Blood is the most informative biological fluid. A biochemical blood test allows you to assess the intensity and direction of metabolic processes and clarify the antigenic status. The data clarifies the features of protein, fat, carbohydrate metabolism, enzyme concentrations, and excludes or records changes in homeostasis.
Patients' blood is taken from the ulnar vein (volume 5–20 ml). The selection is carried out on an empty stomach so that the interpretation of the biochemical blood test is reliable. Before taking tests for the concentration of lipoproteins or cholesterol, you should undergo a 12-14-hour fast. The determination of uric acid will be reliable if 3 days before sampling you exclude dishes from the liver, kidneys, coffee, and tea.
Complexes with this research
Advanced women's anti-aging diagnostics Advanced monitoring of basic blood parameters in women aged 40+ 28,680 RUR Composition
For those at risk of COVID-19 Diagnosis of diseases complicating the course of coronavirus infection 4,510 RUR Composition
Women's check-up No. 1 38 studies for annual preventive examination RUB 19,290 Composition
IN OTHER COMPLEXES
- Biochemistry of blood. 19 indicators 6,280 R
- Diabetes monitoring RUB 1,900
- Vegetarians and vegans RUB 5,820
- Women's anti-aging diagnostics RUB 12,070
- Biochemistry of blood. 13 indicators 3,490 RUR
Albumin and its biochemical norm (ALB)
Total protein is represented by several fractions, the main one being albumin. The role of the latter is associated with maintaining a constant volume of fluid in the blood and transporting various chemical compounds. Since the synthesis of this protein occurs in the liver, its concentration in the blood can be used to judge the functioning of hepatocytes and the presence of liver pathology.
The starting material for the formation of protein molecules is amino acids. Some of them are synthesized endogenously, and the other part comes from food. In this regard, the determination of ALB is necessary for a full study of protein metabolism and the plastic (regenerative) capabilities of the body. The last factor is of particular importance in studying the dynamics of patient management after major operations, injuries, burns; it allows one to predict the healing process and, if necessary, adjust it in case of hypoalbuminemia.
In a healthy adult, the norm is 35-50 g/l. A decrease in concentration is observed when the synthetic function of the liver is impaired due to:
- Toxic or viral hepatitis;
- Fatty hepatosis;
- Alcoholic or biliary cirrhosis;
- Growth of primary tumors (hepatocellular or cholangiocellular cancer);
- Metastatic lesion.
The deficiency may also be caused by:
- Low protein content in food;
- Prolonged fasting;
- High need for a recovery period after surgery and serious injuries;
- Increased utilization during cancer intoxication;
- Losses due to fluid accumulation in the chest (hydrothorax) and abdominal cavity (ascites);
- Kidney failure, which is accompanied by loss of protein in the urine.
For diagnostic and preventive purposes, it is necessary to study ALB in patients:
- After major invasive interventions;
- After prolonged therapeutic fasting (surgeries on the digestive organs, pancreatitis);
- A few days after the evacuation of pleural and abdominal height;
- If liver and kidney symptoms occur;
- In case of edema of unknown origin;
- With intensive treatment with corticosteroids;
- In athletes and people involved in heavy physical labor.
Timely detection of albumin deficiency allows one to avoid the development of severe consequences in the form of “hunger edema”, a decrease in the body’s regenerative function and the ability to eliminate toxins.
Detailed description of the study
Albumin is a blood plasma protein that, by mass, occupies more than half of all plasma proteins. It performs a number of important physiological functions:
- Maintaining physical and chemical blood parameters: viscosity, pH, oncotic pressure;
- Regulation of circulating blood volume and its balance with intercellular fluid;
- Transport of certain hormones, drugs, fats and their complexes;
- Calcium binding and participation in its metabolism;
- Protein reserve: if there is not enough protein in food, albumin can become its source.
Albumin is synthesized in the liver under the influence of thyroid hormones and growth factors, and is excreted by the kidneys. If too little of it is produced in the liver or if it is excessively excreted in the urine, its plasma concentration decreases. This condition is called hypoalbuminemia.
The causes of low albumin levels can be acute and chronic liver diseases, which affects its synthetic function, kidney pathologies, and insufficient protein intake from food. Hypoalbuminemia can be a manifestation of hormonal diseases, intestinal pathologies and cancer. Regardless of the cause, a decrease in plasma albumin levels manifests itself externally as edema.
