On average, 7-10% of Russians have chronic heart failure (CHF), 4.5% suffer from clinical symptoms of heart failure that reduce quality of life and ability to work, and among people over 65 years of age, half of patients with cardiovascular diseases have symptoms of CHF, and These numbers are increasing every year.
Heart failure is a syndrome caused by abnormal structure and decreased function of the heart. It can be the outcome of diseases such as arterial hypertension, coronary heart disease, heart defects, arrhythmias, kidney and thyroid diseases, cardiomyopathies, hereditary or as a result of infections, intoxications, metabolic and other disorders.
Description of the disease
Angina pectoris, or angina pectoris, a chronic disease of the cardiovascular system, is characterized by chest pain during physical or gastronomic stress, in stressful conditions, and sudden hypothermia. This differs from another form - angina at rest. Pressing, squeezing or burning pain occurs due to the fact that the heart muscle cells are in a state of severe oxygen deficiency (ischemia).
Pain in angina pectoris quickly decreases and disappears almost immediately after a person puts a Nitroglycerin tablet under the tongue or stops doing any physical work. This is the main difference between “angina” pain and others.
Angina pectoris is considered the most common type of coronary heart disease and is classified under ICD code I20.8.
According to the World Health Organization (WHO), approximately 300,000,000 people worldwide suffer from angina. The average age of onset of the disease is 45-50 years. The male to female ratio is 2.5:1. However, this only applies to premenopausal women. After menopause, this figure is compared with men. There is a very specific explanation for this fact.
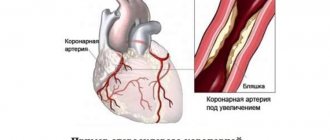
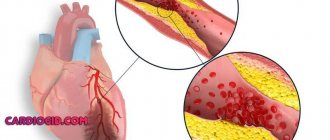
The main cause of angina pectoris is the deterioration of blood flow through the vessels that supply the heart muscle (coronary arteries) due to atherosclerosis. It occurs due to the fact that cholesterol, namely the so-called “bad” variety (low and very low density lipoproteins), is deposited in the walls of blood vessels. Female sex hormones (estrogens) have the ability to reduce the level of this fraction, which reduces the degree of formation of atherosclerotic plaque. And with the onset of menopause, the content of protective hormones in a woman’s blood sharply decreases, which increases cholesterol levels and, accordingly, the rate of development of pathology.
If angina pectoris is not recognized and treated in time, it can lead to myocardial infarction, the number one killer of all diseases.
Degree of disease development
Depending on the speed of development, the disease can be of two types:
- Acute
- develops over several hours or even minutes. In acute left ventricular failure, as a rule, cardiac asthma occurs, which is quickly complicated by pulmonary edema. It is also possible to develop cardiogenic shock, which is characterized by failure of not only the left ventricle, but also the left atrium. Acute right ventricular failure is characterized by stagnation of blood in the systemic circulation. Often occurs against the background of decompensated chronic heart failure. - Chronic
– develops over a longer period of time (up to several years). The severity of the clinical picture largely depends on the underlying disease that affected the cardiac dysfunction.
It is important to classify heart failure according to the form of the disease:
- Myocardial
– with this type, the myocardium is affected, causing the heart muscle to lose the ability to contract normally. The disease is determined by a disorder of both systolic and diastolic function of the heart. - Overload
- as a result of increased load on the organ, the heart muscle gradually weakens. This form of heart failure develops with heart defects that cause a disorder in the normal flow of blood. - Combined
- heart failure develops against the background of increased load on the myocardium and its damage under the influence of various factors.
Make an appointment with a specialist, without queues, at a convenient time
+7
Sign up
Symptoms and signs
The main symptoms that determine exertional angina are attacks of heaviness in the chest, as well as burning or squeezing pain. These sensations can occur when a person is running, working out in the gym, or even just walking up the stairs.
The pain goes away if the load stops or the person takes Nitroglycerin in the form of a tablet/spray. This point is very important, it distinguishes more dangerous conditions - heart attack and unstable form of angina from this disease, since in them the pain is not relieved by Nitroglycerin.
