In medicine, a post-infarction condition is usually called a complex of symptoms and complications that appear in patients who have had a heart attack. This period is dangerous because there is a danger of a second heart attack, which does not always end well. The most common complications of the post-infarction state are heart failure and Dressler's syndrome.
Post-infarction angina
Attacks of angina pectoris that occur in the period from 24 hours to 14 days after myocardial infarction are classified as a post-infarction state. According to statistics, post-infarction angina occurs in about 25% of patients who survive a heart attack. Attacks of angina pectoris are expressed in pain behind the sternum, radiating to the shoulder blade, neck, jaw or left arm. These pains are very strong, nitroglycerin does not help relieve them, and the patient often has to take strong analgesics to get rid of the pain.
An attack of angina pectoris can occur with little physical exertion or even at rest, and the patient’s blood pressure may increase or decrease. In some cases, the attack passes without pain and is accompanied by arrhythmia.
The danger of post-infarction angina is that it can provoke a new myocardial infarction.
Dressler syndrome
This complication develops 2-6 weeks after myocardial infarction due to necrotic damage to the tissue of the heart muscle. Toxic decomposition products entering the patient’s blood cause an autoimmune reaction in the body. Dressler syndrome is characterized by the following symptoms:
- Sharp or pressing pain in the chest, often radiating to the shoulder or neck.
- Sometimes there is an increase in background temperature.
- The patient complains of severe weakness.
- Painful sensations may appear in the area where the lungs are located.
- A dry cough with blood may occur.
- Rashes appear on the skin.
- There is numbness in the left hand.
- Upon visual examination, the left side of the chest appears swollen.
Dressler's syndrome can occur as pleurisy, pericarditis or polyarthritis. This is a typical variant for this condition. The atypical form is expressed as cardiobrachial syndrome, which is indicated by high temperature and changes in blood tests.
Laser therapy for post-infarction conditions
Treatment includes 10-15 sessions of laser therapy procedures, which are carried out every other day or every day. You can repeat the course of laser treatment after 30 days, then 2-4 times a year with ECG monitoring.
The course of treatment with the Rikta device makes it possible to gradually reduce the dose of calcium antagonists and nitro drugs.
You can reduce the dose of blockers starting from the 7th session. During the first course of therapy, it is not advisable to completely stop taking medications.
During the course of laser treatment, it is recommended to drink vitamins A, C and E, group B three times a day before meals. It is possible to take coronary anti-atherosclerotic drugs such as 600 mg of thioctacid before meals, as well as cocarboxylase and ATP, but these drugs must be prescribed by the attending physician.
Additional materials:
- Read more about diseases of the circulatory system
- Laser medicine in angiology (for vascular diseases)
- Laser medicine in cardiology
- Laser therapy in the treatment of hypertension
- Laser therapy during the rehabilitation period after a stroke
In 1956, an American internist (Dressler W., 1890–1969) first summarized the experience of observing patients with the so-called. post-infarction syndrome, which included arthralgia, fever, increased ESR, pleurisy and a key symptom - effusion pericarditis. The first manifestations of post-infarction syndrome were usually recorded at 2-3 weeks after the development of acute myocardial infarction (MI).
It was Dressler who managed to identify the characteristic features of post-infarction syndrome - a tendency to relapse, as well as a relatively benign course of damage to the serous membranes, including the pericardium. Subsequently, he clarified some clinical variants of post-infarction syndrome, and also demonstrated the possibility of a combination of pericarditis and pleurisy with pneumonitis. 3 years after the first publication, Dressler presented the results of a survey of 44 patients with post-infarction syndrome.
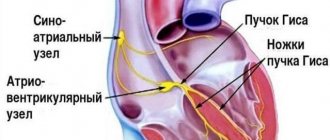
Dressler has repeatedly described other variants of pericarditis, including recurrent ones. In particular, he was able to trace the fate of a patient with a pericardial effusion that persisted for 15 years, but did not lead to the formation of a constrictive lesion of the pericardium. Much of Dressler's work is devoted to ventricular cardiac arrhythmias, including evaluating the results of pacemaker implantation. In response to the intervention, some patients, as after acute MI, developed pericarditis and pleurisy with persistent chest pain. In addition, Dressler identified the phenomenon of the appearance of a normal QRS complex, which in his opinion was of supraventricular origin, against the background of paroxysm of ventricular tachycardia. Often, after the occurrence of this phenomenon, the attack of ventricular tachycardia spontaneously stopped.
After Dressler described the post-infarction syndrome, its individual manifestations were clarified in detail. As a rule, Dressler's syndrome develops after acute MI with a significant area of myocardial damage, especially in the anterior, lower localization, as well as damage to the right ventricle. Post-infarction syndrome is more often observed in the complicated course of acute myocardial infarction. Restrictive lesions of the pericardium as an outcome of Dressler's syndrome are very rare, but they are possible, especially with massive hemorrhagic effusion. In the classic “Essays on Emergency Cardiology” (1973) Chazov E.I. reports the story of a patient in whom severe hemorrhagic pericarditis, which appeared 2 months after acute MI, required surgical intervention. The leading clinical syndrome was biventricular heart failure (central venous pressure reached 270–90 mm Hg), and persistent low-grade fever was also noted. An X-ray examination of the chest revealed significant enlargement of the heart, which required differentiation from a left ventricular aneurysm. Pleuro- and pericardiocentesis were accompanied by a temporary improvement in the condition: exercise tolerance increased, the effectiveness of constantly used drugs that stimulated the inotropic function of the myocardium, as well as diuretics, increased. However, later severe pericardial constriction developed, requiring pericardiotomy. It should be emphasized that the features of acute MI in this patient corresponded to the characteristics of Dressler's syndrome (extensive area of myocardial damage, localization in the anteroseptal region, on the anterior, posterior and lateral walls) and were complemented by a complicated (cardiogenic shock) course.
