General blood analysis. What do the results mean?
So, you have passed a general blood test (also known as a clinical analysis, also known as a detailed analysis). It doesn’t matter whether you gave it from a vein or from a finger, as a result you will get a certain set of letters and numbers that are completely incomprehensible to the uninitiated. What does it mean?
Let's look at the main letter combinations that are found on modern general blood test forms. Of course, on modern general blood test forms there is also a detailed analysis. It doesn’t matter whether you took it, what’s written on the piece of paper is important and interesting.
R.B.C.
(red blood cells - red blood cells) - erythrocytes.
This is the first thing we pay attention to. Erythrocytes are red blood cells that provide the basic vital functions of all body tissues by carrying oxygen.
Norm: men: 4.0-5.0·1012/l; women: 3.5-4.7 1012/l.
Increased: or “erythrocytosis” can be observed either due to an increase in their synthesis in the red bone marrow, for example, with tumor growth (erythremia), due to diseases of the cardiovascular and pulmonary systems that lead to heart or pulmonary failure (as an attempt the body to compensate for the lack of oxygen), due to narrowing of the lumen of the renal artery, due to dehydration of the body (vomiting, diarrhea, active sweating).
Decrease: or “erythropenia”, the causes of which, firstly, are food poor in nutrients and vitamins, and secondly, increased destruction due to bleeding (both external and internal, which may not appear immediately), in - thirdly, due to hereditary enzymopathies or disturbances in the enzyme system responsible for the synthesis of red blood cells, fourthly, due to hemolysis (destruction of cells as a result of intoxication or autoimmune processes, when the body perceives its own elements as foreign), fifthly, due to tumor diseases of the hematopoietic system.
WBC
(white blood cells - white blood cells) - leukocytes.
These are white blood cells, the “protective dogs” of the body, exercising immune control, neutralizing foreign elements and getting rid of viruses and bacteria.
Norm: for men and women 4.0*109/l–9.0*10/l.
Increase: called “leukocytosis” and indicates that some kind of inflammatory reaction is occurring in the body. It is also typical for malignant tumors, injuries, myocardial infarction of the acute and subacute phases, the period of exacerbation of rheumatism, pregnancy (last trimester) and after the childbirth period. May be detected after heavy physical activity and during menstruation
Decreased: or “leukopenia” may indicate diseases of the red bone marrow of a tumor nature (leukemia), radiation sickness after exposure to ionizing radiation, viral infectious diseases (influenza, typhoid fever, malaria, rubella, measles, mumps), viral hepatitis), observed when taking anticancer drugs, as an inevitable effect. There are 5 types of leukocytes in total: granulocytes, which contain granules in the cytoplasm that are stained with special dyes (neutrophils, eosinophils, basophils) and agranulocytes, which do not have specific granules (monocytes and lymphocytes).
GR
% – relative (%) content of granulocytes and GR# – absolute content of granulocytes. Let's look at some of them:
NEUT
% (NE%) (neutrophils) – relative content of neutrophils. Neutrophils are cells that “live” in the bloodstream and, if necessary, move into the tissue, becoming macrophages that absorb and digest foreign viruses and bacteria.
Normal: segmented (mature) 47-72%, band (young) 1-6%.
Increased: infectious and inflammatory processes, myocardial infarction, chronic metabolic disorders (diabetes mellitus), taking immunostimulants.
Reduction: infectious diseases (typhoid fever, brucellosis, influenza, measles, varicella (chickenpox), rubella, viral hepatitis), blood diseases, high levels of thyroid hormones (thyrotoxicosis), consequences of chemotherapy and radiotherapy.
A shift in the leukocyte formula to the left means that young, “immature” neutrophils appear in the blood, which are normally present only in the bone marrow. This happens with mild and severe infectious and inflammatory processes, as well as with acute blood loss, diphtheria, pneumonia, scarlet fever, sepsis, and intoxication.
A shift in the leukocyte formula to the right means that the number of “old” neutrophils (segmented) in the blood increases, and the number of nuclear segments becomes more than five. This picture occurs in healthy people living in areas contaminated with radiation waste, as well as with a lack of certain vitamins (B12, B6).
EO
% – relative content of eosinophils. These are cells that cleanse the body of toxic substances, parasites and help get rid of cancer cells.
Norm: 0-5%.
Increase: mainly for allergies, parasitic and rheumatic diseases. A frequent indicator of the presence of bronchial asthma.
Decreased: with intoxication with heavy metals, severe purulent processes, indicates the beginning of the inflammatory process.
B.A.
% – relative content of basophils. These are cells that are much larger than other leukocytes; they take part in the formation of delayed immunological inflammatory reactions. Yes, these are the main cells that form an allergic reaction, producing substances that cause swelling, hyperemia, and inflammation.
Norm: 0-1%.
Increase: with a decrease in thyroid hormones (hypothyroidism), blood cancer (chronic myoleukemia), allergies, chicken pox, nephrosis.
LYM
% (LY%) (lymphocyte) – relative content of lymphocytes.
Norm: 19-37%.
Increased (lymphocytosis): viral infections, poisoning, use of certain drugs.
Decreased (lymphopenia): tuberculosis, lupus, renal failure, immunodeficiency, consequences of chemotherapy and radiation therapy.
MON
% (MO%) (monocyte) – relative content of monocytes. These are the largest cells of the immune system. They recognize foreign substances and teach other white blood cells to recognize them.
Norm: 3-11%.
Increased: viral infections, autoimmune diseases, diseases of the hematopoietic system.
Decreased: aplastic anemia, consequences of childbirth or surgery, purulent lesions.
HGB
(Hb, hemoglobin) – hemoglobin, concentration in whole blood. This is a substance found in red blood cells that is capable of absorbing oxygen (up to 8 molecules at a time).
Norm: women: 120–140 g/l, men: 130–160 g/l.
Increased: dehydration, diabetes, kidney dysfunction, heart and lung defects, disease of the hematopoietic organs.
Decreased: anemia, iron deficiency, vitamin deficiency, blood loss, exhaustion of the body.
HCT
(hematocrit) - hematocrit. This is the percentage ratio of the volume of blood taken to the volume occupied by red blood cells. It is determined so that it is possible to distinguish a change in the volume of a liquid from a relative change in the volume of red blood cells in it.
Norm: 38.0-49.0%.
Increase: “thickening” of the blood, an increase in the content of red blood cells and a decrease in plasma volume (see erythrocytosis).
Decreased: “thinning” of the blood, a decrease in the content of red blood cells (anemia, renal failure, 2nd half of pregnancy), an increase in plasma volume due to increased fluid consumption.
MCH
– average hemoglobin content in an individual red blood cell. The index reflects how much red blood cells are filled with hemoglobin. Important for identifying and distinguishing different types of anemia (for example, hemolytic and iron deficiency).
Normal: 24–33 picogram.
Previously, the so-called color index (ratio) was used. Its norm is 0.85-1.05.
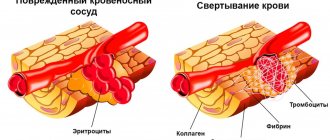
PLT
(platelets - blood platelets) - platelets in absolute numbers. These are blood cells that are pieces of megakaryocytes (giant cells located in the red bone marrow), which are responsible for blood clotting.
Norm: 180-320*109/l.
Increased: blood clotting increases with the removal of the spleen, various types of anemia, erythremia, condition after operations, physical fatigue.
Decreased: blood clotting decreases with congenital blood diseases, autoimmune pathologies, renal vein thrombosis, blood transfusion, blockage of renal veins by blood clots and other conditions.
ESR
- erythrocyte sedimentation rate. The rate at which erythrocytes settle and the separation of the transparent part (plasma and white blood cells) and the erythrocyte mass in the column is observed. This analysis indicates the state of the red blood cell membrane (normally, the membranes have a negative charge and repel, reducing the sedimentation rate), or a quantitative change in blood proteins that are capable of gluing red blood cells into columns, increasing the sedimentation rate. The indicator is very nonspecific, quite variable and has many manifestations in many conditions.
Normal: 2–12 mm/hour.
Increase: infectious and inflammatory diseases, malignant tumors, injuries, kidney diseases, taking medications.
Decreased: recovery from illness, exhaustion of the body, severe traumatic brain injury, some medications (diclofenac, aspirin, immunosuppressants, hormones).
Hematocrit norms
Hematocrit values depend on age, as well as gender (in adults).
Important! Standards may vary depending on the reagents and equipment used in each particular laboratory.
That is why, when interpreting the results, it is necessary to use the standards adopted in the laboratory where the analysis was carried out. You also need to pay attention to the units of measurement. Generalized standards adopted in Russia are given in the table:
Western medical literature provides more general reference values:
- Men - 0.40-0.54 / 40-54%
- Women - 0.36-0.46 / 36-46%
- Newborns - 0.53-0.69 / 53-69%
Factors influencing the result:
Hematocrit increases against the background
- stress,
- taking corticosteroid drugs and diuretics,
- traumatic shock accompanied by intense pain.
A decrease in hematocrit is facilitated by:
- prolonged immobility;
- taking blood thinners (disaggregants, anticoagulants);
- high fluid intake;
- chronic alcoholism.