Physiologically, this is reflected in the properties of blood and transport functions. For example, the content of free molecules of drugs taken in the blood will increase. This may increase their side effects.
Increases in plasma albumin levels are rare: with dehydration or recent intravenous protein administration.
Albumin, globulins, urea – indicators of protein metabolism
A decrease in the amount of albumin to a level of less than 30 g/l causes edema. Its norm ranges from 35 to 55 g/l. A decrease indicates malnutrition of protein products, toxic liver diseases, colitis, and enteritis. Normally, the albumin content is in the range of 40–60% of the total amount of protein fractions.
The amount of α-globulins is 9–18%, β- and γ-globulins are 8–15 and 12–22%, respectively. An increase in globulins confirms inflammation. An indicator of an acute form of inflammation is C-reactive protein, which, as shown by a biochemical blood test, is not normally found in healthy people.
Blood urea is an indicator of protein metabolism. A biochemical blood test in children shows that normally its level ranges from 1.8 to 6.4 mmol/l, in adults – from 2.1 to 7.1. An increase indicates consumption of high-protein foods, kidney disease, a decrease indicates fasting or a violation of the protein-synthesizing function of the liver.
Cholesterol and lipids
When determining the amount of cholesterol, pay attention to advanced indicators of a biochemical blood test: both the total concentration and the ratio of different lipid fractions. The norm is considered to be within the range of 3.6–5.2 mmol/l; an increase is recorded when it is above 6.5. Cholesterol consists of HDL and LDL (high and low density lipids).
If VLDL (very low density lipids) and chylomicrons predominate, this indicates vascular congestion, atherosclerosis, and hypertension.
An additional indicator for diagnosing coronary artery disease and atherosclerosis (using biochemical blood test data in adults) is the amount of triglycerides. Their norm is 1.7–2.25 mmol/l, the highest level starts at 2.26.
Reference values for albumin in blood
Important! Standards may vary depending on the reagents and equipment used in each particular laboratory. That is why, when interpreting the results, it is necessary to use the standards adopted in the laboratory where the analysis was carried out. You also need to pay attention to the units of measurement.
Normal values of albumin in blood serum according to the independent laboratory Invitro:
| Age | Albumin (in blood), g/l |
| up to 6 months | Reference values for children under 6 months. not validated. |
| 6 months -14 years | 38-54 |
| 14-90 years | 35-52 |
| over 90 years old | 29-45 |
Helix laboratory standards:
| Age | Reference values |
| < 4 days | 28 - 44 g/l |
| 4 days - 14 years | 38 - 54 g/l |
| 14 – 18 years old | 32 - 45 g/l |
| > 18 years old | 35 - 52 g/l |
Important! The interpretation of the results is always carried out comprehensively. It is impossible to make an accurate diagnosis based on only one analysis.
Who needs to get tested
Blood test for albumin
used in conjunction with data from other studies in the diagnosis of many diseases. Most often, the analysis is prescribed for suspected pathologies of the kidneys and liver. Its results are also used to assess the health status of patients with cancer diagnoses, major injuries or burns. The test is prescribed independently or in combination with other tests. The composition of the examination required in a particular case is determined by the doctor based on the patient’s complaints, examination results, and medical history.
conclusions
The amount of ALB is required to diagnose a number of diseases and select the optimal treatment tactics. It characterizes metabolism and overall health. In case of severe symptoms of kidney problems, this test is prescribed first. It can also be carried out as part of a comprehensive examination or after it, if deviations are identified and it is necessary to clarify their nature and cause. Interpretation of the results can only be carried out by a doctor; the test is not intended for self-diagnosis
. In some cases, deviations from the norm are possible in the absence of diseases.
Physiological changes in blood parameters during pregnancy
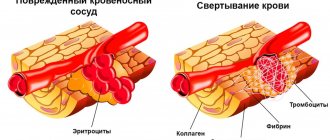
Changes in coagulogram and clinical blood test parameters.
Changes in the coagulogram
(No. , , , , 190, 164, 194)* of a pregnant woman are a physiological process associated with the appearance of the uteroplacental circulation.
This process is associated with the evolutionary, adaptive reactions of the body of a pregnant woman. A woman’s body prepares for costs during pregnancy and possible blood loss during childbirth. During the physiological course of pregnancy, the activity of the procoagulant link increases. Already in the 3rd month of pregnancy, fibrinogen increases (this is factor I (the first) of the plasma coagulation system) and reaches its maximum values on the eve of childbirth. Therefore, gynecologists reasonably recommend monitoring this indicator during pregnancy (once per trimester, if there are deviations in these indicators, more often, once a week). At the end of the third trimester of pregnancy, the concentration of fibrinogen in the serum increases, which may correspond to an increase in the processes of intravascular coagulation in the uteroplacental bloodstream. Simultaneously with the increase in fibrinogen and the activity of the external coagulation pathway, the activity of the internal blood coagulation mechanism also increases, and a shortening of the aPTT is noted. Other parts of the hemostatic system also change during pregnancy, such as the coagulation inhibitor antithrombin III, which has a protein structure and has the ability to inhibit two or more coagulation factors, fibrinolysis and the complement system. As pregnancy progresses, there is a gradual decrease in the activity of antithrombin III. In pregnant women, starting from early pregnancy, the level of D-dimer in the blood gradually increases. By the end of pregnancy, its values can be 3-4 times higher than the initial level. Lupus anticoagulant should not be produced normally in a pregnant woman. Pregnant women may experience minor changes in the general blood count (No. 5)*. Indicators such as hemoglobin and hematocrit may decrease in the second half of pregnancy, and leukocytes may increase (No. 119)*. Changes in biochemical parameters
During pregnancy, a decrease in the total protein concentration in the blood plasma is due to both partial dilution, as a result of fluid retention in the body, and a decrease in the concentration of albumin (No. 10)*. The decrease in albumin is due to its increased consumption on biosynthetic processes. However, it is impossible to exclude the factor of increased vascular permeability and redistribution of fluid and protein in the intercellular space, and hemodynamic disturbances. Changes in the concentration of blood proteins are also detected on the proteinogram. In the first and second trimester of pregnancy, albumin decreases, which is associated with physiological hypervolemia. In the third trimester, an increase in the alpha-1-globulin fraction (No. 29)* and alpha-fetoprotein (No. 92)* is detected. Alpha-2-globulin fraction (No. 29)* can increase due to proteins associated with pregnancy (begin to increase from 8-12 weeks of pregnancy and reach a maximum in the third trimester). Beta globulins (No. 29)* increase due to an increase in transferrin concentration (No. 50)*. Also, in most cases there is a slight increase in the level of gamma globulins (No. 29)*.
Minor changes in C-reactive protein (No. 43)*, observed more often in early pregnancy, may be the body’s response to proliferation processes (increased cell division). Changes in circulating blood volume (CBV) and blood supply to the kidneys lead to changes in the nitrogen excretory function of the kidneys. There is a delay and accumulation of nitrogenous substances, while the amount of urea (No. 26)* decreases, especially in late pregnancy due to increased protein utilization (positive nitrogen balance).
Creatinine (No. 22)* decreases maximum in the 1st - 2nd trimester (its concentration can decrease by almost 1.5 times), which is associated with an increase in the volume of muscle mass of the uterus and fetus. The level of uric acid (No. 27)* is often reduced due to increased blood supply to the kidneys, but even minor renal dysfunction can lead to an increase in this indicator, and this is regarded as symptoms of toxemia.
Lipid metabolism changes significantly during pregnancy (profile No. 53)*. As oxidative processes intensify, there is an increased utilization of cholesterol in the adrenal glands and placenta. This leads to compensatory transient hypercholesterolemia, characterized by an increase in cholesterol and HDL levels. The HDL level remains virtually unchanged. An increase in estrogen levels leads to hypertriglyceridemia, which is facilitated by hypoproteinemia and functional cholestasis. At the same time, fat deposition in the mammary glands and subcutaneous fat increases; this process is also associated with an increase in the transition of carbohydrates to fats due to increased insulin production.