Angina pain is characterized by specific irradiation - return to other parts of the body. This is mainly the lower jaw, neck, left arm and shoulder blade, and upper abdomen. Moreover, the place where the pain is applied is often felt much more strongly, and discomfort in the heart may go unnoticed. I often met patients who for a long time mistook attacks of angina for toothache and unsuccessfully underwent treatment for “pulpitis” or “periodontitis” at the dentist.
In addition to physical work, pain can “overtake” a person under other circumstances. Depending on the factor provoking a painful attack, the following clinical forms of angina pectoris are distinguished:
- Early morning - exacerbation appears at approximately 5-6 o'clock in the morning. Associated with increased blood viscosity and an increase in the amount of cortisol and adrenaline. They cause increased heart rate and hypertension.
- Angina after eating - a large meal redistributes blood flow in favor of the digestive organs. As a result, the oxygen supply to the heart deteriorates.
- Supine angina - when a person lies down, the volume load on his heart increases, which provokes increased work of the organ and, as a result, an increase in its need for oxygenation.
- Cold - at low ambient temperatures, the superficial blood vessels of the skin narrow, which forces the heart to work harder.
- Tobacco – components of cigarette smoke, including nicotine, increase heart rate, constrict blood vessels and thicken the blood.
- Angina after stress – stress stimulates the release of adrenaline and cortisol into the blood.
- Static – when a person bends over to, for example, put on shoes, pressure increases inside the chest. This, in turn, increases the volume load on the heart in the same way as supine angina occurs.
In some groups of patients, the clinical course of angina has its own characteristics. These include:
- elderly people - approximately 50% of people over 65 years of age experience not pain, but sudden difficulty breathing (shortness of breath);
- women - in females, due to the predominance of the emotional component during an attack, in addition to the pain associated with angina pectoris, neurotic pain develops as a result of vasospasm. I often have to accept female patients in whom it is difficult to determine the severity of angina pectoris only by symptoms and to distinguish it from other forms of ischemia;
- diabetics – due to the long course of diabetes mellitus, nerve endings are damaged, including those that conduct pain impulses. Therefore, I often meet such patients with hidden or asymptomatic angina.
Prices for consultation and appointment with a cardiologist
| Name | Price |
| Blood pressure measurement | 60,00 |
| Consultation after MRI/MSCT | 540,00 |
| Initial consultation with a pulmonologist | 1800,00 |
| Initial appointment with a cardiologist (consultation) | 1800,00 |
| Initial appointment with a rheumatologist | 1800,00 |
| Repeated consultation with a pulmonologist | 960,00 |
| Repeated appointment with a cardiologist | 960,00 |
| Repeated appointment with a rheumatologist | 960,00 |
| Preoperative examination by a cardiologist (doctor’s appointment, ECG, interpretation) | 2460,00 |
| ECG interpretation | 600,00 |
| Taking an ECG | 360,00 |
| 24-hour blood pressure monitoring | 2400,00 |
| 24-hour Holter ECG monitoring | 3000,00 |
| ECG with stress | 1950,00 |
Diagnostics
In order to make a differential diagnosis, i.e. To distinguish ischemic pain from non-ischemic pain based on symptoms, I use specially developed criteria, including 3 main signs:
- classic attacks of angina pectoris,
- their appearance during physical work,
- weakening and disappearance after taking Nitroglycerin tablet/spray or stopping the load.
The presence of all three criteria is typical for typical angina, and two for atypical angina. If the patient has only one criterion, then the diagnosis is doubtful.
I also conduct a general examination of the patient, during which symptoms of heart failure can be identified:
- swelling of the legs,
- thickening of the fingertips,
- bluish lip color,
- swollen veins in the neck,
- enlarged and painful liver.
I especially often notice such signs in the elderly. In patients with heart defects, various sounds can be heard on auscultation. It is mandatory to measure blood pressure, since the vast majority of people with angina have hypertension.
To confirm or refute the diagnosis, I prescribe an additional examination, which includes:
- Blood analysis. Almost all people with coronary heart disease have elevated cholesterol levels. Therefore, I always prescribe a lipid profile (cholesterol fraction) determination. Also, following the protocol, you need to check the glucose concentration and do a general blood and urine test.
