Open common atrioventricular canal
Anatomically, this defect is the absence of a section of septa separating the right and left atria in their lower section, and the ventricles in their upper section. Instead of the normal fusion of the interatrial and interventricular septa, a large common opening is formed between all four chambers of the heart. The matter is further complicated by the fact that this is where the zone of attachment to the septum of the atrioventricular valves is located: in the left - the mitral valve, in the right - the tricuspid. nowhere to attach themselves
, and they fuse with each other, forming
valves common to both ventricles
.
Above them there remains a defect between the atria, and below them there is a defect between the ventricles. “full form”
occurs .
If the leaflets adhere to the interventricular septum, then there will be no interventricular defect underneath them. Only interatrial communication remains. Then they talk about “incomplete form”,
or primary atrial septal defect. It’s very simple to imagine this - draw a cross, and then erase the area where the vertical and horizontal lines connect. The vertical line is the interatrial (top) and interventricular (bottom) septa, the horizontal line is the valves, and the dotted line is their common valves: This is the full form. Now connect two horizontal lines with the bottom vertical - you get the letter "Y" with only one hole at the top - this is an incomplete form of the vice.
Unlike ventricular septal defects, the VVC will never close on its own.
Let's talk first about the incomplete form of the vice. It is called a primary atrial septal defect because it is only a large defect in the lower part of the atrial septum. But it is accompanied by another intracardiac disorder - “splitting
» the anterior leaflet of the mitral valve, the two halves of which do not fuse together (and a gap forms between them).
Mitral valve insufficiency
occurs , i.e. With each contraction, through this splitting, part of the blood from the left ventricle is thrown back into the left atrium. That is, in addition to the atrial septal defect, another reason appears that increases the residual blood volume in the cavities of the heart and the load on all its parts.
Complaints and clinical symptoms are very similar to those described for isolated atrial septal defects, but they develop earlier and at a faster rate. Usually, at the age of the first 3-6 months of life, there are already direct indications for surgery. Some patients come to surgeons as adults, but the likelihood that they will suffer from rhythm disturbances even after the defect is completely eliminated is quite high.
The essence of the operation is to close the defect using a patch (usually from the pericardium, i.e. the dense sac surrounding the heart) and suturing the split mitral valve leaflet. It is clear that this is an open-heart intervention with the help of artificial circulation. The operation is well developed and its risk is the same as when closing a conventional interatrial communication, i.e. practically insignificant.
With the full form of the vice
the situation is more complicated. There are several components: an atrial septal defect and a ventricular septal defect, merging into one huge hole, and one valve ring common to both ventricles, regulated by two large common leaflets. All parts of the heart work under enormous overload, constantly increasing the volume of blood. The small circle is especially crowded. The pressure in it naturally increases and, as with large VSDs, the danger of rapid development of irreversible changes in the pulmonary vessels is very high.
Clinically, the defect is severe. Symptoms of heart failure appear already in the first months of life, and the child’s condition requires constant drug support. The heart quickly increases in size - all four chambers are overloaded and have difficulty coping with the work. The child is very sick, eats and develops poorly, and constantly catches colds, often ending in pneumonia. The condition is not critical, but very dangerous. Surgery required
soon after a definitive diagnosis.
If there are conditions for surgical treatment, the defect can be eliminated simultaneously in the first months of life, and if there are no such conditions, treatment can be divided into two stages, i.e. First, narrow the pulmonary artery (as with VSD), and after a few months perform radical surgery.
The essence of correcting the defect is this. In an open-heart setting, the common valve leaflets are bisected to create two separate entrances to the right and left ventricles. The ventricular septal defect is then closed using a patch. The previously dissected parts of the common leaflets are sewn to this patch, thereby creating the right and left atrioventricular openings. Then, a separate patch is used to close the interatrial part of the former defect.
There is a lot of work here, and it takes quite a long time both for the operation itself and for using the heart-lung machine. At the same time, the capabilities of leading clinics specializing in the surgical treatment of defects in infants make it possible to perform this operation in infancy. Operations in the early stages are absolutely justified, because allow you to avoid many complications that are already difficult or impossible to correct. Today the operation is quite well developed and standard, and its results are good.
However... This is an eternal “however” in medicine... When a surgeon works on valve flaps, which, especially in small children, are the thinnest transparent petals, then any, even the thinnest material for sutures turns out to be too rough. In addition, the baby will grow, and the heart - and its valve openings - will enlarge as it grows. Therefore, the earlier the operation is performed, the more likely it is that someday his atrioventricular valves, especially the mitral valve, will work imperfectly, i.e. their insufficiency will appear. This can happen even after a perfectly performed first operation. At some point in adolescence or adulthood, the question may be raised about eliminating the insufficiency surgically: plastic surgery or valve replacement. But this, if it happens, will be much later. Here we want to emphasize that a child who has been successfully operated on for a full form of VVC should be regularly shown to a cardiologist and monitored the function of his valves, which may change over the years.
This does not mean at all that you need to protect your child from physical activity and convince him that he has a heart condition, under no circumstances. But he probably still shouldn’t engage in, for example, high-impact sports, which today involves stress beyond the limits of a healthy person’s capabilities. However, monitoring him by a competent pediatric cardiologist is the guarantee that everything will be done on time.
