CRP – indications for examination
CRP is assigned:
- if the patient is at risk of a bacterial infection;
- For patients recovering from surgery, if CRP values remain elevated three days after surgery, a bacterial infection may be suspected;
- newborns with signs of infection;
- patients with signs of sepsis: fever, chills, rapid breathing and palpitations;
- when a health condition needs to be assessed, such as lupus or arthritis;
- to check the effectiveness of inflammation therapy - during it, the level of CRP should decrease;
- to study body damage and consequences after operations, organ transplants and burns, for early detection of possible infection.
The CRP test can help with:
- assessing the severity of the inflammatory process;
- early detection of postoperative complications;
- detection of transplant rejection;
- monitoring the success of antibiotic treatment for bacterial infections;
- monitoring patients with inflammatory rheumatic diseases.
Thus, the most common use of the CRP test is to determine its level when inflammation caused by a bacterial infection is suspected.
This is especially useful for distinguishing viral from bacterial infections. Since in viral infections - inflammations accompanied by increased sedimentation and an increase in the number of leukocytes, the level of CRP remains in a lower range than in the case of a bacterial infection. And in this case his growth is much higher.
An increase in CRP is present in the following cases:
- with inflammation;
- after operation;
- in the presence of malignant diseases;
- for allergic reactions;
- for chronic inflammatory diseases such as rheumatoid arthritis or lupus.
Complexes with this research
Male check-up No. 1 39 studies for annual preventive examination 12,740 RUR Composition
Inflammation of the joints Risk indicator for developing systemic manifestations of rheumatoid arthritis 510 RUR Composition
For those at risk of COVID-19 Diagnosis of diseases complicating the course of coronavirus infection RUR 2,880 Composition
IN OTHER COMPLEXES
- Advanced male anti-aging diagnostics RUB 25,030
- Nutritionist recommends RUB 4,930
- Women's anti-aging diagnostics RUR 8,130
- Anti-aging diagnostics in postmenopause RUR 8,510
- Male anti-aging diagnostics RUB 9,090
High CRP and disease diagnosis
During an acute inflammatory reaction, the concentration of CRP increases many times over. It begins to grow 6 to 9 hours after the onset of inflammation and reaches a maximum after 48 hours. Protein returns to baseline levels within 7 to 10 days after stopping treatment.
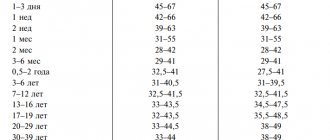
| SPB level | Meaning | What does it indicate? |
| <5 mg/l | Normal | No inflammation |
| 0-40 mg/l | Slightly elevated | Mild inflammation |
| 40-200 mg/l | Increased | Acute inflammation |
| 200 and above mg/l | High | Severe bacterial infection |
Testing the concentration of C-reactive protein often reveals problems in the proper functioning of the body at an early stage before symptoms appear.
| Type of infection | SPB level |
| Gram-negative bacteria – Escherichia coli, Salmonella, Helicobacter pylori and others | 500 mg/l or more |
| Gram-positive bacteria – staphylococci, streptococci, tuberculosis or parasites | up to 100 mg/l |
| Viruses | up to 50 mg/l |
Results above 50 mg/L are a sign of serious infection, injury, or chronic disease, which will require additional testing to determine the cause.
In such situations, rapid identification of the bacterial pathogen is especially important to determine targeted antibiotic therapy.
SRP and antibacterial therapy: a paradigm shift?
The COVID-19 pandemic has forced the international community to reconsider recommendations for the diagnosis and management of respiratory infections. For example, the recommendations of the UK National Institute of Health [20] for primary care physicians on the management of patients with community-acquired pneumonia previously suggested determining the level of CRP for symptoms of lower respiratory tract infection, if after a clinical study the diagnosis of pneumonia was not established and it was unclear whether to prescribe an antibiotic to the patient or not. An antibiotic should not be prescribed if the CRP level was less than 20 mg/L, if the CRP level was 20–100 mg/L, a delayed antibiotic was recommended (a prescription was given for a subsequent antibiotic if symptoms worsened), and if the CRP level was above 100 mg/L, a antibiotic. During the COVID-19 pandemic, this guidance was withdrawn and is currently being revised [20]. The Russian medical community is also expecting updated recommendations, some of them have already been published in the form of drafts [8], others are under revision. Further studies will show whether, in the long term, the doctor's decision to prescribe antibiotic therapy for respiratory infection will depend on the results of the rapid test for CRP [2, 4, 21]. The introduction of such tests into the routine practice of primary care physicians should be considered in the context of initiatives for the rational use of antibiotic therapy.
