Frederick's syndrome is a deadly organic pathology. Its essence lies in the disruption of the normal conduction of electrical impulses through cardiac structures.
In the presence of disease, the signal is not transported from the atria to the ventricles, circulating in the upper chambers in isolation, which leads to a significant drop in myocardial contractility.
The result of the pathological process is fatal arrhythmias, which sooner or later are very likely to lead to cardiac arrest, cardiogenic shock or heart attack.
Third-party emergencies are also possible, which are caused by a violation of the general blood flow.
Recovery is expected in theory, but in reality there are no options other than surgical treatment, and surgical intervention does not guarantee complete management of the condition.
Development mechanism
The essence of the process becomes clear if we take into account the anatomical and physiological features of the work of cardiac structures.
Normally, the functional activity of the heart is constant and is determined by the generation of an electrical impulse by a special accumulation of myocyte cells. It is called the sinus node or natural pacemaker.
Next, the excitation is transmitted through special bundles from the atria to the ventricles. There is an alternating, complete contraction of the myocardium along its entire length.
This phenomenon is accompanied by an intense release of blood into both circles: small and large, providing both adequate gas exchange and nutrition of all tissues and systems.
Frederick's syndrome is characterized by disruption of the normal conduction of cardiac structures. The changes correspond to a complete blockade.
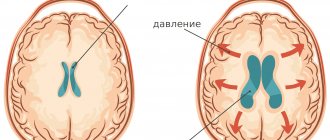
The electrical impulse does not reach the ventricles, but moves in a circle in the atria, which leads to the emergence of a dual mechanism:
- The upper chambers begin to contract chaotically or correctly, but excessively quickly.
- The lower ones generate their own signal, becoming excited.
Hence the fluttering, fibrillation. More often the process affects all cardiac formations, and therefore is the most severe.
The result is a drop in myocardial contractility, disruption of the normal rhythm, decreased blood output, changes in the nature of hemodynamics, hypoxia, insufficiency of work of both the muscular organ itself and remote systems.
This generalized nature of the deviations explains why the mortality rate of the condition is at the average level of 96-98%.
How does the syndrome develop?
When Frederick's syndrome develops, the atria begin to contract voluntarily, and not when it is really needed. This pathological process is called atrial fibrillation. Sometimes it is replaced by fluttering, in which a regular but too frequent rhythm is observed. In addition, blood circulation inside the heart is disrupted.
Due to fibrillation, electrical impulses from the atria move into the ventricles along conductive channels. When Frederick's syndrome occurs, this movement of signals stops completely. This process is atrioventricular block.
Due to the blockage, the ventricles of the heart do not receive impulses, so foci are formed in them, which themselves produce electrical signals. This condition is physiological, as it is intended to prevent cardiac arrest. The ventricular rhythm replaces the necessary contractions, but their frequency is significantly less than normal.
The heart ventricles contract slowly, the amount of blood pumped becomes less and less, and as a result, the cells do not receive enough oxygen. Due to these processes, a person develops symptoms of Frederick's syndrome.
Causes
The described phenomenon is never primary; it is always secondary in origin to one or another disease. The pathological factors for the development of Frederick's syndrome are as follows.
Disorders of the functional activity of the thyroid gland
It can be called hypothyroidism, that is, insufficient production of specific hormones. But that's an understatement.
Deficiency in itself does not entail a violation of conductive capacity; such syndromes are formed as a result of subsequent pathologies. Myxedema occurs against the background of hypothyroidism.
This is a complex deviation on the part of the whole organism, it is characterized by total dysfunction of the body. The elasticity of the dermal integument decreases, the activity of the heart, liver, and kidneys is disrupted.
The proliferation of so-called “fast” cells (skin, hair, nails) decreases, and general swelling occurs. The quality of life drops significantly. The picture is crowned by the presence of dangerous arrhythmias.
If treatment is not started promptly, Frederick's syndrome will put an end to the history.
Coronary heart disease or ischemic heart disease
Develops as a result of a heart attack, coronary insufficiency, trauma, tumors and atherosclerosis.
The essence of the pathological process lies in the malnutrition of the muscle layer. Gradually, little by little, it undergoes degeneration and is replaced by scar tissue.
Terrible complications, such as dangerous arrhythmias, begin in a relatively late period, when recovery becomes impossible by any means.
