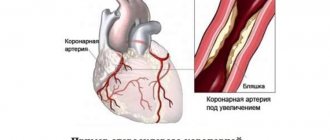
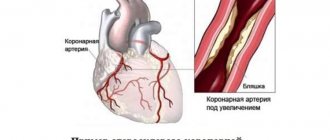
Most cases of angina are associated with a sharp increase in the level of physical or psycho-emotional stress. However, there are exceptions to this rule. Thus, Prinzmetal's angina, also called variant, vasospastic or spontaneous, usually develops in a patient who is at rest. The typical time for symptoms to occur is between midnight and the wee hours of the morning. The pain syndrome is intense, spreading to the head or arms, reminiscent of signs of seizures. It is more often observed in smokers, patients with high cholesterol or blood pressure, but can also occur in healthy people. Thanks to modern diagnostic methods and a thoughtful course of treatment while eliminating bad habits or factors, it is possible to significantly reduce the frequency of attacks and make them less painful.
Causes of Prinzmetal's angina
Coronary artery spasm can occur in the following cases:
- hypothermia of the body;
- smoking;
- symptoms of arterial hypertension;
- stress;
- increased cholesterol levels;
- taking medications that slow blood flow;
- consumption of alcohol and drugs.
The disease is more common in patients aged 50 to 60 years. 5 times more common in men than in women. Smoking and alcohol consumption are recognized as the main risk factors. Less commonly, the pathology develops against the background of vasomotor vascular disorders.
Prevention
Prevention is aimed at eliminating all existing risk factors.
Important:
- Get rid of bad habits. Smoking is especially dangerous.
- Eliminate physical inactivity. A sedentary lifestyle leads to many diseases of the cardiovascular system. Moderate physical activity, in turn, is beneficial for the body. They really prolong life.
- Lose weight (if it is increased).
- Normalize nutrition. To prevent the risk of pathologies of the cardiovascular system, you should constantly introduce fiber-rich vegetables and fruits into your diet, and avoid flour, sweet, fatty and fried foods.
- Constantly monitor your blood pressure and take medications to stabilize it.
- Eliminate the risks of emotional and physical overload.
Our doctors will tell you about all preventive measures.
Important! You should not only adhere to the recommendations of specialists, but also regularly undergo a comprehensive examination by a cardiologist. It will allow you to detect any deviations in a timely manner.
Symptoms of Prinzmetal's angina
The list of characteristic symptoms of vasomotor angina includes:
- pain in the chest at rest, which can be of a different nature - from some discomfort to severe pain radiating to the head or arm;
- feeling of pressure and tightness in the chest;
- attack of nausea;
- sweating;
- dizziness, clouding of consciousness;
- tachycardia, etc.
The duration of the attack ranges from 2 to 20 minutes, and the characteristics of individual episodes are usually similar to each other. Cases of relapse with frequent attacks may be followed by a state of calm for several weeks or months.
Are you experiencing symptoms of Prinzmetal's angina?
Only a doctor can accurately diagnose the disease. Don't delay your consultation - call
Classification (types) of angina
Stable
(angina pectoris) – angina pectoris that occurs in response to physical and/or emotional stress, indicating the functional class (we talked about the classes above).
- exacerbation of angina pectoris, or pre-infarction condition. The pain appears even with minimal exertion and does not stop even after taking Nitroglycerin. The process of thrombus formation occurs, but not sufficiently to cause necrosis of the heart muscle. It is considered an emergency condition and its symptoms are indistinguishable from myocardial infarction, but can lead to it.
Unstable
angina:
- First appeared. A situation when a person who previously had no symptoms of angina pectoris or characteristic pain begins to show its signs.
- Progressive. In a situation where the frequency of attacks and their duration increases, Nitroglycerin helps the patient worse than in previous attacks. Pain occurs in response to an increasingly lower load, that is, the functional class of angina increases.
- Post-infarction. Angina attacks appear within two weeks after a myocardial infarction.
- Spontaneous. Another name for this type of angina is vasospastic, variable. It is this type of angina that is caused not by atherosclerosis of blood vessels (not by their narrowing), but by severe vasospasm. Spontaneous angina has a specific picture: it most often appears in young men; pain does not occur in response to loads or stress, but at any moment; manifests itself as a series of attacks with an interval of 10 minutes to an hour (2-5 attacks)
Microvascular angina (also known as cardiac X syndrome). The peculiarity of this type: pain with ECG signs typical of angina occurs with normal vascular patency (more than 50 percent). Typical for women 40-50 (period of premenopause and menopause) who have neurotic disorders. Doctors have not yet established the exact cause of this type of angina, but they suggest that cardiac X syndrome appears as a result of vasospasm caused by a decrease in estrogen.
Methods for diagnosing the disease
Suspicion of Prinzmetal's angina arises in any case if the patient complains of sharp chest pain at rest or at night. The diagnosis implies that the duration of attacks can range from 30 seconds to 5 minutes, and their number varies up to several dozen within half an hour. In addition, an indirect sign is the subsidence of pain when taking sublingual drugs with a nitrate chemical composition.