The primary care physician also faces the question of which inflammatory biomarker is best to use and whether it is advisable to prescribe several tests simultaneously. In 2021, the results of a prospective cohort study of nearly 137,000 outpatients [22] who underwent biomarker testing (including CRP or ESR, or both) for various conditions (including infections) were published. CRP testing has been shown to have greater diagnostic accuracy for infections than ESR testing, and using both tests simultaneously only marginally increases diagnostic accuracy (which is clinically controversial and economically irrational). The authors suggested that CRP levels should be used as a first-line test in most cases (infections, autoimmune conditions, cancer).
What can a CRP test show?
C-reactive protein manifests itself as a protective reaction of the body. Its function is to participate in the immune response, which consists in inactivating the inflammatory factor and stimulating the function of immune cells.
Quantitative CRP testing has less diagnostic value in the case of chronic inflammatory diseases such as rheumatic diseases, since the CRP value can vary from 10 to 1000 mg/L. However, diagnostically important is the fact that the level of CRP is associated with the degree and activity of the inflammatory process. Monitoring changes in the concentration of C-reactive protein - decrease or increase - informs about the stage of inflammation, its extinction or failure of therapy.
Before taking a CRP test, it is recommended that you consult with your doctor in advance to discuss any medical conditions that may affect the results.
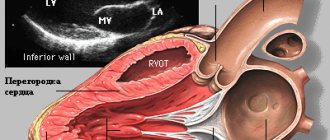
It is important that your consultation with your doctor takes into account lifestyle risk factors, other medical conditions and family history. If there is a risk of cardiovascular disease, an echocardiogram, computed tomography of the coronary arteries, a stress test, cardiac catheterization or an electrocardiogram may be prescribed.
No. 3. CRP to determine the need for urgent kidney drainage
It is highly doubtful that the decision about the need for kidney drainage should be based on the level of CRP. But Angulo JC made such an attempt and published the results of his study in the journal Urology in 2010. The study involved 110 patients with renal colic, 29 of whom underwent emergency kidney drainage. The mean CRP level in patients who required drainage was 140 mg/L. The average level of CRP in patients who did not require drainage was significantly lower – 15 mg/l. The cut-off point was 28 mg/l. The authors conclude that determination of CRP levels in patients with renal colic is an objective and useful tool for deciding whether to place a ureteral stent, even more valuable than leukocyte expression or serum creatinine levels.
CRP and cardiovascular disease
Recently, CRP protein levels have also been taken into account in the diagnosis and treatment of cardiovascular diseases. It is used to assess the risk of myocardial infarction, ischemic stroke and sudden cardiac arrest. It turns out that there is a relationship between the risk of coronary heart disease and the level of CRP in the patient’s blood.
Low levels of CRP accompany mild inflammation, which medicine associates with atherosclerosis because the inflammatory process plays a key role in the detachment of atherosclerotic plaques, the formation of local blood clots and blockage of blood vessels. CRP levels are also associated with hypertension, low good cholesterol, and metabolic disorders leading to abdominal obesity.
According to the Cleveland Clinic, a non-profit multidisciplinary academic medical center (Ohio, USA), the CRP test can be used to identify the risk of developing cardiovascular diseases:
| CRP value | Risk of developing cardiovascular diseases |
| below 1 mg/l | Short |
| from 1 to 2.9 mg/l | Moderate |
| exceeds 3 mg/l | High |
However, the CRP test does not provide a complete picture of the risk of cardiovascular disease.
Other causes of elevated CRP
If the reading is above 10 mg/L, this may be a signal for further research to answer the question of what is causing the inflammation.