Important! The interpretation of the results is always carried out comprehensively. It is impossible to make an accurate diagnosis based on only one analysis.
Results
The hematocrit value (HCT) is a reflection of the red blood cells (RBCs) in the blood relative to the plasma. The hematocrit level is determined as part of a general clinical blood test. HCT laboratory standards are developed taking into account the age and gender of the individual.
Women's normative values are lower than men's, which is associated with monthly blood loss. The upper limit of HCT for women of reproductive age is 45%. With the onset of the premenopausal period and during menopause, the norm increases to 47%. During the perinatal period, the hematocrit number decreases due to thinning of the pregnant woman's blood. For men under 45 years of age, the reference value is 39–49%, for men over 45 years of age, 49–50%.
The reasons for the increase in the indicator are:
- chronic pathologies of the cardiovascular system and respiratory organs;
- dehydration of the body;
- oxygen deficiency due to smoking or intense sports training.
A decrease in hematocrit number, first of all, indicates anemia (anemia). Children's values increase as they grow older. In newborns, the level is elevated due to changes in living conditions. A pathologically high rate is recorded during oxygen starvation (hypoxia) of the baby during birth. If there are systematic deviations of hematocrit, hemoglobin and red blood cells from the reference values, the patient needs advanced laboratory and hardware diagnostics.
Platelets
(TC)
– the most important element of blood clotting. They store the protein thromboplastin in themselves and, if necessary to urgently stop bleeding, they explode and throw it into the blood. A lack of TC indicates a possible increased bleeding, a threat of bleeding, an excess indicates a tendency to thrombosis. Both are bad. The norm ranges from 180 thousand to 320 thousand. The number of TC in the analysis strongly depends on the state in which the person took the test - nervous, smoked before donating blood, or took alcohol the day before. A deviation from the norm of 10% is acceptable.
Physiological reasons for changes in hematocrit levels
A natural change in hematocrit level, which is not a consequence of the disease, occurs in the following cases:
- Pregnancy. In women in the second and third trimester of the perinatal period, plasma volume increases significantly, while the number of red blood cells does not change. The blood becomes more dilute, so the hematocrit number drops to 35–40%. In addition, during delivery, heavy blood loss is often observed. In the postpartum period, the ratio of the liquid part of the blood and the formed elements should return to its original values.
- The first 6–7 days of the follicular phase of the menstrual cycle. During the period of natural blood loss by the female body, the composition of the blood changes. The hematocrit percentage decreases. The maximum permissible difference is 5%.
- Conditions associated with oxygen deficiency in body tissues. To compensate for the lack of oxygen, the body strives to produce more red blood cells, and accordingly, the hematocrit increases. An increased need for oxygen occurs during intense sports training (other physical overload), nicotine addiction, and in high mountain climates. And this condition is also observed in newborns, especially with complicated delivery, accompanied by fetal hypoxia.
In the absence of chronic diseases, a slightly reduced HCT is not considered a pathology in people over 65 years of age.
Hematocrit - what is it, what does it depend on
Hematocrit analysis provides data on the ratio of the volume of red blood cells to the total volume of blood; sometimes this indicator refers to the ratio of the volume of all formed elements to the total volume. There is no particular difference between the interpretations; 99% of the blood cell volume is made up of red cells. More often, hematocrit is recorded as a percentage of the total volume, less often as a ratio of cell volume to total blood volume.
This indicator is determined as part of a general blood test complex. It is classified as secondary and is calculated based on data on the number of red blood cells. Occasionally, direct measurement of hematocrit is performed by centrifuging the sample. This procedure allows you to separate plasma from formed elements and directly measure this indicator.
Indications and preparation for analysis
Indications for hematocrit analysis are symptoms indicating the development of anemia or other diseases of the blood or hematopoietic system. These include:
- Pale or jaundiced skin
- Enlarged spleen, liver
- Changes in the size of lymph nodes
- Digestive disorders
- Skin and hair problems (rashes, ulcers on mucous membranes, hair loss or brittleness)
In addition to identifying anemia, the analysis allows us to identify other diseases, for example, polycythemia (a chronic disease in which the bone marrow produces an excess amount of red blood cells) of various origins. This study is also used when it is necessary to assess the need for blood transfusion and calculate the required volume of transfusion.
No special preparation is required for the hematocrit test. It is necessary to follow the standard rules for conducting a general blood test:
- Blood is drawn early in the morning.
- You should not eat food 6-10 hours before the test.
- Avoid alcohol 2-3 days before the procedure.
Patients who smoke are advised to abstain from smoking for at least 2-3 hours before blood collection. If these recommendations are not followed, the analysis may give unreliable results. This is due to the fact that the composition of the blood is subject to strong fluctuations depending on the action of various environmental factors.