Treatment is supportive and does not guarantee the absence of lethal consequences. The ideal option is therapy at an early stage, when the chances of stabilizing the condition are still high.
Lung cancer in any phase
It manifests itself most clearly from the position of cardiac structures at stages 3-4, when the tumor reaches sufficient size on the one hand (compression of the chest organs occurs), on the other, active decay of neoplasia and poisoning of the body occurs, the load on the heart increases significantly.
The prognosis of Frederick's syndrome of this etiology depends on the prospects of the cancer itself.
If the neoplasm and metastases to regional lymph nodes are eliminated, there is a chance for a long and relatively healthy life without significant limitations. But, as a rule, at stage 3, especially stage 4, the chances of such an outcome are small, if not ghostly.
Myocardial infarction
IHD crowns itself, becoming its natural outcome. Avalanche-like death of cardiac structures develops when a certain critical mass is reached due to circulatory disorders at the local level.
Recovery and its prospects depend on the extent of the lesion. The larger the changes, the more tissue is scarred and, accordingly, the weaker the contractility of the myocardium.
Frederick's syndrome develops as a result of disturbances in electrical activity, as well as destruction of conductive structures.
Coronary insufficiency
It exists in the form of unstable angina (so named for its ability to progress, leading to a fatal outcome in a relatively early period) or as acute cell death (necrosis).
The first inevitably turns into the second, it’s a matter of time. The duration of deviations is indefinitely long.
It is impossible to predict anything, but against the background of gradual destruction of the conductive tracts and gross fusion of dead tissue, Frederick's syndrome develops in 5-10%.
Inflammatory lesions of cardiac structures
Myocarditis, endocarditis, pericarditis. They are accompanied by severe symptoms, which makes diagnosis relatively simple and quick.
In this case, recovery is carried out strictly in a hospital setting, in order to avoid fatal complications.
Diseases are of infectious or autoimmune origin.
With an aggressive course of the process or a late start of therapy (usually both), destruction of cardiac structures occurs, similar to infarction or more severe. The result is sclerotic changes, conduction disturbances.
Cardiomyopathy
Decreased functional activity of the muscle layer of the organ. It is rarely primary; genetic abnormalities or anomalies of the perinatal period are possible.
More often, this is the development of disorders during life that are difficult to treat even in the early stages. It is possible to maintain and stabilize the condition; there are no radical ways.
Rheumatism
Inflammation and subsequent destruction of the heart of an autoimmune nature. The rate of progression depends on the initial data: the patient’s health status, the strength of the immune response, and others.
Congenital and acquired heart defects
They arise as a result of genetic pathologies, spontaneous phenotypic disorders, incorrect, dangerous lifestyle, past infectious and other diseases.
Surgical treatment is aimed at restoring the anatomical integrity and activity of the muscular organ.
Collagenoses
Diseases associated with deviations in the regenerative ability of connective tissue. There are several such collagenoses; which one develops must be assessed based on diagnostic results.
Causes are eliminated gradually during the diagnostic process. Data for pathology are not always present. Then an idiopathic form of Frederick's syndrome with an unknown origin is stated.
Treatment methods
If Frederick's syndrome is identified during the patient's diagnosis, treatment is prescribed, which has several goals. First of all, it is important to prevent the unexpected occurrence of death due to serious cardiac dysfunction. Then it is necessary to alleviate the patient’s condition by eliminating the symptoms of the pathology and prevent the onset of heart failure.
Treatment of the syndrome includes therapeutic and medicinal methods. The first method assumes that patients must adhere to the basic principles of dietary nutrition and refrain from excessive physical activity. If possible, doctors stop medications that worsen heart block. Such medications are drugs against arrhythmia, calcium antagonists and others.
Drug treatment is used to eliminate the factors that led to the development of complete heart block. Also, taking medications is necessary to improve the patient’s condition and eliminate Frederick’s syndrome.
If during the diagnostic process a 3rd degree blockade is detected, accompanied by ventricular fibrillation, then surgical intervention is required. Its goal is to restore impulse conduction.
During surgery, single-chamber ventricular pacing may be used. During this procedure, two electrodes are inserted into the ventricle, which stimulate the myocardium and cause it to contract. If the ventricle begins to contract unnecessarily, its stimulation will be immediately blocked.