Such a high CRP value may indicate:
- osteomyelitis or bone infection;
- tuberculosis;
- inflammatory bowel diseases;
- lupus;
- connective tissue disease;
- some kind of autoimmune disease;
- exacerbation of autoimmune arthritis;
- pneumonia;
- type 2 diabetes;
- cancer – with a special indication for lymphoma.
Increased levels of CRP may occur in women:
- taking birth control pills;
- in pregnant women - this condition may indicate complications, so additional tests should be carried out to be sure.
CRP and cancer
The highest concentrations of CRP are observed in patients with malignant neoplasms, especially neoplasms of the hematopoietic system. Sometimes these are three-digit numbers or more. If the CRP blood test results show a high level of C-reactive protein, doctors immediately begin looking for a neoplastic process that, in addition to the elevated CRP level, has not yet caused any symptoms other than an altered ESR level.
However, keep in mind that the CRP test is not useful in diagnosing cancer. Too many other factors influence its level. A low level of CRP does not exclude the presence of a neoplasm, and its elevated level should direct the diagnosis primarily to infectious and inflammatory diseases. Moreover, the CRP protein is a very plastic molecule: the rate can increase up to a thousand times in 24 or 48 hours - this happens during acute bacterial or viral infections and after serious injuries.
C-reactive protein is the “golden marker”, significant and irreplaceable
Velkov V.V., Candidate of Biological Sciences, CJSC "DIAKON", Prospekt Nauki 5, Pushchino, Moscow region, 142290. Email
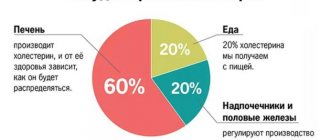
A review of domestic and foreign literature devoted to the analysis of recent advances in the use of C-reactive protein (CRP) for diagnosing a wide range of inflammatory processes and monitoring the effectiveness of therapy for various diseases. Particular attention is paid to the recently discovered mechanisms of the participation of CRP in the initiation and development of atherosclerosis and the use of the method of highly sensitive measurement of baseline hsCRP concentrations to assess the risks of cardiovascular diseases. It is emphasized that for a correct assessment of cardiovascular risks, it is necessary to combine a highly sensitive measurement of hsCRP with measurements of traditional indicators of atherosclerosis: total cholesterol, cholesterol associated with high and low density lipids, apolipoproteins B and AI, and triglycerides.
Intended for specialists in the field of clinical laboratory diagnostics and for medical workers.
For the full article, see https://www.diakon-diagnostics.ru
"C-reactive protein? Yes, it has been known for a hundred years... What could be new there? Well, a nonspecific marker of inflammation. There is one answer to eight troubles. And which one exactly? It’s better to measure ESR, cheap and cheerful. And you don’t need to explain anything for a long time to the attending physician...”
Firstly, not a hundred years, but 75. It was in 1930 that it was discovered, when, when studying blood serum proteins, it was discovered that one of them was contained only in the plasma of patients who had acute diseases. And, most importantly, in the presence of calcium ions, it bound to the C-polysaccharide of pneumococcus. At the same time, a cautious assumption was made: this protein is somehow involved in inflammatory processes. At that time, it was difficult to even imagine what role C-reactive protein would play in medicine and, especially, in clinical laboratory diagnostics.
And secondly, it is simply necessary to tell the attending physician about the modern use of SRP for clinical diagnosis. Otherwise, you can lose not only face, but also the patient.
Structure and functions of the SLO.
CRP belongs to an evolutionarily ancient family of proteins called pentraxins. CRP consists of 5 identical subunits, non-covalently linked to each other. The molecular weight of each subunit is 21-23 kDa, which gives a total molecular weight slightly greater than 100,000. Each member of the pentraxin family has a specific region (the so-called “pocket”) in which the binding site for calcium ions is located. This is necessary so that the protein then binds ligands (in particular, phosphocholine, a hydrophobic component of cell membranes). Another region of pentraxins is responsible for binding receptors and complement C1q. Thus, with one of its sections, SRB “identifies the enemy” - a foreign antigen, and with another, it attracts means to destroy it. In general, CRP has many properties characteristic of immunoglobulins: it binds to bacterial polysaccharides and glycolipids, to damaged membranes and to exposed nuclear antigens. This, in turn, leads to binding to C1q and activation of the classical complement cascade, which, as a result, causes the fixation of cleaved phagolytic complement products. CRP also binds to Fc receptors and increases phagocytosis of certain antigens and microorganisms.