It should be added that, in contrast to previously described operations for patent ductus arteriosus, ventricular or atrial septal defect, coarctation, and incomplete AVK, surgery for complete AVK, especially in young children, is a particularly delicate and complex procedure that requires excellent preparation the entire surgical team and sufficient experience. Not long ago, it was associated with significant mortality even in the best specialized centers. Today this is not the case, and the results, both immediate and long-term, are excellent.
One of the founders of cardiac surgery, Dr. John Kirklin, once said: “In my opinion, this is the most beautiful operation that is performed for congenital heart defects.” And may she be not only the most beautiful for your child, but also the most successful.
How to get treatment at the Scientific Center named after. A.N. Bakuleva?
Online consultations
Publications in the media
Patent atrioventricular canal (AVC) is a group of congenital anomalies characterized by the presence of fused VSD and atrial septal defect (ASD) and impaired development of the AV valve apparatus. Statistical data • 5% of all congenital heart disease under the age of 1 year • 2–6% of all congenital heart disease, of which 70% are partially open AVK, 30% are complete and intermediate forms of open AVK • 25–30% are combined with Down syndrome.
Etiology: causes of congenital heart disease (see Tetralogy of Fallot).
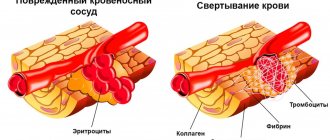
Pathogenesis. The full form (common OAVC) is characterized by a primary ASD merging with a defect in the membranous part of the interventricular septum, and a highly located VSD; the AV valves have common leaflets for the left and right atrioventricular orifices. Partially open AVK is a combination of a primary ASD with splitting of the anterior mitral leaflet and/or tricuspid valve leaflet. Intermediate forms (oblique canals, or Gerbode defects) are characterized by blood flow from the left ventricle to the right atrium, which leads to overload of the right ventricle and dilation of the pulmonary artery trunk. Hemodynamic disorders consist of a combination of those with VSD and ASD (see Ventricular septal defect, Atrial septal defect).
Clinical picture
• Complaints: see Atrial septal defect, Mitral valve insufficiency.
• Objectively • Pallor of the skin •• Severe cyanosis in children over 4 years of age with the full form of open AVK •• The borders of the heart are expanded to the left and right •• Increased apical impulse •• Right ventricular impulse •• Systolic tremor •• Strengthening of the first sound above the apex of the heart and II tone above the pulmonary artery (with a partially open AVK absent) •• Pansystolic murmur over the entire region of the heart with a maximum in the third and/or fourth intercostal spaces, carried out in the interscapular and axillary region (with complete and intermediate forms) •• For incomplete forms Characteristic is a systolic murmur in the second intercostal space on the left (the murmur of an ASD) in combination with the murmur of mitral regurgitation at the apex of the heart.
Instrumental diagnostics • ECG : see Ventricular septal defect, Atrial septal defect, Mitral valve insufficiency • EchoCG: see Ventricular septal defect, Atrial septal defect, Mitral valve insufficiency • Chest X-ray: see Ventricular septal defect, Atrial septal defect partitions, Mitral valve insufficiency • Catheterization of the cardiac cavities: see Ventricular septal defect, Atrial septal defect, Mitral valve insufficiency • Left and right atriography and ventriculography, coronary angiography: see Ventricular septal defect, Atrial septal defect, Mitral valve insufficiency.
Drug treatment: prevention of infective endocarditis and treatment of heart failure.
Surgical treatment • Indications •• At an early age - variants of the defect refractory to conservative treatment, accompanied by clinical symptoms •• General open VVC •• At preschool age - open VVC, regardless of the presence of clinical symptoms (due to the high risk of infective endocarditis and the high frequency progression of heart failure at school age) • Contraindications: see Atrial septal defect • Methods of surgical treatment •• In case of incompletely open VVC - mitral valve plastic, ASD plastic with a patch of autopericardium or synthetic material •• If emergency correction of a general open VVC is necessary in children with body weight less than 3 kg, concomitant heart defects and with little clinical experience in radical correction of the defect at an early age - narrowing of the pulmonary trunk •• In other cases - simultaneous plastic surgery of VSD, ASD, mitral and tricuspid valves •• For intermediate forms of open AVK - plastic surgery VSD, if necessary, tricuspid valve annuloplasty.
Specific postoperative complications • Inadequate correction of the defect (most often mitral regurgitation) • AV block • Infective endocarditis.
Prognosis • Severe forms manifest themselves in the first months of life, with mild forms the general condition is not affected • Average life expectancy - 15 years • With incompletely open VKA, average life expectancy of non-operated patients - 20 years • Surgical mortality - less than 6.7% • In general open VVC and the natural course of the defect, 95% of patients die by the age of 5 • Postoperative mortality - up to 32% • Patients with intermediate forms of open VVC have a relatively favorable prognosis, but all require surgical treatment.
Synonyms: Defects of endocardial ridges; Atrioventricular communication; Persistent common atrioventricular orifice.
Abbreviations. AVK - atrioventricular canal.
ICD-10. Q21.2 Atrioventricular septal defect