The attending physician decides which treatment method to choose based on the results of the patient’s examination. The prognosis after therapy depends on how timely it was carried out, the severity of the development of the syndrome, and how old the patient is. If surgery is not performed in severe cases, the life expectancy of a person is about 2 years.
Risk factors
There are so-called risk factors that do not directly cause the onset of pathological changes, but actively push the body to the line:
- Genetic predisposition. Heredity plays an important role. As was said, some of the deviations are transmitted as a result of disorders of intrauterine development, others - as a result of a fundamental change during the process of embryogenesis.
- Frequent inflammatory and infectious diseases of one kind or another.
- Long-term or improper use of heart medications, antihypertensive drugs, psychotropics, antibiotics, progestin contraceptives.
- Metabolic disorders of generalized type.
Etiology and pathogenesis
The human heart is a unique organ that works according to the strictest physiological laws. Some cardiac pathologies disrupt its functioning and rhythm, which leads to hypoxia of organs and tissues.
With Frederick's syndrome, the functioning of the atria is disrupted, arrhythmia develops, nerve impulses cease to be conducted into the ventricles, and the myocardium contracts frequently and irregularly. There are no organic heart lesions.
Popular articles What does the diagnosis of diffuse changes in the myocardium mean?
The ventricles begin to independently generate nerve impulses. Pathological foci appear in the atrioventricular node of the ventricles, which produce excitatory signals. The ventricular rhythm is started, protecting against cardiac arrest and preventing the death of a person. Gradually, the heart rate decreases to 40-60 beats per minute. Compensatory contraction of the ventricles occurs more slowly than in healthy people. Systemic blood flow slows down, hypoxia develops, the consequences of which are dangerous to human life.
Severe cardiac diseases lead to the development of Frederick's syndrome:
- Cardiac ischemia,
- Post-infarction sclerosis of the heart muscle,
- Acute coronary insufficiency,
- Inflammatory diseases of the myocardium,
- Heart defects
- Rheumatic carditis,
- Pronounced vagotonia,
- Connective tissue diseases
- Syphilitic myocarditis.
Various surgical interventions on the heart lead to the development of Frederick's syndrome. Drug intoxication is a common cause of pathology. Typically, poisoning of the body is caused by cardiac glycosides, β-blockers, slow calcium channel blockers, antiarrhythmics, and lithium salts.
Idiopathic fibrosis and sclerosis of the myocardium leads to dystrophy and dysfunction of the heart muscle. Cardiomyocytes that generate electrical activity are replaced by connective tissue cells.
Clinical symptoms
Manifestations depend on the duration of the pathological process, the presence of concomitant diseases, age, physical characteristics of the patient and other factors.
The basis of the picture is the following features:
- Swelling of the lower extremities. Based on the severity of pathological changes, we can talk about one intensity or another.
In the early stages, provided that there are no associated pathologies, everything is limited to a slight thickening of the tissue in the ankle area.
There are always two reasons: an increase in circulating blood volumes with the general ineffectiveness of the hemodynamic model of a person suffering from Frederick syndrome, as well as disruption of the excretory system, as a result of the evacuation of fluid from the body.
- Dizziness. The intensity varies. Total impossibility of orientation in space also occurs in the acute period. This usually indicates the onset of an emergency. For example, a stroke or advanced stages of encephalopathy.
- Cephalgia. The pain is localized in the occipital region, parietal lobe. They have a stable, aching or squeezing character. They develop regularly, in paroxysms. Each episode lasts from a couple of minutes to hours and even days.
- Bradycardia. The hallmark of Frederick's syndrome. As a result of a decrease in myocardial contractility due to lack of stimulation, a slowdown in the pulse rate is observed. Sometimes to critical levels: 30-40 beats per minute. Against the background of current bradycardia, disturbances of a different kind are observed. Fibrillation or fluttering, as already mentioned.
In combination, the intense work of the atria and the chaotic activity of the ventricles creates a bright picture on the ECG, but nonspecific. Analytical work is required to make a diagnosis.
- Dyspnea. In the early stages of Frederick's syndrome, in a state of intense physical activity, and then in complete rest. The latter option leads to disability, significantly reduces the patient’s quality of life, and makes it impossible not only to work, but also to care for oneself at home.
- Weakness. Intense, to the point of inability to work normally or perform daily duties.