An indicator reflecting the level of endogenous insulin secretion is C-peptide (No. 148)*. Glucose values (No. 16)* may change slightly without reaching the level of hyperglycemia. Since during pregnancy the glomerular filtration rate increases and the permeability of the epithelium of the renal tubules increases, glucosuria (physiological) may periodically be observed. Most often, glucosuria appears during pregnancy 27 - 36 weeks. Features of mineral metabolism in healthy pregnant women compared to non-pregnant women are the retention of sodium, potassium, chlorine (No. 39)*, phosphorus (No. 41)* salts in the body; it is changes in phosphorus levels in the body of a pregnant woman that are associated with an increase in alkaline phosphatase (No. 36) *. This is due to changes during pregnancy in bone tissue and changes in the liver. As you know, during pregnancy the need for calcium salts, which are necessary for the formation of the fetal skeleton, increases, and the mother may experience calcium deficiency (No. 37)*. Hypocalcemia in pregnant women can manifest itself in muscle cramps and spastic phenomena. Increased iron intake during pregnancy can lead to anemia. This condition is characterized by a decrease in iron (No. 48)*, ferritin (No. 51)*, vitamins: B12 (No. 117)*, folic acid (No. 118)*. Changes in the endocrine system
The pituitary gland, especially the anterior lobe, enlarges. Pituitary hormones ACTH (No. 100)*, prolactin (No. 61)* play a large role in changing the metabolic processes of the pregnant woman’s body. Therefore, these hormones may be elevated. The placenta also has hormonal activity. It produces progesterone (No. 63)*, free estriol (No. 134)*, b-hCG (No. 66)*, these hormones are similar in their action to somatotropin (No. 99)*. The thyroid gland also undergoes changes, it enlarges somewhat, and in the first half of pregnancy its hyperfunction is noted. There is an increase in free T4 (No. 55)*, with normal T4 levels (No. 54)*. There is also an increase in the function of the parathyroid glands with a relative increase in parathyroid hormone (No. 102)*. The production of FSH (No. 59)* decreases during pregnancy.
Biochemical analysis: albumin
Maintaining optimal levels of this protein is extremely important for the functioning of the body as a whole. The volume of blood circulating in the body depends on this. In addition, the protein is responsible for regulating osmotic pressure. This indicator changes under the influence of many factors (for example, after eating salty foods). Therefore, its regulation is a very important process. Albumin is also responsible for the transport and storage of many biological compounds and amino acids. When examining your health status, the ALB level is one of the key indicators.
Albumen
Description of the analysis:
Albumin is a protein produced by the liver and is one of the markers for diagnosing its diseases. It is also important in diagnosing kidney diseases.
It is albumin that is the main protein component of blood plasma, in which it performs a number of functions:
- transport – transports fatty acids, metal ions, some vitamins, hormones, cholesterol, drugs (aspirin, a number of antibiotics) with the bloodstream;
- reserve - is a carrier of amino acids, which begin to be consumed if a person is starving or on a diet low in protein;
- maintaining osmotic pressure of the blood - keeps fluid in the bloodstream and does not allow the tissues of our body to swell.
Indications for measuring albumin levels
Measuring albumin levels during diagnosis or treatment may be necessary for doctors of various specialties: gastroenterologists and hepatologists, nephrologists, internists, cardiologists, rheumatologists, oncologists or traumatologists.
Indications for testing in gastroenterology may be:
- vomit;
- diarrhea;
- chronic hepatitis;
- cirrhosis of the liver;
- liver atrophy;
- malabsorption (insufficient absorption of nutrients in the small intestine);
- intestinal obstruction.
In nephrology, analysis is prescribed for:
- nephrotic syndrome;
- diabetic nephropathy.
In oncology, indications for prescription may be:
- multiple myeloma;
- tumor processes.
In rheumatology, the reason for ordering a test may be a suspicion of:
- rheumatoid arthritis;
- systemic lupus erythematosus.
In traumatology, the indications are:
- burns;
- bleeding;
- injuries.
The therapist prescribes an albumin test when:
- general weakness;
- swelling of the limbs;
- seizures caused by calcium deficiency;
- infections;
- dehydration;
- dystrophy;
- anorexia;
- cachexia;
- feverish conditions;
- overhydration.
To cardiologists, a decrease in albumin levels indicates congestive heart failure.
In endocrinology, a drop in the level of this protein may indicate thyrotoxicosis.
Albumin level in blood
Albumin is measured in grams per liter, and the level of this protein in the blood depends primarily on the age of the patient. For adults, the reference values are 35-53 g/l; for elderly people, a decrease to 32-46 g/l is typical. For children under 1 4 years of age, the norm is 28-54 g/l, and for children under two months – 28-44 g/l.
Causes of high or low albumin
Albumin increases most often when the body is dehydrated, often observed in heavy smokers and people who abuse alcohol. In most of the above cases, its level in the blood decreases.