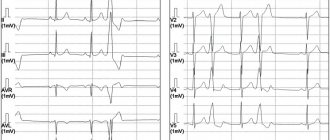
- Electrocardiography (ECG) is the main diagnostic method for suspected angina. The main symptom of the disease is a decrease (depression) in the ST segment. Sometimes a negative T wave is recorded. However, often these changes cannot be detected at rest, i.e. when there is no pain. Therefore, I prescribe additional ECG studies for my patients.
- Electrocardiography with stress. Of all such tests, I prefer bicycle ergometry (riding an exercise bike) and treadmill test (walking or running on a treadmill). If, after a certain time, symptoms of angina appear and the ECG shows typical signs (ST segment depression greater than 1 mm and a negative T wave), the test is considered positive. It is worth noting that such studies are not suitable for everyone. For example, I do not perform them on patients over 85 years of age and people with severe heart failure (III-IV functional class).
- Daily ECG monitoring. In cases where physical tests are not possible or the results obtained are questionable, it is advisable to conduct a Holter study. It is also a very good way to detect silent myocardial ischemia. Most often, I prescribe Holter ECG to patients with diabetes.
- Echocardiography (Echo-CG, ultrasound of the heart). The method allows you to check the ability of an organ to pump blood, assess the condition of the valves, the degree of wall thickening, and the presence of intracardiac blood clots.
- Transesophageal electrical stimulation of the heart (TEC) - the procedure is as follows. A flexible probe with an electrode is inserted through the patient's nose and installed in the esophagus in the projection closest to the heart. Then weak signals are sent, causing an attack of angina. At the same time, an ECG film is removed to record specific changes. I also perform this method on patients for whom physical tests are contraindicated.
- Myocardial scintigraphy - with this method I study the intensity of blood supply to the myocardium. For this, a radioactive drug is used (I mainly use thallium-201 and technetium-99-m), which is administered intravenously to the patient. Then he begins to perform moderate physical activity, after which an image is displayed on a special device. The degree of intensity of the glow is used to judge the blood circulation of different parts of the heart. I resort to myocardial scintigraphy if the patient has serious arrhythmias (bundle branch blocks, repeated ventricular extrasystoles), in which it is impossible to see specific changes on the cardiogram. This method is of little information for women, since breast tissue accumulates a significant part of the pharmaceutical drug.
- Coronary angiography is the gold standard for diagnosing coronary heart disease, allowing a reliable diagnosis. It can also be used to determine whether surgery is necessary.
Clinical forms
- Congestive left ventricular failure is characteristic of mitral disease and severe forms of coronary artery disease - especially in patients with arterial hypertension. Increased pressure in the pulmonary veins helps fill the left ventricle and maintain sufficient cardiac output. At the same time, congestive changes in the lungs disrupt the function of external respiration and are the main factor aggravating the patient’s condition with this form of heart failure. Manifestations: shortness of breath, orthopnea, auscultatory signs of pulmonary congestion (dry rales below the level of the shoulder blades, migrating moist rales) and radiological, cardiac asthma and pulmonary edema, secondary pulmonary hypertension, tachycardia.
- Left ventricular failure is characteristic of aortic disease (see), coronary artery disease, and arterial hypertension. Manifestations: cerebrovascular insufficiency (dizziness, darkening of the eyes, fainting), coronary insufficiency, sphygmographic and echocardiographic signs of low output. In severe cases, Cheyne-Stokes breathing, alternating pulse (rarely), presystolic gallop rhythm (pathological IV tone), and clinical manifestations of congestive left ventricular failure are possible. In the terminal stage, right ventricular failure may occur.
- Congestive right ventricular failure is characteristic of mitral and tricuspid disease, constrictive pericarditis. Usually associated with congestive left ventricular failure. Manifestations: swelling of the neck veins, high venous pressure, acrocyanosis, enlarged liver, subicterus, edema - cavitary and peripheral.
- Right ventricular ejection failure is characteristic of pulmonary artery stenosis and pulmonary hypertension. It is diagnosed mainly radiographically (depleted peripheral pulmonary vascular pattern). Other signs of this form may be detected: shortness of breath at a strictly defined threshold level of physical activity, right ventricular hypertrophy - palpation, then ECG signs of the “pressure load” type (high I wave and decreased T wave in the right precordial leads). In especially severe cases, gray coloration of the skin.
