Among diseases of the biliary tract, the first place belongs to dyskinetic disorders.
Dysfunctions of the biliary tract (previously called dyskinesias) mean disturbances in the motor-evacuation function of the gallbladder, ducts, as well as disturbances in the tone of the sphincter of Oddi. These changes lead to disruption of the process of formation and secretion of bile, and subsequently to its stagnation. Biliary tract dysfunctions are functional disorders lasting more than 3 months. They can be periodic, short-term or protracted, manifesting themselves in the form of pain in the right hypochondrium.
Bile plays an important role in the digestion process. It is needed to “blur” fats into an emulsion. It is then processed by enzymes in the intestines, broken down and absorbed. Bile is an aqueous solution consisting of 70% bile salts (cholic and chenodioxycholic), 22% phospholipids (lecithin), 4% cholesterol, 3% protein and 0.3% from bilirubin. With insufficient amounts of bile acids - lecithin and cholesterol - insoluble cholesterol appears and bile becomes lithogenic. When stagnation occurs in the biliary tract, changes in the composition of bile occur, an inflammatory process develops and a sediment appears in the bile - biliary sludge, which can subsequently lead to the formation of stones.
Causes of biliary tract dysfunction
Dysfunction of the biliary tract Primary dyskinesia of the biliary tract can occur in children due to: uncoordinated work of the sympathetic and parasympathetic nervous system: the tone of the sphincter of Oddi and the gallbladder decreases.
Also, various stresses, improper diet or eating errors (eating large amounts of fatty foods, overeating or irregular meals) lead to the fact that the neuromuscular apparatus of the gallbladder becomes irritated and contracts poorly. Secondary dyskinesia of the biliary tract appears due to: chronic diseases of the digestive system, helminthic infestation; congenital malformations of the biliary tract; endocrine disorders, inflammatory diseases of the digestive system.
Development of pathology
Biliary hypertension is a disease that develops due to improper functionality of the bile ducts and their sphincters.
The outflow of bile is disrupted, causing an increase in pressure inside the biliary tract and obstructed blood flow within systems and organs. Bile duct hypertension is a stable syndrome during which a person’s vascular pressure inside the biliary tract increases to 160/140 mm. rt. pillar If a person begins to use antihypertensive drugs not prescribed by a doctor, then these attempts become ineffective. Consequently, the patient is forced to consult a specialist to identify the causes of difficulty in bile outflow.
As a rule, biliary hypertension appears due to the occurrence of pathological processes in the area of the gallbladder or other factors that impede the full functionality of the bile ducts.
The disease occurs from the following factors:
- From the appearance of tumors localized in the biliary tract, as a result of which the outflow of bile is disrupted. Similarly, these deviations provoke neoplasms of nearby organs, compressing the ducts that carry out the removal of bile.
- Due to calculous cholecystitis or cholelithiasis. This is the formation of hard stones (insoluble) in the hepatobiliary system. As a result, jaundice of mechanical origin appears.
- When parasitic worms enter the bile ducts. Having settled in the human bile ducts, helminths begin to poison the body with toxins and multiply. As a result, they close the lumen of the vessels or organs responsible for the outflow of bile.
- If biliary hypertension is detected in childhood, it is necessary to examine the bile ducts for the presence of abnormal development, characterized by a narrowing of the venous lumen or an altered shape.
Symptoms of biliary tract dysfunction
Clinical manifestations of dysfunctional disorders of the biliary tract are quite wide and can be nonspecific. Complaints are multisymptomatic and usually associated with psychosocial factors. They can be roughly divided into three groups.
Abdominal pain
The hypertensive form of gallbladder dysfunction is characterized by acute paroxysmal, stabbing, short-term compressive pain in the right hypochondrium or around the navel, usually accompanied by nausea, belching or even vomiting, but without a rise in temperature.
The hypotonic form is characterized by aching, pressing, dull pain that becomes constant and is associated with eating, physical activity or emotional stress. There is a bitterness in the mouth and nausea.
Spasm of the sphincter of Oddi in combination with decreased tone of the gallbladder is characterized by dull, aching pain in the abdomen. With insufficiency of the sphincter of Oddi, early pain is characteristic after eating fatty foods; they can be sharp and aching, combined with manifestations of dyspepsia.
Dyspeptic disorders
Nausea, vomiting, belching, heartburn, bitterness in the mouth, a feeling of heaviness in the epigastrium, changes in the nature and frequency of stool are observed. All this is associated with untimely release of bile into the duodenum and impaired digestion of fats, with duodenogastric and gastroesophageal reflux.