- Chest pain. Feeling of heaviness, pressure. Episodes of arrhythmias last for several hours, less often than a day. Recovery is carried out using specialized drugs, unless there are contraindications.
Also possible: nausea, vomiting, disturbances in the normal functioning of the liver, gall bladder, secondary encephalopathy with weakening of mnestic and cognitive functions, behavioral disorders (increasing phenomena of vascular dementia), constipation, diarrhea, flatulence.
All this is the result of insufficient supply of oxygen and nutrients to the organs.
ECG and other examination methods
A diagnosis can be made based on the characteristic signs on. These include:
- absence of atrial waves;
- frequent and low f or F waves (they are larger and less frequent);
- QRS complexes from the lower part of the atrioventricular node are narrow, and from the myocardium of the ventricles themselves - deformed and wide, frequency no more than 40 - 60 per minute;
- the distances between the atrial waves and ventricular complexes are equal;
- The rhythm of contractions of the atria and ventricles does not coincide.
To clarify the diagnosis and assess the severity of the syndrome, it is indicated to carry out.
Additionally, an ultrasound of the heart is prescribed to determine the cause of the rhythm disturbance and study the viability of the myocardium.
Diagnostics
Examination of prospective patients is carried out by cardiologists. Specialized surgeons are involved as necessary.
The activities are:
- Oral questioning of a person regarding his complaints, collection of anamnestic data to objectify symptoms, building an understandable further scheme.
- Measurement of blood pressure (usually slightly deviates from the norm in one direction or another), heart rate (severe bradycardia with an irregular rhythm).
- Auscultation (dull, chaotic tones).
- Electrocardiography. The main technique identifies a group of nonspecific traits that are subject to a thorough comprehensive assessment.
- Echocardiography. Allows you to determine the root cause of the pathological condition, and also identify organic disorders that arose after the onset of Frederick's syndrome. There can be many of these. Defects are acquired relatively quickly, within 1-2 years.
- Daily monitoring is prescribed as necessary. It makes it possible to dynamically assess the functional activity of the heart and identify the slightest disturbances in the pulse indicator.
Other studies are used less frequently. Usually one cardiography is enough. Additional techniques are aimed at verifying and assessing the extent of the problem and acquired complications.
Prevention
Doctors do not name any specific measures to prevent the development of Frederick's syndrome. This condition occurs due to various heart pathologies. To avoid problems with the functioning of this organ, people should adhere to the basic principles of a healthy lifestyle.
The following is recommended:
- Exercise. It is worth remembering that physical activity should be moderate. Under no circumstances should you overload your heart.
- Eat properly. The condition of blood vessels depends on the foods consumed, the failure of which negatively affects the activity of the heart.
- Stop smoking and drinking alcohol. Bad habits adversely affect the body's condition, causing oxygen starvation and intoxication.
- Visit a cardiologist annually for a preventative heart examination. This is the most important measure, only thanks to which it is possible to detect heart disease in a timely manner and safely get rid of it.
Thus, Frederick's syndrome is a serious pathological condition that indicates a disturbance in the functioning of the heart and leads to serious consequences. A person’s future life depends on the timely detection and treatment of the disease.
Frederick's syndrome on ECG
- The occurrence of extrasystoles (they fit unevenly into the graph).
- Low heart rate (from 30 to 60, not higher).
- The rhythm may be correct, but more often it turns out to be the other way around (RR).
- Complete disappearance of P peaks, their replacement by F-waves of a sawtooth nature.
- The QRS complex may widen.
The signs of Frederick's syndrome on the cardiogram, as was said, correspond to a complex arrhythmia, but it is only possible to say that this is it with serious analytical work.
Attention:
To make a diagnosis, considerable training in the field of cardiology is required, otherwise errors are likely.
Symptoms
A decrease in the pumping function of the heart and hypoxia of the brain determine the clinical picture of Frederick's syndrome. Patients experience weakness, dizziness, darkening of the eyes, shortness of breath, palpitations, interruptions in heart function, exercise intolerance, drowsiness, transient sensations of confusion, cardialgia, rare pulse, cyanosis, convulsions. Pauses in the work of the heart are clinically manifested by attacks accompanied by loss of consciousness.
The above clinical signs are nonspecific. They occur in almost any severe cardiac pathology. Therefore, to make a diagnosis it is necessary to undergo a complete medical examination.