- Dystrophic form. As a rule, end-stage right ventricular failure. Options: a) cachectic; b) edematous-dystrophic with dystrophic changes in the skin (thinning, shine, smoothness of the pattern, flabbiness), edema - widespread or limited mobile, hypoalbuminemia, in the most severe cases - anasarca; c) uncorrectable salt depletion.
In some cases, changes in the heart itself (cardiomegaly, atriomegaly, atrial fibrillation) come to the fore, which allows us to speak of a “central” form of heart failure. As special forms with specific mechanisms of circulatory disorders and manifestations, HF is considered in “blue” congenital defects with insufficient blood flow in the pulmonary circle and unreduced or excessive in the large circle, with cor pulmonale, thyrotoxicosis, anemia, arteriovenous anastomosis, cirrhosis of the liver, as well as arrhythmogenic SN.
Patients may develop “passive adaptation” from childhood (low body weight and height, poor physical development, sharply reduced physical activity, infantilism). The listed forms of CH occur in various combinations; often it is possible to isolate only the leading form.
Canadian classification
To determine the severity of symptoms of angina pectoris, the Canadian Society of Cardiology has developed a special classification in the form of a table, which includes the following functional classes of angina pectoris:
Functional class 1
When performing normal physical activity for a person, he feels good. Pain only appears during intense and prolonged work, such as weightlifting or long-distance running.
Functional class 2
Pain occurs even during normal walking, when a person walks more than 200 meters. Also, angina pectoris develops if the patient climbs stairs above the 2nd floor, goes outside in very cold weather, or overeats.
Functional class 3
The attack begins when walking from 100 to 200 meters, or when climbing to the 2nd floor.
Functional class 4
Doing any physical work causes pain. An attack can develop even in a completely calm state.
Functional classification of pulmonary hypertension
| Class I | There is no restriction on physical activity. Ordinary physical activity does not cause shortness of breath, weakness, chest pain, or dizziness |
| Class II | some decrease in physical activity. Ordinary physical activity is accompanied by shortness of breath, weakness, chest pain, dizziness |
| Class III | severe limitation of physical activity. Little physical activity causes shortness of breath, weakness, chest pain, dizziness |
| Class IV | inability to perform any physical activity without the above clinical symptoms. Shortness of breath or weakness may be present even at rest, discomfort increases with minimal exertion |
Treatment
Before starting treatment, I need to assess the risk, i.e. the likelihood of the patient developing complications in the future (myocardial infarction and death). This is necessary to choose treatment tactics.
To do this, I pay attention to the following parameters:
- Results of tests with physical activity (the time of performing the exercise, after which the patient has an attack);
- echocardiography indicators, namely the adequacy of the pumping function of the heart;
- glow intensity on myocardial scintigraphy;
- the prevalence of atherosclerosis of the coronary arteries and the degree of narrowing of their lumen.
If the patient is at low or medium risk, then I limit myself to drug therapy. And if he is at high risk, then he needs more aggressive treatment of angina pectoris in the form of surgery.
The Braunwald Guide for the treatment of cardiac diseases, the most authoritative publication, recommends the use of the following medications for angina pectoris:
- Beta-blockers (Bisoprolol, Metoprolol) - reduce the pulse rate and slow down the conduction of nerve impulses, thereby reducing the myocardial need for oxygen. In addition, due to an increase in the period of relaxation (diastole) of the heart muscle, its blood circulation improves.
- Slow calcium channel antagonists (Diltiazem, Verapamil) have a similar mechanism of action. I use them in case of intolerance to beta-blockers or if there are contraindications to them.
- Antiplatelet drugs are necessary to prevent the formation of blood clots in the arteries, which lead to a heart attack. First, I prescribe Acetylsalicylic acid, and if the patient has a stomach or duodenal ulcer, then Clopidogrel.
- Statins (Atorvastatin, Rosuvastatin) - reduce the concentration of cholesterol in the blood, thereby slowing down the process of formation of atherosclerotic plaque.