In addition, albumin levels are reduced during pregnancy and breastfeeding. Taking high doses of steroid hormones, combined oral contraceptives and estrogens can reduce the level of albumin in the blood. Low albumin may be due to a genetic defect called analbuminemia.
Preparing for the examination
Preparation for the analysis of albumin levels is the same as for other biochemical blood parameters:
- do not eat at least 8 hours before blood sampling (you can drink water, but not liquids containing sugar);
- do not smoke or drink alcohol for at least 12 hours before the examination;
- avoid physical activity.
The material taken for analysis is venous blood.
Determination method: end point.
Analysis readiness time: 1 business day
Sign up for tests
3.What can affect the content of total protein in the blood?
What can affect the level of total protein in the blood?
Reasons that may affect the content of total protein in the blood:
- Taking certain medications: corticosteroids, estrogens, androgens, growth hormones, or insulin;
- Injury or infection;
- Long bed rest;
- Chronic diseases, especially those that prevent you from eating certain foods;
- Pregnancy.
What's worth knowing?
If you have abnormal globulin levels, you may need additional testing for specific subgroups.
If the liver is damaged
and stops producing protein,
then the protein in the blood remains unchanged for some time.
Liver damage can be seen only after 2 weeks by analyzing the total level of protein in the blood.
Unlike carbohydrates and fats, proteins cannot be stored in the body. They are broken down into amino acids and used to form other proteins, hormones, enzymes and more.
Low albumin levels may predict poor outcome in patients with COVID-19
The COVID-19 pandemic has claimed more than four hundred thousand lives worldwide, and Spain is one of the worst affected countries. At the time of writing this article, there have already been more than 25,000 deaths due to COVID-19 in Spain. The article's authors explain that despite this, little information is available regarding the underlying characteristics and risk factors for patients at risk of hospitalization due to infection. This study included 48 patients admitted with COVID-19.
The scientists explained that it was necessary to identify factors on the basis of which an unfavorable prognosis for a particular patient can be made. The team said many studies show that there is suppression of the immune system during infection. This may be a key factor that leads to the progression of a mild infection to a more severe and ultimately life-threatening condition in the patient. Because inflammation plays a key role, factors that influence inflammation may be important in the progression of the disease.
Albumin is a protein produced in the liver and found in the blood. People with low albumin levels may have liver and kidney problems. Low albumin levels are also seen in patients with malnutrition, severe infection, thyroid disease, and inflammatory bowel disease.
The study involved 52 patients hospitalized due to complications of COVID-19 until March 31, 2020. Of these patients, 48 had severe acute respiratory syndrome due to SARS-CoV-2. They all tested positive for the virus. Data were collected between 15 and 31 March 2021. The aim of the study was to describe the clinical characteristics and epidemiological features of severely and critically ill patients.
Among the 48 patients, 21 were admitted to intensive care and 27 were not. All of these patients were residents of the island of Mallorca in Spain. Their average age was 66 years, and 67% were men. The age distribution was similar among patients. The following conclusions were made:
before hospitalization included fever (all patients), cough (85% of patients), difficulty breathing (76% of patients), diarrhea (42% of patients, and weakness (21%)).
The main reason for hospitalization among patients was low blood oxygen levels (SpO2 below 90%) and the presence of pneumonia in both lungs (94% of cases).
Among all patients, 70% had high blood pressure, 62% had high cholesterol and 30% had heart disease.
Those admitted to the intensive care unit (ICU) had more difficulty breathing.
Acute respiratory syndrome (ARDS) developed in all patients admitted to the ICU.
All 48 participants required oxygen therapy.
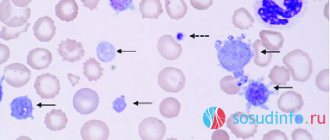
Laboratory tests showed that intensive care unit patients had low lymphocyte counts and low blood albumin levels.
Among patients admitted to the ICU, there was a significant increase in inflammatory markers such as lactate dehydrogenase (LDH), C-reactive protein (CRP), and procalcitonin compared with those not admitted to the ICU.
Lower blood albumin levels were significantly associated with worse outcome and longer hospital stay. The risk of death was also higher among people with lower blood albumin levels.
In red blood cell studies, mean corpuscular volume of red blood cells was lower among patients who died from infection and its complications.
At the end of the study (April 28, 2021), the mortality rate was 21%: 8 patients in intensive care units and 2 in other units died from infection.