The initial assumptions can be confirmed by:
- electrocardiogram in the format of a one-time study or daily monitoring;
- provocative pharmacological tests.
Treatment of Prinzmetal's angina
A course of medication that affects both the symptoms of the disease and its causes can help cope with attacks and reduce their regularity. Clinical recommendations for Prinzmetal angina include:
- taking drugs from the category of calcium antagonists in combination with long-term nitrates;
- anti-alpha adrenergic drugs that prevent coronary artery spasm;
- a course of antioxidant vitamins C and E;
- other medications that promote the natural elasticity of blood vessels and maintain their conductive capacity.
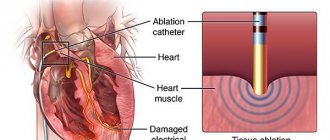
If a conservative course turns out to be ineffective, doctors resort to surgical intervention. More often this is coronary angioplasty with stenting, less often cardiac denervation with plexectomy simultaneously with coronary bypass surgery. A decision may be made to implant an automatic defibrillator or pacemaker.
FAQ
What does Prinzmetal's angina mean?
This is the name of a separate type of angina, the main symptom of which is severe pain during the patient’s rest or night sleep. The main reason is a short-term spasm of the coronary artery, as a result of which the blood flow sharply slows down. But the heart muscle, maintaining the same rhythm of work, is forced to contract even more intensely, which gives a characteristic pain syndrome.
How does Prinzmetal's angina manifest?
It is not easy to miss an attack of the disease: it makes itself felt by a sharp pain in the heart area, which radiates to the head, shoulder or arm. You feel nausea, difficulty breathing due to a feeling of pressure in the chest, dizziness, and a sharp increase in heart rate. Sometimes patients complain of nausea and sweating.
Syndrome X in cardiology (“microvascular angina”)
In approximately 10–20% of patients who undergo diagnostic coronary angiography due to acute or chronic cardiac ischemic syndrome, the coronary arteries are intact. Even if we assume that in some of them the symptoms of ischemia may be due to other cardiac and non-cardiac causes, then at least one out of ten patients with typical angina pectoris does not have hemodynamically significant stenoses of the coronary arteries. The presence of typical angina with unchanged coronary arteries was first described by N. Kemp in 1973 [1]. This syndrome is called “ X(X) syndrome” .
Cardiac syndrome X is a pathological condition characterized by the presence of signs of myocardial ischemia in the absence of atherosclerosis of the coronary arteries and spasm of the epicardial coronary arteries on coronary angiography (signs of myocardial ischemia: typical attacks of angina and ST segment depression ≥ 1.5 mm (0.15 mV) duration more than 1 minute established during 48-hour ECG monitoring). Thus, cardiac syndrome X is diagnosed in patients:
• with typical chest pain;
• with positive stress tests;
• with angiographically normal epicardial coronary arteries and no clinical or angiographic evidence of coronary artery spasm;
• with the absence of systemic arterial hypertension with and without left ventricular hypertrophy, as well as the absence of disturbances in the systolic function of the left ventricle at rest.
In rare cases, patients with syndrome X develop left bundle branch block with subsequent development of dilated cardiomyopathy. It should be noted that in the absence of changes in the coronary arteries during angiography, there is often occlusive pathology of the distal vessels (microvascular angina).
Some authors use the term “microvascular angina,” meaning that patients with typical angina have a normal coronary angiogram and reduced coronary reserve.
Syndrome X is usually classified as one of the clinical forms of coronary artery disease, since the concept of “myocardial ischemia” includes all cases of imbalance in oxygen supply and myocardial demand for it, regardless of the reasons causing it.
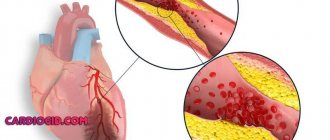
It should be noted that the capabilities of the angiography method in assessing the state of the coronary bed, in particular microvascular, are limited. Therefore, the concept of “angiographically unchanged coronary arteries” is very arbitrary and indicates only the absence of atherosclerotic plaques narrowing the lumen of the vessels in the epicardial coronary arteries. The anatomical features of the small coronary arteries remain “angiographically invisible.” Causes of cardiac syndrome X:
The etiology of cardiac syndrome X remains unclear and only some pathophysiological mechanisms leading to the development of typical clinical and instrumental manifestations of the disease have been established:
• increased sympathetic activation; • endothelial dysfunction; • structural changes at the microcirculation level; • metabolic changes (hyperkalemia, hyperinsulinemia, “oxidative stress”, etc.); • increased sensitivity to intracardiac pain; • chronic inflammation; • increased stiffness of arteries, etc.
There are a number of hypotheses that determine the pathogenesis of syndrome X. According to the first of them, the disease is caused by myocardial ischemia due to functional or anatomical disorders of microcirculation in intramuscular (intramural) prearterioles and arterioles, i.e. in vessels that cannot be visualized by coronary angiography. The second hypothesis assumes the presence of metabolic disorders leading to disruption of the synthesis of energy substrates in the heart muscle. The third hypothesis suggests that syndrome X occurs with increased sensitivity to painful stimuli (decreased pain threshold at the level of the thalamus) from various organs, including the heart.