In 1983, the discovery of a new form of CRP was reported. It turned out that the “new” form of CRP accelerated platelet aggregation and serotonin secretion, modulated the metabolism of arachidonic acid, stimulated the release of interleukin, etc. This “new” CRP, “neo-CRP,” has antigenic determinants that are different from those of native CRP and consists of free SRP monomers rather than pentamers. More recently, the functionality of the SRB has been confirmed in great detail. CRP concentrations are known to increase dramatically during the inflammatory response, causing coronary disease through direct activation of endothelial cells. It has been shown that this process requires a transition from native pentameric SRP to its monomeric forms (mSRP). It is believed that in order to induce a proinflammatory process, a transition from the pentameric form of CRP to the monomeric form is necessary.
And just recently, the SRB presented another surprise. Previously, it was believed that CRP subunits are not glycosylated (i.e., do not contain a carbohydrate component). But in 2003, the fact of covalent modification of SRB, and, moreover, of two different types, was established experimentally. It turned out that modification can occur both due to glycosylation and by shortening the amino acid sequence with C and N and the ends of the protein molecule. The functional significance of CRP glycosylation, which occurs in various pathological processes, has not yet been clarified. It is possible that these forms of CRP have altered functional characteristics, such as the efficiency of binding to viruses, bacteria and other pathogens, and perhaps a different ability to activate different complement pathways.
CRP is a central component of the acute phase of the inflammatory process.
In humans, as in other mammals, the acute phase (AP) of the inflammatory process is characterized primarily by an increase in temperature, changes in vascular permeability and changes in the biosynthetic and metabolic profile of many organs. Systems of the whole organism are involved in the development of OF: immune, central nervous, endocrine, cardiovascular. It turned out that one of the central participants of the PF is the SRB. Indeed, during inflammation, the concentration of CRP in the blood plasma increases by 10-100 times, and there is a direct connection between changes in the level of CRP and the severity and dynamics of the clinical manifestations of inflammation. A higher concentration of CRP means a higher severity of the inflammatory process, and vice versa. That is why CRP is the most specific and sensitive clinical and laboratory indicator of inflammation and necrosis. That is why measurement of CRP concentration is widely used to monitor and control the effectiveness of therapy for bacterial and viral infections, chronic inflammatory diseases, cancer, complications in surgery and gynecology, etc. It turned out that different causes of inflammatory processes increase CRP levels in different ways.
With viral infections, tumor metastasis, sluggish chronic and some systemic rheumatic diseases, CRP concentrations increase to 10-30 mg/l. With bacterial infections, with exacerbation of some chronic inflammatory diseases (for example, rheumatoid arthritis) and with tissue damage (surgery, acute myocardial infarction), the concentration of CRP increases to 40-100 mg/l (and sometimes up to 200 mg/l). Severe generalized infections, burns, sepsis increase CRP almost prohibitively - up to 300 mg/l or more. But during inflammation, along with CRP, the concentrations of other proteins also increase.
What does a high CRP warn about?
For diagnosis and for monitoring the course of chronic processes, it is very advisable to monitor changes in the concentration of not only CRP, but also changes in the levels of slower reacting markers of OF: alpha1-acid glycoprotein (orosomucoid) and K-proteinase inhibitor. Monitoring only one inflammatory marker is risky; In some patients, a disharmonious acute phase response is possible. Moreover, increased consumption of haptoglobin, the C3 component of complement, and fibrinogen in the body may indicate the presence of another pathological process accompanying inflammation. The inclusion of negative OF proteins, such as albumin and transferrin, in the study allows us to obtain additional data on the chronic process, general protein catabolism, and the involvement of blood vessels in the development of pathology.