- ACE inhibitors (Perindopril, Lisinopril) - these medications are needed by patients who, in addition to angina, suffer from chronic heart failure or diabetes.
- Blockers of If-channels of sinus node cells (Ivabradine) are so-called pulse-lowering drugs. I use them when the patient has a very fast pulse (more than 100).
This scheme allows me to achieve clinical improvement in the form of cessation of pain in some patients. If attacks persist with the selected therapy, then I add nitrates (Nitroglycerin). These drugs relax the smooth muscle walls of the coronary arteries, which leads to their expansion and increased blood flow to the myocardium.
However, these drugs must be handled very carefully, since if they are not taken correctly, tolerance (addiction) quickly develops, and their therapeutic effect is reduced several times. Therefore, I always recommend that my patients take nitrates only when an attack begins, or no more than 2 times a day, and so that the interval between doses is at least 12 hours.
If drug treatment is unsuccessful, or if the patient has a high cardiovascular risk, surgery is performed.
There are 2 main types of operations:
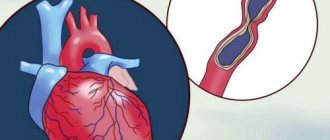
- Stenting, or percutaneous coronary intervention (PCI);
- coronary artery bypass grafting (CABG)
The essence of PCI is the introduction of a special metal stent into the vessel, which improves its patency. The operation is performed under local anesthesia. Access is through the femoral artery. PCI is performed when stenosis in one vessel is more severe than 50%.
When performing CABG, a connection is created between the aorta and the coronary artery to bypass the narrowed vessels. CABG is an open abdominal operation with general anesthesia (anesthesia) and opening of the chest. This method is justified if several arteries are affected or stenting is not possible.
Lifestyle requirements
In order for drug and surgical treatment to have maximum effect, I recommend that my patients adhere to a certain lifestyle, which includes several aspects:
- bad habits – it is advisable to limit alcoholic drinks (to about 300 ml of wine per week). Smoking is strictly prohibited;
- diet - reducing the consumption of foods rich in saturated fats (meat, milk, butter) and increasing foods with a predominant content of omega-3.6 fatty acids (vegetables, fish, vegetable oil). The diet must include fruits, nuts, and cereals;
- regular moderate physical activity or exercise therapy - aerobic exercises are preferable, such as swimming, running, cycling;
- body weight control is achieved by strict adherence to the previous 2 points.
Chronic heart failure
The data on chronic heart failure (CHF) that have accumulated in recent years have led to the need for a unified approach to the diagnosis and treatment of this pathology, which in turn has contributed to the emergence of a number of advisory documents. Over the past 5 years alone, authoritative cardiological associations have already published several revisions of their recommendations for the diagnosis and treatment of CHF: American College of Cardiology / American Heart Association (2001, 2005), European Heart Association (2001, 2005), VNOK (1993, draft, 2006 ).
Ideas about CHF have been constantly changing over the past decades. Moreover, not only the issues of pathogenesis, diagnosis and treatment, but also approaches to determining
CHF.
Thus, in the European recommendations of 2001
CHF is presented as “
a pathophysiological syndrome
in which, as a result of a particular disease of the cardiovascular system, a decrease in pumping function occurs, which leads to an imbalance between the hemodynamic need of the body and the capabilities of the heart.”
According to the domestic recommendations of the All-Russian Scientific and Cultural Organization (2003),
CHF is also “
a syndrome
that occurs when a person has systolic and/or diastolic dysfunction, accompanied by chronic hyperactivation of neurohormonal systems and clinically manifested by shortness of breath, weakness, palpitations, limitation of physical activity, pathological fluid retention in the body "
At the same time, the modern neurohormonal theory of the pathogenesis of heart failure has convincingly shown that, regardless of the initial causes, its development occurs on a single pathophysiological basis. These provisions allowed GFCI experts to put forward a proposal that CHF is a separate nosological unit, and in the draft national recommendations of GFCI and OSCH of 2006
.
CHF is proposed to be understood as “ a disease with a complex of characteristic symptoms (shortness of breath, fatigue and decreased physical activity, edema, etc.), which are associated with inadequate perfusion of organs and tissues at rest or during exercise and often with fluid retention in the body.”