Treatment
Therapy is strictly surgical. On the one hand, the origin factors themselves cannot be corrected (scars, myocardial hypertrophy, etc.), on the other hand, the disorder of the conduction system itself is anatomically irreversible. Therefore, there are no alternatives to radical intervention.
At the same time, we can only talk about the ineffectiveness of drug correction.
Indeed, drugs are not capable of changing the situation. But to carry out an operation without careful preparation is not only unprofessional, but also downright stupid, since the risks are too high: the patient may not survive the implantation of a pacemaker.
Urgently, without preparation, a radical technique is indicated only in the case of an acute emergency condition.
During the planned period, antiarrhythmic drugs, antihypertensive medications, cardioprotectors are prescribed, and, as needed, potassium and magnesium supplements.
Specific names, as well as combinations, are selected by specialists; independent use is unacceptable.
Attention:
Cardiac glycosides are not used.
The essence of the operation is the implantation of a pacemaker. It saves lives, but not always.
Creating an additional pathway makes it possible to eliminate arrhythmia or significantly smooth out its symptoms. The pathology is too dangerous.
Effective or conditionally effective treatment is possible only in the early stages. In this case, a good result is the extension of the patient’s life by at least several years.
Features of therapy
Treatment of Brugada syndrome is actively discussed, experts propose approaches to prescribing medications based on clinical experience and the results of their use in patients with pathology of the electrical activity of the heart, but to this day no effective drug method has been found for the prevention of ventricular arrhythmias and sudden death.
Patients in whom ECG phenomena are provoked by tests with the introduction of a sodium channel blocker, but there are no symptoms at rest, and there are no cases of sudden death in the family, need observation.
Medicines
Drug therapy consists of prescribing class IA antiarrhythmic drugs - Quinidine, Amiodarone, Disopyramide. It is worth noting that the drugs Novocainamide, Aymalin, Flecainide, belonging to class I, cause blockade of sodium channels and, accordingly, symptoms of Brugada syndrome, so they should be avoided. They provoke arrhythmia, and therefore Flecainide, Procainamide, Propafenone are contraindicated.
Quinidine is usually prescribed in small dosages (300-600 mg), is able to prevent episodes of ventricular tachycardia, and can be used in patients with a discharged defibrillator as an additional means of preventing sudden death.
Isoproterenol is considered effective, acting on beta-adrenergic receptors of the heart, which can be combined with Quinidine. This drug can help reduce the ST segment to the baseline and is applicable in pediatric practice. A new drug that “returns” the ST segment to its normal position is Phosphodiesterase.
It has been shown that many antiarrhythmic drugs cause blockade of sodium channels in cardiomyocytes, so it would be logical to assume that those that do not have such an effect - Diltiazem, Bretyllium - would be safer, but studies of their effectiveness have not yet been conducted.
Antiarrhythmic therapy is effective only in 60% of patients; in the rest, it is not possible to achieve a safe state only with the help of medications, and there is a need to correct the electrical activity of the heart using special devices.
Surgical intervention
The most effective way to prevent sudden death is the installation of a cardioverter-defibrillator, which is needed if:
- There are symptoms of SB;
- The course of the pathology is asymptomatic, but provocation causes ventricular fibrillation;
- When tested, the Brugada phenomenon type 1 occurs, and among relatives there have been cases of unexplained death at a young age.
According to world statistics, SB occurs much more often than it appears in the diagnoses of cardiologists. The low detection rate can be explained by a lack of vigilance on the part of doctors and the lack of convincing diagnostic criteria. Based on this, all patients with characteristic ECG changes, unexplained fainting, and an unfavorable family history of sudden death among young people need a thorough examination with ECG, Holter monitoring, and pharmacological tests. Relatives in families where there have already been cases of sudden death of young people also require increased attention.
Popular articles What does upper and lower pressure mean: what does it show, decoding
The study of Brugada syndrome continues, and to obtain high results, a sufficient number of observations is necessary, so experts are interested in identifying as many patients as possible in different countries.
To study pathology, a special International Brugada Syndrome Foundation has been created, where all persons suspected of this disease can be consulted free of charge and in absentia. If the diagnosis is confirmed, the patient will be included in a single list of patients who may in the future be subjected to genetic research in order to clarify the hereditary mechanisms of the development of the pathology.