– For acute diseases:
Bacterial infection
. It is with this condition that the highest levels of CRP are observed (100 mg/l and above). With effective therapy, the concentration of CRP decreases the very next day, and if this does not happen, taking into account changes in CRP levels, the issue of choosing another antibacterial treatment is decided.
Sepsis in newborns
. If sepsis is suspected in newborns, a CRP concentration of more than 12 mg/l is an indication for immediate initiation of antimicrobial therapy. But it should be taken into account that in some newborns, a bacterial infection may not be accompanied by a sharp increase in the concentration of CRP.
Viral infection
.
With it, CRP may increase only slightly (less than 20 mg/l), which is used to differentiate a viral infection from a bacterial one. In children with meningitis,
CRP concentrations above 20 mg/l are an absolute basis for starting antibiotic therapy.
Neuropenia
. With neuropenia in an adult patient, a CRP level of more than 10 mg/l may be the only objective indication of the presence of a bacterial infection and the need for antibiotics.
Postoperative complications
. If CRP continues to remain high (or increases) within 4-5 days after surgery, this indicates the development of complications (pneumonia, thrombophlebitis, wound abscess).
Associated bacterial infections.
In any disease or after surgery, the addition of a bacterial infection, be it a local process or sepsis, is accompanied by an increase in the levels of OF proteins, the concentration of CRP becomes greater than 100 mg/l. At the same time, alpha1-antitrypsin and orosomucoid also increase.
Tissue necrosis.
Tissue necrosis causes an acute-phase response similar to that caused by bacterial infection. An acute-phase response is possible with myocardial infarction, with tumor necrosis of the tissues of the kidney, lung, and large intestine. If, with high levels of OF proteins, no obvious signs of inflammation can be detected, this is a clear indication that the patient should be examined for the presence of a malignant disease
– When monitoring the effectiveness of treatment of chronic diseases:.
Systemic rheumatic diseases.
With them, the levels of a whole spectrum of OF proteins sharply increase, and a decrease in their concentration in
rheumatoid arthritis
clearly indicates the effectiveness of treatment.
In systemic vasculitis,
monitoring CRP is an objective test to minimize steroid dosage.
Inflammatory diseases of the gastrointestinal tract.
Crohn's disease is accompanied by severe OF, but with nonspecific ulcerative colitis, OF is insignificant. In functional disorders, OF proteins are usually not increased.
Malignant tumors
. In these cases, various changes in the levels of OF proteins are possible; this depends on the addition of infection, tissue necrosis, dysfunction of organs due to obstruction of the respiratory tract or gastrointestinal tract, and the influence of immunosuppression and chemotherapy. A massive acute-phase response is observed in necrosis of solid tumors. Lymphomas, on the contrary, are rarely accompanied by tissue necrosis and changes in the spectrum of plasma proteins. In myeloma, very strong OF is possible, caused by increased synthesis of IL-6 by tumor cells - this is a poor prognostic sign.
Secondary amyloidosis.
Elevated CRP levels correlate with the development of renal complications.
Transplant rejection.
In cardiac allograft rejection, high CRP correlates with infectious complications but does not indicate rejection per se. But in case of kidney transplant rejection, a strong acute phase response is one of the early indicators of rejection.
Thus, a significant increase in the level of CRP and other OF proteins can quite clearly indicate both the diagnosis and the effectiveness of the therapy. But this is far from the end of the clinical significance of determining CRP concentrations. In 1680, Antoine Van Leeuwenhoek increased the sensitivity of the human eye 270 times and, looking through a microscope, saw life in a completely new dimension. The same thing happened with SRB, when in 1994-1997. a new highly sensitive method for measuring its concentrations was discovered.
HsCRP is a highly sensitive method for measuring CRP concentration.