The combination of pericarditis and pleurisy with markers of a “nonspecific” inflammatory response (low-grade fever or fever, increased ESR, leukocytosis, arthralgia, in which joint deformations are not typical) became the basis for discussing the autoimmune component of the pathogenesis of Dressler's syndrome. This was also evidenced by the possibility of the development of pericarditis during acute MI, in which the subepicardial layers of the myocardium remained intact and, therefore, direct “reactive” involvement of the pericardium (similar to pleurisy in lobar pneumonia) was excluded. In addition, there is a clear tendency to relapse and frequent regression when prescribed nonsteroidal anti-inflammatory drugs (NSAIDs).
Attempts have been made repeatedly to identify the triggering factors of post-infarction syndrome. Its connection with latent viral infections has not been confirmed. The role of components of necrotic myocardium resorbed into the blood seems more convincing. That is why post-infarction syndrome is more often observed after acute extensive infarctions followed by massive necrosis of the affected areas. In patients with post-infarction Dressler syndrome, complement activation and an increase in the serum titer of circulating immune complexes, including those containing antibodies to cardiomyocytes and their individual components (actin, myosin), are recorded. However, specific antibodies to pericardial structures in Dressler syndrome could not be identified.
Rare components of post-infarction syndrome that substantiate its autoimmune genesis are: combination with anemia, thrombocytopenia and bronchial asthma, as well as described by A.V. Sumarokov. and Aprosina Z.G. (1972) autoimmune hepatitis. The onset of signs of the latter (skin itching, hepatomegaly, hyperbilirubinemia, hyperproteinemia due to hypergammaglobulinemia, increased serum levels of IgA, IgG and IgM) was noted in a 60-year-old patient 1.5 years after acute MI and coincided with the development of exudative pleurisy, pericarditis, and also pneumonitis. In addition, a persistent increase in ESR was recorded. A combination of Dressler's syndrome with acute febrile dermatosis and inflammatory bowel disease (so-called Sweet's syndrome) is also known.
Already in the first report, pointing out the predominantly hemorrhagic nature of the pericardial exudate, Dressler suggested the influence of the irritating effect of blood components on the pericardium on the formation of post-infarction syndrome. In this regard, a provoking role in the development of Dressler's syndrome was attributed to anticoagulants, including warfarin, since the appearance of hemopericardium was explained by the action of these drugs. This assumption was subsequently refuted; moreover, today there is no doubt that timely treatment of acute MI, including with the use of anticoagulants, makes it possible to prevent Dressler's syndrome. The lack of influence of anticoagulants on the pathogenesis of post-infarction syndrome was already obvious when analyzing data from the patient population described by Dressler himself. Despite the fact that more than a quarter of the patients did not receive these drugs at all, the author, nevertheless, observed characteristic clinical signs in them - effusion pericarditis, pleurisy, fever and arthralgia.
In the first two decades since its description, Dressler's syndrome was found in 3–4% of patients with acute MI. Currently, the patient has symptoms such as increasing heart failure, a rapid increase in the shadow of the heart due to pericardial effusion, recorded by radiography, against the background of pleural and joint pain, a rise in body temperature in a patient who suffered an acute MI at least 2 weeks ago, according to - still always requires exclusion of Dressler's syndrome. ECG changes typical for acute pericarditis in Dressler's syndrome are recorded relatively rarely. It is believed that a certain proportion of patients in whom benign pericarditis was accidentally detected, the cause of which could not be determined, suffer from Dressler's syndrome, having previously suffered a subclinical and therefore not timely recognized acute MI.
Currently, Dressler's syndrome has become a casuistically rare diagnosis, which is associated primarily with a radical improvement in the quality of treatment of acute MI, which currently makes it possible to minimize the area of myocardial necrosis. The possibility of early restoration of myocardial perfusion, for example, using thrombolysis and angioplasty, has led to a significant reduction in the incidence of complications of acute myocardial infarction, including Dressler's syndrome. Thus, the results of an analysis of data from large groups of patients with acute myocardial infarction indicate that with successfully performed thrombolysis, post-infarction syndrome does not form at all; its development always confirms that it was not possible to restore the patency of the occluded coronary artery. Other drugs used to treat coronary heart disease, primarily β-blockers and statins, appear to contribute to a reduction in the incidence of post-infarction syndrome. Dressler's syndrome is extremely rarely observed in patients who have suffered pulmonary embolism. Its formation, as a rule, reflects the development of acute right ventricular MI.
It is well known that the clinical manifestations of Dressler syndrome almost always respond to treatment with NSAIDs and corticosteroids. However, the use of these drugs for the treatment of post-infarction syndrome is not recommended, since in the first four weeks after the development of acute MI they can disrupt the repair processes of the heart muscle, promoting the formation of aneurysms and increasing the risk of heart rupture, as well as increasing coronary vascular resistance. Acetylsalicylic acid in large (650 mg every 4 hours) doses is considered preferable for the treatment of Dressler's syndrome.
More than 50 years after its first description, Dressler's syndrome remains important as a relatively rare, yet possible complication of acute myocardial infarction. Timely recognition of Dressler's syndrome and its adequate treatment, obviously implying not only the use of acetylsalicylic acid, but also other drugs used for the secondary prevention of cardiovascular complications (β-blockers, statins, clopidogrel), and currently remain relevant, since they contribute to increasing the active life expectancy of patients.