Neurological and autonomic disorders
Headache, feeling of a lump in the throat, sweating, drowsiness, fatigue, cardialgia, cold extremities, behavior changes, anxiety, hysteria, decreased learning ability and performance.
Treatment of portal hypertension at the Innovative Vascular Center
In the Innovative Vascular Center, both classical operations to create splenorenal anastomoses and emergency endovascular operations of transjagular portacaval shunting (TIPS) are used to treat portal hypertension.
Endovascular operations are performed on an angiographic complex with the additional use of visualization of the portal vein using ultrasound navigation. Such interventions are performed under local anesthesia with intravenous sedation.
Splenorenal anastomosis operations are performed in intact patients who have suffered bleeding from varicose veins of the esophagus. We perform such interventions under anesthesia through an access in the left side wall of the abdomen with transition to the chest. Such interventions help to avoid the deadly complications of portal hypertension.
Methods for diagnosing biliary tract dysfunction
The abundance and variety of symptoms of dysfunctional disorders of the biliary tract causes difficulties in making a diagnosis, which requires additional examination.
Screening diagnostic methods
Screening diagnostic methods include: biochemical studies of blood serum, ultrasound of the abdominal organs and endoscopy.
Clarifying methods
To clarify the diagnosis, ultrasound is used to determine the function of the gallbladder and sphincter of Oddi, dynamic cholescintigraphy, and ERCP.
Sign up for diagnostics To accurately diagnose the disease, make an appointment with specialists from the Family Doctor network.
Diagnostics
To establish the cause of biliary hypertension or confirm the diagnosis, instrumental methods of examining the patient will be required. The most informative of them are:
- Ultrasound.
- CT scan.
- X-ray contrast research techniques.
- Biopsy.
- Laparoscopy.
Ultrasound of the bile ducts is a non-invasive way to study the retroperitoneal space, using ultrasound radiation that is safe for the patient’s health.
This determines the level of blockage of the bile ducts, the expansion of intra- and extrarenal bile ducts. When a disease with a distal blockage of the bile ducts is detected, dilation of the hepaticocholedochus appears. If no measures are taken, over time the ducts located inside the kidneys expand, increasing the diameter of the gallbladder. A duct larger than 10 mm appears due to the appearance of a tumor (over 50% of cases).
CT scans also allow visualization of organs without interfering with the integrity of the human body. The results of the study make it possible to estimate the size of the emerging tumors and neoplasms, their localization and growth into nearby organs and structures.
X-ray contrast studies involve the introduction of a contrast agent into the body, which brightens the darkened areas of the internal organs. As a result, the damaged areas are clearly displayed on the x-ray, making it possible to assess the ability of the bile ducts to function normally.
Biopsy is a rare research method. In this case, doctors have to remove a small piece of pathological tissue from the body. The procedure is performed under the supervision of specialists using ultrasound equipment. The results of the examination of the obtained tissue make it possible to determine the benign or malignant nature of the neoplasm.
If the methods described above do not help to obtain sufficient information about the causes of the disease, then laparoscopy is performed, which is a surgical intervention. In this case, doctors can examine the damaged areas and at the same time carry out treatment, take biomaterials for further research. Based on the identified pathological disease, repeated surgical treatment is performed.
Treatment methods for biliary tract dysfunction
Treatment of dysfunctional disorders of the biliary tract should be comprehensive and aimed at normalizing the outflow of bile and pancreatic secretion. To do this, it is necessary to normalize the diet and nature of nutrition. Food stimulates the contraction of the gallbladder, so meals should be divided, up to 5 times a day, in small portions, and it is advisable to eat meals at the same time. The diet should be structured so that the first half of the day accounts for 55-60% of its total calorie content. Excluded from the diet: carbonated drinks, rich broths, fatty meats, smoked foods, spicy, fried and canned foods, concentrates. Freshly prepared food in warm boiled, steamed or stewed form is recommended. Therapeutic nutrition is prescribed for at least 1 year, and if the pain syndrome persists for a long time - up to 1.5-2 years.
A special role in the treatment of biliary dyskinesias belongs to choleretic drugs, which are conventionally divided into:
- choleretics that stimulate bile formation by enhancing the functional activity of hepatocytes. These are preparations containing bile: allohol, cholenzyme, lyobil; synthetic drugs: nicodine, oxafenomide, cyclone; preparations of plant origin: corn silk extract, milk thistle extract, artichoke, smoker, flamin, holagol, hofitol, holosas, hepabene, etc.