Classical methods for determining the concentration of CRP in blood plasma/serum are radial immunodiffusion, immunoturbidimetry and nephelometry. Elevated concentrations of CRP, which are determined in pathology, are in the range of 5-500 mg/l or more, i.e. lie within the concentration range determined by the specified methods. And for a very long time, the diagnostic value of CRP was correlated precisely with indicators exceeding 5 mg/l. And when the CRP concentration was less than 5 mg/l, the absence of a systemic inflammatory response was stated, and in general, an accurate determination of the CRP concentration was not considered clinically significant. But only until, to increase the sensitivity of the analysis, antibodies to CRP began to be immobilized on latex particles. This increased the sensitivity of CRP determination by approximately 10 times. And the lower limit of the detection range for CRP when using high-sensitive (hs - high sensitive) latex-enhanced immunoturbidimetry is now approximately 0.5 mg/l. As a result, kits have been introduced into laboratory practice that allow the determination of CRP concentrations that were previously considered “normal,” “trace,” or simply “background.” Now such concentrations are called basic.
The basic concentration of CRP is the level that is consistently detected in practically healthy individuals, as well as in patients in the absence of an acute inflammatory process or without an exacerbation of the disease. It is to determine baseline levels of CRP that hsCRP methods are used.
Here are the main reasons that led to the widespread use of the hsCRP method:
1) hsCRP is simple and applicable even in outpatient settings; 2) the results of determining hsCRP in fresh, stored and frozen plasma are practically the same; 3) unlike short-lived cytokines, which are characterized by daily fluctuations in concentrations, hsCRP levels are quite stable due to its relatively long half-life from the body; 4) the hsCRP method is standardized, there are standards certified by WHO and reliable control materials.
What do changes in baseline CRP concentrations indicate?
Cardiovascular diseases.
As a result of numerous and large-scale studies, it has been established that measuring baseline levels of CRP has a prognostic value, which: allows you to assess the degree of risk of developing:
– acute myocardial infarction, – cerebral stroke and – sudden cardiac death in persons without cardiovascular disease.
At baseline SRP concentrations (mg/l)
– less than 1.0 – risk of vascular complications (acute myocardial infarction, stroke) – minimal, – at 1.1-1.9 – low, – at 2.0-2.9 – moderate, – at more than 3 mg/l - high.
In general, hsCRP levels between 3 and 10 mg/L are a sign of low-grade inflammation and are associated with a high risk of cardiovascular disease. For risk stratification of cardiovascular diseases, a CRP level not exceeding 10 mg/l is significant. If the level of CRP is higher, it is associated with acute inflammation, chronic disease, injury, etc.
For acute coronary syndrome
Destabilization (rupture) of atheroma and thrombus formation are associated with inflammatory processes. In patients with unstable angina, elevated baseline levels of hsCRP occur much more often (in 70% of patients) than in exertional angina (in 20% of patients). Moreover, among patients with unstable angina who developed acute myocardial infarction, hsCRP levels were elevated (> 3 mg/L) in almost all (98%) patients.
Risk of early mortality
. When stratifying the risk of early (up to 14 days) mortality in patients with unstable angina and acute myocardial infarction, the most informative is the combined determination of hsCRP and the level of cardiac troponin T. An increase in both of these risk markers (hsCRP > 1.55 mg/l, troponin T > 0, 1 mg/l) indicates a high risk of death. Levels of hsCRP < 1.55 mg/l and troponin T < 0.1 mg/l indicate minimal risk.
Complications after cardiac surgery
. In such patients, initially elevated hsCRP is associated with a risk of early delayed complications after coronary artery bypass graft surgery. In angioplasty with coronary artery stenting in patients with coronary artery disease (CAD), high baseline hsCRP levels are associated with a higher risk of subsequent restenosis. The connection between the hsCRP level and the risk of complications after invasive treatment of coronary artery disease is evidenced by the following: only in 12% of patients with coronary artery restenosis that developed after angioplasty with stenting, the hsCRP level was <5 mg/l (in combination with a normal ceruloplasmin level, >2 g/l). l). All patients with hsCRP levels >9 mg/l (in combination with a reduced ceruloplasmin level <0.2 g/l) developed coronary artery restenosis.
Heart transplantation.
In such patients, coronary artery disease of the transplanted heart is the leading cause of death a year or more after transplantation. It turned out that the processes of chronic inflammation in the vessels of the heart are also significant in the development of this pathology. Increasing baseline hsCRP levels doubled the risk of graft failure by 36%. And advanced coronary artery disease in the transplanted heart is associated with higher basal plasma hsCRP levels.