Active studies of any individual component of the pathogenesis of CHF in different years have led to the emergence of different pathophysiological definitions and, accordingly, models of its development (Table 1).
| Most common etiological factors CHF remains coronary heart disease (CHD), in particular myocardial infarction (MI), angina pectoris and ischemic cardiomyopathy, which is primarily associated with a decrease in global systolic function of the left ventricle (LV). The second and third positions are occupied by dilated cardiomyopathy and rheumatic heart defects, respectively. At the same time, in people over 70 years of age, hypertension and associated disturbances in myocardial diastolic relaxation play a leading role in the development of CHF, along with ischemic heart disease. Diagnostics CHF is built on three main pillars: 1) clinical manifestations, among which the most common are shortness of breath, fatigue and decreased performance, peripheral edema; 2) objective signs of heart damage, that is, evidence of the connection of clinical signs specifically with cardiac and not other pathology; 3) ex juvantibus effect. In this case, the presence of the first two criteria is mandatory. However, diagnosing CHF is quite a difficult task, since clinical signs, like objective data, are very nonspecific and can occur in a wide variety of diseases. At the same time, they should be constantly remembered, since it is they who, already at the first communication between the doctor and the patient, allow one to suspect the presence of CHF. The most common symptoms and objective data characteristic of CHF are presented in table. 2.
|
Doctor's advice
In addition to the generally accepted lifestyle interventions described above, I strongly encourage my patients to monitor their blood pressure and take appropriate medications regularly.
If a person suffers from diabetes, he should regularly check his blood glucose levels and periodically take a glycated hemoglobin test. This is important, since diabetes can worsen the course of angina several times and lead to complications.
Also, if you cannot eat fish often, you can take fish oil in the form of dietary supplements. They are available in any pharmacy. To argue for the benefits of fish oil, I would like to give the example of Japan, a country where heart disease rates are extremely low, and fish as a food product occupies the top positions.
Clinical case
I would like to provide an example from personal experience.
A 52-year-old man visited his local physician for an outpatient appointment with complaints of pressing pain in the heart area, which occurs when climbing the stairs to the 3rd floor and goes away a few minutes after resting. I began to notice the appearance of these pains about a month ago. Suffering from type 2 diabetes mellitus and hypertension. She takes Metformin 1000 mg 2 times a day and Lisinopril 10 mg 1 time a day. The therapist referred him to a cardiologist, who prescribed an ECG and VEM (veloergometry). At rest, when deciphering the ECG, there were no changes. When performing a VEM, an ECG revealed ST segment depression of 2 mm. The patient was sent to the cardiology hospital for further examination with a diagnosis of coronary artery disease, angina pectoris FC 2. Coronary angiography was performed, which revealed 70% stenosis of the right coronary artery. The damage to the remaining vessels was not critical, so the decision was made to install a stent. Drug therapy was also prescribed (Acetylsalicylic acid, Rosuvastatin, Bisoprolol). The patient noted a significant improvement in his condition in the form of cessation of pain attacks. Upon discharge, recommendations for lifestyle modifications were given.
In conclusion, I would like to note that angina pectoris is a serious disease that requires due attention from both the doctor and the patient. Ignoring attacks of pain can lead to an unfavorable prognosis in the form of myocardial infarction, disability and death. However, timely diagnosis and proper treatment can improve the quality and increase the life expectancy of a person.
Make an appointment with a cardiologist
The best cardiologists at the private Multidisciplinary Medical Center in Moscow invite patients with any type of cardiac dysfunction to diagnose and treat them. If signs of heart failure are detected, the patient is prescribed a comprehensive examination, after which experienced specialists will monitor the disease through medication and other effective therapy.
You can make an appointment with a cardiologist for a fee by phone or using the feedback form. Check the price of initial and repeat appointments on the clinic’s website. If the patient’s condition is acute, cardiologists will see him without an appointment at any time of arrival at our center.
Moscow, st. Krasnodarskaya, house. 52, bldg. 2
+7
We work on weekdays and weekends from 8.00 to 21.00