- cholekinetics that stimulate bile secretion, cause an increase in the tone of the gallbladder, a decrease in the tone of the bile ducts and promote increased flow of bile into the duodenum: magnesium sulfate, sorbitol, xylitol.
To relieve pain, myotropic antispasmodics (halidor, drotaverine, baralgin, mebeverine, etc.) are used. Cholelytic agents (derivatives of deoxycholic acid), which normalize cholesterol production, and hepatoprotective agents, which have a complex effect on the hepatobiliary system (antispasmodic, anti-inflammatory and choleretic), can also be prescribed.
To improve the outflow of bile, it is good to carry out dubazhi according to Demyanov (blind probing), with magnesium sulfate (0.2-0.4 g/kg), mineral water “Magnesium Donat”, 1-2 times a week (for a course of up to 4-8 procedures).
Quite often, dysfunction of the biliary tract is a consequence of neurosis. For this purpose, vegetotropic therapy is indicated. Preference is given to herbal medicines:
- sedatives: valerian root, bromine, motherwort, sage.
- tonic preparations: eleutherococcus extract, tincture of aralia, Chinese lemongrass, freshly brewed tea, etc.
Prevention
Prevention of dysfunctional disorders of the biliary tract consists of prescribing a balanced diet, following a diet, eliminating stress, sanitizing secondary foci of infection, and prescribing dosed physical activity.
Dispensary observation
Children with biliary tract dysfunctions are monitored for a period of 2 years. The child must undergo preventive courses of therapy in the spring-autumn periods and during the period of remission: herbal medicine, hydrotherapy and balneotherapy.
Make an appointment Do not self-medicate. Contact our specialists who will correctly diagnose and prescribe treatment.
Rate how useful the material was
thank you for rating
Types of biliary hypertension
When diagnosing a patient, doctors establish a specific type of billiard hypertension, characterized by the degree of complexity and the presence of complications. Thanks to this data, a specialist can choose the most effective treatment and save a person’s life.
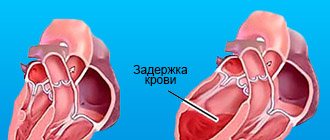
Biliary hypertension is characterized by the prevalence of high blood pressure. This factor contains 2 possible options for the course of the disease: segmental or total.
- Total hypertension implies damage to all vessels of the portal system.
- Segmental is characterized by impaired blood flow in the splenic vein. However, with this course of the disease, the pressure in the portal vein remains normal.
Determined by the location of the venous block:
- Intrahepatic hypertension is the result of blockage of blood flow within the hepatic portal vein.
- Prehepatic - appears due to obstructed venous blood flow in the vessels supplying blood to the liver.
- Posthepatic - occurs due to difficulty in the movement of blood from the liver to the vena cava (inferior).
- Mixed. In this case, several types of biliary hypertension may be observed, complicating the patient’s condition and the prescription of therapy.
By severity:
- The initial stage is determined by a slight disruption of the functionality of the bile ducts.
- Moderate - in this case, the failure and working functionality of the bile ducts is compensated.
- Severe - in this case, an accumulation of fluid appears in the abdominal cavity, which leads to an increase in the size of this area.
- Complicated – provokes the occurrence of renal failure or internal bleeding.
Having examined all these factors, the doctor begins to prescribe optimal therapy to alleviate the patient’s condition and reduce the patient’s susceptibility to complications.
Forecast
Portal hypertension is a complication of underlying liver disease. The disease can often be controlled, and survival depends on the preservation of liver function. The worse the liver performs its functions, the worse the prognosis.
There are higher rates of mortality and morbidity in patients with severe and persistent gastrointestinal bleeding. The mortality rate of patients diagnosed with esophageal varices is 30%.
Patients who have had at least one episode of bleeding due to esophageal varices have an 80% chance of rebleeding within 1 year. In patients with esophageal varices, complications of the immune, cardiovascular and pulmonary systems contribute to approximately 20-45% of deaths.
Complications
The main complications: gastrointestinal bleeding, ascites and hepatic encephalopathy (liver failure, a complex of mental, nervous and muscle disorders).
Splenomegaly often causes anemia, low white blood cell counts, and low platelet counts.
Common complications associated with portal hypertension are aspiration pneumonia, sepsis, renal failure, cardiomyopathy, arrhythmias, and hypotension.
Portal hypertension is a dangerous disease because it can cause bleeding. In many cases, bleeding episodes are considered medical emergencies because the mortality rate from variceal bleeding is about 50%. Esophageal varices are very common in people with advanced cirrhosis, and it is estimated that one in three people with varices will develop bleeding.