Despite intensive research over the past 35 years regarding the pathogenesis of coronary syndrome X, many important questions remain unanswered.
Among patients with cardiac syndrome X, middle-aged people, mostly women, predominate. Less than 50% of patients with cardiac syndrome X have typical exertional angina, and the majority have atypical chest pain. Symptoms of cardiac syndrome X:
The main complaint includes episodes of angina-type chest pain that occurs during physical activity or is provoked by cold or emotional stress; with typical irradiation, in some cases the pain is longer lasting than with ischemic heart disease, and is not always relieved by taking nitroglycerin (in most patients the drug worsens the condition). Symptoms accompanying cardiac syndrome X resemble vegetative-vascular dystonia. Cardiac syndrome X is often found in people who are suspicious, with a high level of anxiety, against the background of depressive and phobic disorders. Suspicion of these conditions requires consultation with a psychiatrist. The diagnostic criteria for cardiac syndrome X include: • typical chest pain and significant depression of the ST segment during physical activity (including on the treadmill and bicycle ergometer); • transient ischemic depression of the ST segment ≥ 1.5 mm (0.15 mV) lasting more than 1 minute during 48-hour ECG monitoring; positive dipyridamole test; • positive ergometrine (ergotavin) test, a decrease in cardiac output against its background; • absence of atherosclerosis of the coronary arteries during coronary angiography; • increased lactate content during ischemia when analyzing blood from the coronary sinus area; • ischemic disorders during stress myocardial scintigraphy with 201 Tl.
Syndrome X resembles stable angina. However, clinical manifestations in patients with syndrome X are very variable, and in addition to exertional angina, attacks of resting angina can also be observed.
When diagnosing cardiac syndrome X, the following should also be excluded: • patients with spasm of the coronary arteries (vasospastic angina), • patients in whom non-cardiac causes of chest pain are documented by objective methods, for example:
- musculoskeletal causes (osteochondrosis of the cervical spine, etc.); — neuropsychic causes (anxiety-depressive syndrome, etc.); - gastrointestinal causes (esophageal spasm, gastroesophageal reflux, gastric or duodenal ulcer, cholecystitis, pancreatitis, etc.); - pulmonary causes (pneumonia, tuberculosis in the lungs, pleural overlays, etc.); - latent infections (syphilis) and rheumatological diseases.
Treatment of cardiac syndrome X:
Treatment for the group of patients with syndrome X remains not fully developed. The choice of treatment is often difficult for both treating physicians and the patients themselves. The success of treatment usually depends on the identification of the pathological mechanism of the disease and is ultimately determined by the participation of the patient himself. An integrated approach to the treatment of patients with cardiac syndrome X is often necessary.
There are various approaches to drug treatment: antianginal drugs, ACE inhibitors, angiotensin II receptor antagonists, statins, psychotropic drugs, etc. Antianginal drugs such as calcium channel blockers (nifedipine, diltiazem, verapamil, amlodipine) and β-adrenergic blockers (atenolol, metoprolol , bisoprolol, nebivolol, etc.) are necessary for patients with documented myocardial ischemia or impaired myocardial perfusion. Sublingual nitrates are effective in 50% of patients with cardiac syndrome X. There is evidence regarding the effectiveness of nicorandil, which has a bradycardic effect, the α1-blocker prazosin, L-arginine, ACE inhibitors (perindopril and enalapril), cytoprotectors (trimetazidine).
General advice on changing quality of life and treating risk factors, especially aggressive lipid-lowering therapy with statins (reducing total cholesterol to 4.5 mmol/l, LDL cholesterol less than 2.5 mmol/l), should be considered as vital components of any chosen treatment strategies.
Physical training. With cardiac syndrome X, tolerance to physical activity decreases, physical detraining and inability to perform exercise are observed due to a low pain threshold. Physical training increases the pain threshold, normalizes endothelial function and “delays” the appearance of pain during exercise in this category of patients.
Forecast.
The prognosis of patients with cardiac syndrome “X” is usually favorable. Complications typical for patients with coronary artery disease with stenotic atherosclerosis of the coronary arteries (in particular, myocardial infarction) are extremely rare. Survival with long-term follow-up is 95–97%, but in the majority of patients, repeated attacks of angina over many years have a negative impact on the quality of life. While not associated with increased mortality or an increased risk of cardiovascular “events,” cardiac syndrome X often seriously impairs patients' quality of life and poses a significant burden to the health care system. It must be emphasized that the prognosis is favorable in the absence of endothelial dysfunction. In these cases, the patient should be informed about the benign course of the disease. When excluding patients with left bundle branch block and patients with secondary microvascular angina due to serious systemic diseases such as amyloidosis or multiple myeloma, the prognosis of patients with cardiac syndrome X is favorable both in terms of survival and preservation of left ventricular function, but in some patients clinical manifestations of the disease persist for quite a long time.