At the end of the study, all non-ICU patients were discharged from the hospital. While among the intensive care unit patients, one third remained in hospital at the end of the study (5 in the intensive care unit and 2 transferred to general wards).
Conclusions and implications
People with influenza A (H1N1) and human immunodeficiency virus infection (HIV) also had a poorer outcome if they had lower albumin levels, the paper's authors reported. Among patients with influenza, the need for respiratory support increased with low albumin levels, and among patients with HIV, low albumin levels meant a greater risk of inflammation and atherosclerosis.
This was a relatively small study that showed that certain laboratory parameters may be important in characterizing the severity of illness in patients with COVID-19. “Lower albumin levels were associated with worse outcomes in patients with COVID-19. Albumin may be important because of its association with disease severity and mortality in patients infected with SARS-CoV-2."
The scientists added: “This small case series provides the first steps towards a comprehensive clinical characterization of severe and critical adult patients with COVID-19 in Spain.”
Expert opinion
: Of course, based on such a small study, no final conclusions can be drawn. But now any additional information can adjust the forecasts for patients with COVID-19. Moreover, determination of albumin level is included in the list of standard laboratory tests.
Anemia, hypertension, hypovitaminosis D: are your kidneys okay?
Not many people know, but the kidneys are not only an excretory organ. It is “here” that vitamin D is transformed into its active form. Erythropoietin is synthesized here, which maintains the level of red blood cells. Renin is formed here, which indirectly affects the “width” of the vessels and, thereby, determines the pressure. And kidney disease has many more signs and consequences than is commonly believed.
"Non-standard" and "classic"
Symptoms of kidney disorders, as already noted, are not only about “urine” and lower back pain. After all, they appear exclusively at the time of acute inflammation in the organ.
In other cases, changes can be much more inconspicuous, the identification of which is possible only through screening. A special, distinctive feature of such disorders is resistance to traditional therapy.
Signs may include:
1. Jumps in blood pressure that are difficult to correct.
After all, renal renin activates angiotensin, which sharply constricts blood vessels and increases blood pressure.
Among other things, angiotensin irritates the thirst center in the brain, literally “forcing” you to drink more, thereby increasing the volume of the liquid part of the blood and contributing to an even greater increase in pressure.
And this “pressure” does not decrease after taking “conventional” medications, creating the risk of a critical increase.
2. Persistent anemia (deficiency of red blood cells)
due to a lack of renal erythropoietin, which stimulates the bone marrow to synthesize red blood cells. At the same time, the level of iron, vitamins B12 and B9, the deficiency of which is the main cause of anemia, remains normal.
3. Symptoms of D-deficiency and calcium disorders.
Decreased immunity, distorted immune reactions, caries, osteoporosis, rickets, muscle cramps, weakened memory and concentration, mood instability with a tendency to depression and other symptoms occur against the background of normal levels of total vitamin D and its fractions (25-hydroxyergocalciferol and 25-hydroxycholecalciferol) .
And a decrease in the level of 1,25-dihydroxycholecalciferol (calcitriol), the only active form of vitamin D, which is formed in the kidneys under the influence of parathyroid hormone and has all the effects inherent in the vitamin, can “give away” the renal origin of the symptoms.
Of course, kidney problems can also manifest themselves with more “classical” signs, such as urinary problems, swelling and general weakness. Indeed, with renal failure, toxic metabolic products accumulate in the body, as well as metabolites of drugs and other “harmful” substances.
Simple and affordable
Kidney screening, in addition to a urine test, should also include some blood parameters, including:
- Creatinine and urea are products of protein metabolism, a slight increase in the level of which is acceptable during active physical activity and during fasting. Whereas a significant increase is a sign of developing renal failure;
- Uric acid is a breakdown product of purine bases (DNA, RNA), an increase in which leads to the accumulation of urates and the development of gout. And the reason for the increase may be a violation of the excretory function of the kidneys, as well as a number of serious diseases;
- Albumin is one of the protein fractions synthesized in the liver, which is normally unable to penetrate the kidney filter. Therefore, a lack of albumin in the blood may be an early sign of kidney pathologies. However, such an analysis must be evaluated in combination with other indicators, as well as a blood test (the appearance of protein);
- Clinical blood test with leukocyte formula - helps to identify renal inflammation (which in the early stages may not have clinical signs), as well as a lack of red blood cells (anemia). Which, as already noted, may be a consequence of erythropoietin deficiency.