Possible complications
Possible consequences of the pathological process:
- Cardiogenic shock. A total disorder of cardiac function develops against the background of conduction disturbances, especially often. The lethality of the process is almost one hundred percent, regardless of the form.
- Heart attack. Necrosis of cardiomyocytes and scarring of affected areas.
- Heart failure. It is not accompanied by preliminary symptoms and occurs suddenly. Almost always lead to death due to the unpreparedness of the patient and his loved ones for such a scenario.
- Vascular dementia. Accompanied by signs inherent in Alzheimer's disease. It is potentially reversible at the first stage.
- Stroke.
- Multiple organ failure or dysfunction of individual systems.
Signs of early ventricular repolarization syndrome
Premature ventricular repolarization syndrome is characterized primarily by changes in the electrocardiogram (ECG). Some patients experience various symptoms of cardiovascular disorders, while others completely lack clinical signs of the disease, the person is and feels absolutely healthy (about 8–10% of all cases). Violation of the repolarization process on the ECG in a child or adult is reflected in the following main changes:
- The ST segment rises above the isoline.
- There is a downward-facing convexity on the ST segment.
- There is an increased amplitude of the R wave, in parallel with a decrease in the S wave or its disappearance.
- The J point (the point at the transition of the S segment to the QRS complex) is located above the isoline, in the interval of the descending limb of the R wave.
- The QRS complex is widened.
- At the interval of the descending knee of the R wave there is a J wave, visually resembling a notch.
Types of ECG changes
Based on the changes detected on the electrocardiogram, the syndrome is divided into three types, each of which is characterized by its own degree of risk of complications. The classification is as follows:
- First type: signs of the disease are observed in a healthy person, in the chest leads studied in the lateral plane with an ECG (the likelihood of complications developing is low).
- Second type: localization of signs of the syndrome - inferolateral and inferior ECG leads (the likelihood of complications is increased).
- Third type: signs are recorded in all ECG leads, the risk of complications is the highest.
When playing sports for at least 4 hours a week, the ECG shows signs of an increase in the volume of the heart chambers and an increase in the tone of the vagus nerve. Such changes are not symptoms of pathology and do not require additional examinations. During pregnancy, an isolated form of the disease (without affecting the mother’s cardiac activity) does not in any way affect the development of the fetus and the process of gestation.
Manifestations of pathology
Clinical signs of early ventricular repolarization are detected only in the form of the disease with disturbances in the functioning of the cardiovascular system. The syndrome is accompanied by:
- Various types of arrhythmia (ventricular extrasystole, tachyarrhythmia - supraventricular and other forms, ventricular fibrillation, accompanied by loss of consciousness, stopping pulse and breathing, etc.).
- Fainting (loss of consciousness).
- Diastolic or systolic dysfunction of the heart, hemodynamic disorders caused by it - hypertensive crisis, pulmonary edema, cardiogenic shock, shortness of breath.
- Tachycardial, hyperamphotonic, vagotonic, dystrophic syndromes (especially in childhood or adolescence), caused by the influence of humoral factors on the hypothalamic-pituitary system.
Forecast
Prognostic assessments depend on the moment of initiation of therapy, health status, age, body weight, concomitant pathologies and other factors.
By installing a pacemaker, it is possible to improve the likely outcome quite significantly.
If mortality without therapy is 96% or higher, after implantation the figure drops to 25-30% or less; if in addition there are no risk factors, and there are many positive prognostic factors, the likelihood of a long and high-quality life is maximum.
A negative factor that neutralizes all the benefits of radical treatment is the presence of fainting and syncope in the clinical picture. This is a sign of cerebral ischemia. Such patients most often die within 2-4 years.
Pathology Clinic
The peculiarity of the disease is that the signs of atrial fibrillation disappear against the background of transverse heart block. This makes it difficult to make a correct diagnosis. Patients do not have a feeling of rapid heartbeat, rhythm interruptions, but appear (loss of consciousness).
The insidiousness of Frederick's syndrome is that during the blockade the rhythm of contractions slows down, so a false impression is created that the condition is improving. Good health can remain for a long time.
But later, as the ventricular myocardium loses its ability to maintain rhythm, the patient’s condition deteriorates sharply. At a pulse rate of 20 to 30 contractions per minute, cerebral hypoxia develops, which can be fatal if there is a long pause between contractions.
Watch the video about atrioventricular block and its degree: