (Candell - Riera J. et al., 1981; Wenger N. et al., 1981; Goldberger A., 1984 ; Wagner G., 1994; Shevchenko N.M., 1994; Doshchitsin V.L., 1999; Mazur N.A., 2009). Registration of V3R-V6R or at least V4R in the first hours of the disease is very important for recognizing right ventricular myocardial infarction (N.A. Mazur, 2009).
In order to remove additional right chest leads, the active electrode is applied to the right half of the chest “mirror”, symmetrically with respect to the traditional chest leads (Fig. 1). In this case, electrodes V1-2 are left unchanged, and electrodes V3-6, transferred to the right half of the chest, form the right chest leads.
Figure 1. Additional right chest leads
a - diagram of the application of additional right chest leads
b — application of chest electrodes on the patient
c - ECG taken with left chest leads and additional right chest leads in a practically healthy person
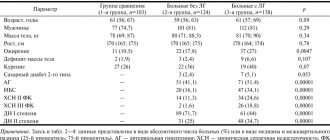
In case of myocardial infarction of the right ventricle, the following changes are detected in the right precordial leads:
1) the presence of ST segment elevation of 0.5-1 mm in these leads is highly specific (however, ST segment elevation in half of the patients persists for no more than 10 hours from the onset of the disease);
2) pathological Q wave; the QRS complex has the form QR or QS (V.L. Doshchitsin, 1999). ON THE. Mazur (2009) notes that pathological Q in the right precordial leads has low specificity;
3) negative T wave;
4) in the case of necrosis of the lateral and anterior walls of the right ventricle, the same changes are recorded when electrodes V3R-V4R-V5R-V6R are applied two ribs above (Lyusov V.A. et al., 2008).
In addition, ST segment depression in leads V2 and aVF has a high predictive accuracy (about 80%); Right bundle branch block and atrioventricular block often occur.
We observed patient Sh., 70 years old, in the 11th city hospital of Kazan with extensive circular myocardial infarction, when an ECG during the first day of hospitalization initially revealed an elevation of the ST segment by 3 mm in leads V1-V4, depression of the ST segment in I, aVL, then a complete block of the right bundle branch developed, and then ST segment elevation occurred in III and aVF. ECG signs of inferior myocardial infarction (ST segment elevation in III and aVF) prompted us to take the right precordial ECG leads. When removing the right chest leads, pathological Q, ST segment elevation and negative T in V3R-V6R were detected, which indicates the development of myocardial infarction in the right ventricle as well.
We present an ECG of patient Sh., 70 years old (Fig. 2).
Figure 2. ECG of patient Sh., 70 years old.
Extensive circular myocardial infarction with a Q wave: myocardial infarction with a Q wave of the anteroseptal region of the left ventricle spreading to the apex and lateral wall of the left ventricle, myocardial infarction with a Q wave of the inferior wall of the left ventricle and right ventricle; complete right bundle branch block
Subsequent selective coronary angiography (at the Moscow Clinical Clinical Center) revealed a right coronary type of coronary circulation. The details of the angiographic study are as follows: left coronary artery - trunk without features, LAD - occlusion in the middle segment, distal LAD is not contrasted, subocclusion of the 1st arterial artery in the proximal section, OB - stenosis of the high-outgoing 1st arterial artery in the proximal segment up to 50%, stenosis of the left artery in the middle segment up to 75%. Right coronary artery - stenosis in the middle segment up to 50%, stenosis of the RV ostium up to 90%, WMA - stenosis in the middle segment up to 90% and 80%. ZMZhV - occlusion in the proximal part, the distal parts are contrasted by intrasystemic anastomoses.
So, with this message we want to draw attention to the issue of ECG diagnosis of right ventricular myocardial infarction. In routine clinical practice, with ECG signs of myocardial infarction of posterior localization, it is necessary to take an ECG in additional right chest leads V3R-V6R, which makes it possible to diagnose right ventricular myocardial infarction when a pathological Q wave, ST segment elevation and a negative T wave are detected in these leads. right ventricular myocardial infarction makes a significant correction in the management of patients with myocardial infarction.
V.N. Oslopov, O.V. Bogoyavlenskaya, Yu.V. Oslopova, M.A. Makarov, R.T. Khabibullina, M.G. Tregubova
Kazan State Medical University
City Clinical Hospital No. 11 UZ Kazan
Bogoyavlenskaya Olga Vladimirovna - Candidate of Medical Sciences, Associate Professor of the Department of Propaedeutics of Internal Diseases
Literature:
1. Mazur N.A. Practical cardiology. - M.: Medpraktika-M, 2009. - 616 p.
2. Shpector A.V., Vasilyeva E.Yu. Cardiology: clinical lectures. - M.: AST: Astrel, 2008. - 765 p.
3. Candell-Riera J., Figueras J., Valie V. et al. Right ventricular infarction. Relationships between ST segment elevation in V4R and hemodynamic, scintigraphic and echocardiographic findings in patients with acute inferior myocardial infarction. - Am. Heart J., 1981. - V. 101. - P. 281.
4. Wenger NK, Mock MB, Ringqvist I. Ambulatory electrocardiographic recording. — Chicago: Year Book Med. Publ., 1981. - 456 p.
5. Goldberger AL Myocardial infarction. Electrocardiographic differential diagnosis: 3rd ed. —St. Louis: Mosby, 1984. - 336 p.
6. Wagner GS Marriot's practical electrocardiography. 9th ed. - Baltimore: Williams & Wilkins, 1994. - 434 p.
7. Shevchenko N.M. Fundamentals of clinical electrocardiography. Qualification tests for ECG interpretation. - M.: Overley, 1994. - 156 p.
8. Doshchitsin V.L. Clinical electrocardiography. - M.: Medical Information Agency, 1999. - 373 p.
9. Lyusov V.A., Volkov N.A., Gordeev I.G. Myocardial infarction. In the book: Guide to Cardiology: Textbook in 3 volumes / ed. G.I. Storozhakova, A.A. Gorbachenkova. - M.: GEOTAR-Media, 2008. - T. 1 - P. 514-515.
Atrial hypertrophy
A relatively common pathology in children. It is observed in the case of simultaneous violation of the mitral valve and tricuspid valve, with other heart defects that are congenital in nature, as well as with an atrial septal defect. Also, hypertrophy of both atria occurs as a concomitant disorder with carditis.
Doctors note that diagnosing biatrial enlargement (atrial hypertrophy) is more difficult than with isolated atrial defects. As with other types of hypertrophy, the main diagnostic methods are ECG and ultrasound of the heart.
Ventricular myocardial hypertrophy
the myocardium of both ventricles working without disturbances and the synchronous contractility of both chambers. But when the physiologically normal functioning of the cardiac system is disrupted, creating obstacles or changes in the direction of blood flow, it leads to intensive work. As a result of greater load, cardiac hypertrophy , which is combined with simultaneous changes in the myocardium itself. Conductivity and metabolism deteriorate.
The disease is quite common in young children. But diagnosing it, especially in early childhood, is quite difficult. Compared to diagnosing atrial hypertrophy, identifying ventricular myocardial disorders is considered a more difficult task, since it is more difficult to detect asynchrony in the work of the right and left sections.
Atrial hypertrophy
Left atrial hypertrophy occurs in children with the following diseases:
- congenital heart defects (mitral valve insufficiency, left ventricular hypoplasia, transposition of blood vessels, etc.)
- acquired heart defects (mitral valve stenosis and insufficiency, etc.)
- hypertension
- atrial tumors, myocarditis, cardiomyopathy
- mitral valve prolapse
Right atrium hypertrophy , compared with left atrium pathology, is much less common in pediatric patients. The process of enlargement of the right atrium is given rise to diseases such as:
- congenital heart defects (tetralogy of Fallot, Eisenmenger disease, pathology of the interatrial septum and others)
- cor pulmonale
- tricuspid malformations
In conclusion, it should be noted that depending on the degree of pathology and its types, the doctor prescribes either conservative treatment or insists on the need for surgery.
leave a comment
Specifics and classification of the violation
The shape and size of the heart are individual and depend on body type, lifestyle, gender, and age. This is a muscular organ that has four chambers - 2 ventricles and 2 atria. The wall has a three-layer structure - the endothelial layer, the myocardium, and the connective tissue layer.
The myocardium is a layer of highly specialized striated muscle tissue, densely saturated with capillaries and nerve fibers. Heart cells are not capable of simple division; they increase in volume due to the accumulation of various substances in the cytoplasm.
Structure of the heart wall
Cardiomyocytes contain a large number of contractile proteins - troponins, myosin, tropomyosin and others. If their synthesis is disrupted, the structure and arrangement of fibers is disrupted, and functions are reduced.
There are several classifications of cardiac hypertrophy. By form:
- Asymmetrical - uneven thickening of the wall of one or more cavities, for example, the apex, interventricular septum, hypertrophy of the anterior or posterior wall of one of the ventricles, atrial hypertrophy.
- Symmetrical - equal thickening of the muscle layer in all sections.
By time of occurrence:
- Acquired.
- Congenital.
Thickening of the wall of the left ventricle
Concentric and eccentric hypertrophy are also distinguished. In the first case, the ratio of the thickness of the walls of the heart cavities and their volume is disrupted. In the second form, a more pronounced expansion of the cardiac chambers occurs with a slight increase in the muscle layer.
Depending on the blood flow disturbances, obstructive and non-obstructive forms are distinguished. There is also a classification based on myocardial thickness. Normally, this indicator during echocardioscopy is no more than 15 mm. With a moderate degree, the wall thickens up to 20 mm, average 20-25 mm, severe hypertrophy - more than 25 mm.
Based on the characteristics of the clinical course, several stages of development of myocardial hypertrophy are distinguished:
Compensated. The person has no active complaints, no blood flow disturbances are observed.- Subcompensated. Complaints appear when walking quickly, performance decreases, pressure in the cavity of the left ventricle rises to 36 mm Hg.
- Decompensated. There is a feeling of shortness of breath, lack of air, nagging pain behind the sternum when performing the usual work. LV pressure is 37-44.
- Expressed. Life-threatening condition, pronounced symptoms even when walking. The pressure in the heart cavity rises above 75.
Causes and symptoms of damage to different parts of the heart
Myocardial hypertrophy is caused by many reasons and is manifested by a variety of symptoms, often has a genetic predisposition or occurs secondary.
Left ventricle
This is the largest chamber of the heart; blood is ejected from it into the aorta to ensure the functioning of all internal organs. With hypertension, stenosis of the four-leaf valve, obesity, and physical activity, energy costs for muscle contraction increase, since greater pressure must be overcome.
If the tricuspid valve, located between the left atrium and the ventricle, is insufficient, during the period of relaxation of the heart, the ventricle is overloaded with a large amount of blood.
Departments of the heart
The organ begins to compensate for its function by increasing the muscle layer. Also, increased work of this muscle is necessary during stress, emotional instability, and insufficient rest because the number of heart contractions increases, and accordingly, more energy is expended.
The main symptom is the appearance of pain behind the sternum during physical and emotional stress, of a pressing or squeezing nature. This symptom is based on insufficient oxygen supply to cardiomyocytes, caused by narrowing of the capillaries during contraction of the thickened muscle.
Quite often, arrhythmia is a manifestation of left ventricular hypertrophy. A person feels a sinking heart, which is then replaced by a frequent and increased heartbeat.
This condition is accompanied by dizziness and darkening of the eyes due to insufficient blood flow to the brain. Other symptoms include shortness of breath, increased blood pressure, and disturbances in the general condition of the body.
Left atrium
Left atrial hypertrophy can occur either as a result of progression of left ventricular failure or as an independent pathology. The most common causes are hypertension and obesity.
With mitral valve stenosis, large amounts of energy are required to fill the left ventricle. With tricuspid valve insufficiency, part of the blood is thrown back into the atrium during contraction. The residual volume of blood is retained in the atrium, and the load increases accordingly.
Enlargement of the walls of the left atrium on the ECG
For quite a long time, the pathological process may not be accompanied by clinical symptoms; the heart uses compensation mechanisms. One of the main complaints with LA hypertrophy is shortness of breath.
In the initial stages, it occurs during intense physical activity and quickly goes away with rest. Then it can be complicated by cough, hemoptysis, and attacks of suffocation. Angina pectoris and arrhythmias almost always occur. All these manifestations significantly reduce the quality of life.
Right ventricle
Right ventricular hypertrophy is always a pathology and very often occurs as a manifestation of other disorders of the cardiovascular system. It is quite rare in the general population; it is more often congenital and occurs in children.
The most common cause is congenital defects (tetralogy of Fallot, ventricular septal defect, mitral valve stenosis), lesions of the valve apparatus due to infectious, autoimmune diseases (systemic lupus erythematosus, rheumatism).
Also, an increase in the right side of the heart is observed with:
hypertension of the pulmonary circulation;- chronic obstructive bronchitis;
- bronchial asthma;
- pulmonary form of cystic fibrosis;
- pneumosclerosis;
- emphysema;
- tuberculosis.
There are usually no pronounced complaints. Swelling of the lower extremities, shortness of breath, and cough may occur. Pancreatic hypertrophy is most often diagnosed accidentally.
Right atrium
Right atrial hypertrophy is always a symptom of pre-existing disorders. Most often it occurs with increased pressure in the pulmonary vessels, with hypertension, congenital heart defects, and chronic diseases of the respiratory system. Symptoms are nonspecific.
Diagnostics
It is impossible to make such a diagnosis on your own. Diagnosis of hypertrophic changes in the heart includes several stages. At the initial appointment, the doctor, using objective research methods, can predict the disease.
Using percussion (tapping with fingers on the anterior chest wall), he determines the shape and size of the heart, assesses their compliance with age and physique. On palpation, he may feel an increased heartbeat between the ribs. Auscultation can detect various noises and increased heart sounds.