Primary and secondary prevention of cardiovascular diseases and their complications.
Despite the fact that hsCRP is an independent predictor of the risk of cardiovascular diseases and complications, analysis of a large amount of data has revealed correlations between the level of hsCRP and a number of classical risk factors (such as smoking, obesity, insulin resistance, etc.). Baseline CRP levels may determine the effectiveness of treatment of cardiovascular diseases and their complications. By quitting smoking, regular physical activity, moderate alcohol consumption, and treating obesity, the baseline level of hsCRP decreases and coronary risk decreases. Taking aspirin to prevent vascular complications is effective only in individuals with initially elevated baseline hsCRP levels. Taking statins to prevent coronary artery disease is also effective in individuals with elevated baseline hsCRP levels.
In general, hsCRP is an independent and strong predictor of acute myocardial infarction in apparently healthy middle-aged individuals of both sexes, in the elderly, and in patients with coronary artery disease. But we especially emphasize: the greatest prognostic significance is the joint determination of hsCRP and the atherogenic index (hsCRP + oC/HDL-C), total cholesterol/high-density cholesterol.
Atherosclerosis.
If previously it was believed that this disease was caused by disorders of metabolism and lipid transport, now it has become obvious that inflammation plays a large role in atherogenesis, including the initiation and development of damage to the vascular wall, instability of atheroma and the occurrence of thrombotic complications. According to the current concept of atherogenesis, atherosclerosis is a long-term, sluggish chronic inflammation in the intima of a vessel. This makes clear the connection between inflammatory mediators and risk factors for the development of atherosclerosis. Low-active, low-grade inflammation, which is detected by changes in hsCRP, predicts the risk of developing atherosclerotic complications. When determining the hsCRP level, the characteristics of the method (test) can significantly influence the use of this parameter in practice. Blood for hsCRP measurement can be collected either fasting or postprandial in metabolically stable patients. The determination of hsCRP is carried out in duplicates; it is advisable to repeat the measurement after two weeks. When interpreting hsCRP results, the following recommendations should be followed:
– with hsCRP < 1 mg/l – the risk of atherogenesis is low; – with hsCRP 1-3 mg/l – the risk is medium, – with hsCRP > 3 mg/l – the risk is high.
If the hsCRP level is > 10 mg/L, the measurement is repeated and the patient is examined to identify infectious and inflammatory diseases.
In general, the baseline level of hsCRP carries independent prognostic information and complements the data of traditional risk factors for atherogenesis.
Can mutations in the CRP gene that increase its basal level be a cardiovascular risk factor?
In 2005, several articles were published at once, according to which some mutations in the CRP gene (in particular, some mutations in its promoter) lead to an increase in its basic level in plasma and, which is significant, regardless of traditional cardiovascular risk factors. One mutation in the promoter of the CRP gene was found to be strongly associated with elevated levels of CRP, predominantly in individuals with cardiovascular disease. However, no difference in the frequencies of this allele (gene variant) was found between post-infarction patients and the control group. Perhaps the risk of heart attacks and the risk of mild cardiovascular problems are associated with different mutations in different regions of the CRP gene? As a result of long-term and large-scale studies (3790 individuals were observed, whose age at the beginning of observation was from 7 to 15 years) an association was identified between mutations in the promoter region of the CRP gene, plasma CRP levels and cardiovascular risk. Mutations have been found that are strongly associated with elevated levels of CRP in the plasma of individuals with cardiovascular problems. However, the authors believe that at the moment, the question of whether a genetically determined increase in CRP is a marker of cardiovascular diseases or their causative agent does not yet have a clear answer. But, according to the authors, the results they obtained may indicate that SRB is still a causative agent. Mutational substitutions in the promoter predict CRP levels throughout life, independent of other factors correlated with elevated CRP levels (in particular, independent of body mass index). It is believed that if CRP is a causative agent of cardiovascular diseases, then its genetic variants associated with increased CRP should also be associated with an increased risk of cardiovascular diseases. At this time, the average age of the study cohort is 42 years and therefore the number of recorded cardiovascular events that occurred in it is not yet sufficient to give a definitive answer. The authors conclude that mutations in the CRP gene promoter that significantly affect baseline plasma CRP levels should be taken into account when risks are assessed using hsCRP. And, moreover, they believe it is necessary to develop molecular genetic tests for screening various alleles (variants) of the CRP gene, which will allow stratifying healthy people into groups according to their high or low risk in relation to inflammatory diseases
DRR: prospects for application and study.
Massive measurements of CRP levels carried out in the last decade for the purposes of laboratory clinical diagnostics, as well as the study of the structure and numerous functions of this protein, have led to new ideas about both its diagnostic value and its participation in the occurrence and development of certain pathologies. It has become even more clear that measurements of CRP concentrations, especially its baseline concentrations tested using the hsCRP test, must be carried out in conjunction with measurements of other biochemical and immunological indicators, the choice of which can be dictated by many factors. The results of such complex analyzes are of great importance not only for the individual treating physician, but also, when summarized and published, may be important for the development of various specialized diagnostic kits that include the measurement of both CRP and hsCRP.
Particularly promising is the study of the mechanisms of CRP modifications (glycosylation, changes in amino acid sequences) that occur in various pathologies. It is possible that different modified forms of SRP can be correlated with specific forms of pathologies and/or with their quantitative manifestations. This, in turn, could lead to the development of more sensitive and/or more specific diagnostic tests. Moreover, this may lead to the creation of new therapeutic agents aimed at inactivating those properties of CRP that can lead to the emergence and development of pathologies caused by it.
Internet magazine “Commercial Biotechnology” https://www.cbio.ru/
Elevated CRP – is this always a pathology?
In adults, an elevated CRP value exceeds 5 mg/l, with the exception of smokers, people with obesity or hypertension, for whom the norm is less than 10 mg/l.
In older children, elevated CRP values are considered to be greater than 10 mg/L. As with adults, interpretation of the result should be left to the pediatrician. He will evaluate the result in the context of the child's condition and medical history.
Slightly elevated CRP values up to 40 mg/l may be observed in older people and during pregnancy.
Therefore, when interpreting the results and drawing up a medical report, it is necessary to take into account other laboratory parameters, such as a complete blood count (CBC) with a leukocyte formula.
Effect of drugs on CRP concentration
Taking acetylsalicylic acid or aspirin, even in high doses, does not affect the quantitative level of CRP. This is somewhat surprising since aspirin is known for its anti-inflammatory properties.
Patients with high cholesterol who take statins are less likely to have a heart attack because statins not only lower lipid levels but also have anti-inflammatory properties. This is very important because high CRP and low cholesterol are more dangerous than high cholesterol and low CRP. The level of CRP is also reduced by drugs from the group of fibrates and beta-blockers, but less effectively than by statins.
C-reactive protein and ESR
ESR or Birnatsky reaction is a measurement of the erythrocyte sedimentation rate in a test tube with blood. It is expressed in millimeters per hour. ESR is an indirect indicator of the inflammatory response. However, the ESR test is less specific than CRP.
In addition to inflammation, an increase in ESR is also affected by:
- Obesity. Adipose tissue is a source of interleukin 6. This is one of the proteins involved in the formation of inflammation.
- Kidney failure. In end-stage renal failure and in the case of nephrotic syndrome, patients have significantly increased ESR values.
- Hemoglobin concentration. Anemia speeds up the decline of red blood cells.
- Shape of red blood cells. Determination of ESR is unreliable in diseases with abnormal red blood cells, such as sickle cell disease.
If there is a disproportion between CRP concentration and ESR, the first step is to consider the possibility of a false measurement due to the above factors or laboratory error, such as taking too long from collection to delivery to the laboratory or storing the tube in inappropriate conditions.
CRP levels respond more dynamically to increased inflammation than ESR. In the case of, for example, lupus erythematosus, the ESR value may be elevated when the level of CRP in the blood is low. This is caused by high levels of type 1 interferon, which suppresses the liver's production of CRP.
If you find an error, please select a piece of text and press Ctrl+Enter