For some reason, this type of heart rhythm disorder is often called incorrectly. “Sine ary and even “sinusoidal” - all kinds of distortions of the name are allowed by people who are looking for information about it. Here we will dwell in detail on the features of this type of heart rhythm disturbances.
Snoring, apnea, insomnia or other problems? Contact the Sleep Medicine Center at the Rehabilitation Clinic in Khamovniki. We will definitely help you! Ask questions and sign up for a consultation by phone.
Causes of sinus arrhythmia
Physiological sinus arrhythmia is very common in healthy people. It is a kind of manifestation of the normal function of a healthy heart.
The human heart is sensitive to changes in the functioning of the body and signals from the nervous system. So, during physical activity, the heart rate increases, and during rest it returns to the usual 60 - 80 beats per minute. The breathing phase also affects the heart rate. On inhalation they become less frequent, on exhalation they become more frequent. Such increases and decreases, in principle, can be characterized as physiological sinus arrhythmia.
In children and adolescents, sometimes there is another variant: unequal time intervals between “adjacent” heart contractions. This is a manifestation of the immaturity of the nervous system. As you grow older, it goes away on its own.
In addition, athletes and people in good physical condition may have a heart rate less than 60 beats per minute. This phenomenon is called physiological bradycardia, and it can also be called a type of “normal” sinus arrhythmia.
Pathological sinus arrhythmia occurs as a consequence of diseases, including:
- Heart diseases (more details in the article “What are arrhythmias”)
- Nervous system dysfunction (neuroses, vegetative-vascular dystonia)
- Endocrine diseases (thyroid dysfunction, diabetes mellitus)
- Diseases of the respiratory system (bronchial asthma)
- Intoxications (medicines, alcohol)
- Electrolyte disturbances.
Sometimes the cause of sinus arrhythmia cannot be identified.
Causes of heart rhythm disturbances
The organic type manifests itself against the background of several pathologies:
- myocardial infarction;
- myocardial dystrophy;
- myocarditis;
- cardiosclerosis.
The listed diseases provoke degenerative changes in the sinus node and conduction disturbances in the myocardium.
The extracardiac form of bradycardia is the result of neuroses, increased intracranial pressure or compression of the carotid sinus by clothing.
Toxic lesions develop when a person comes into contact with hazardous chemicals. Bradycardia of this type often develops against the background of the patient’s professional activity.
Drug-induced bradycardia occurs when a person violates the prescribed dosage of a drug or long-term use of medications with a pronounced effect on the heart rate.
Symptoms and complications of sinus arrhythmia
Physiological arrhythmia usually does not cause any discomfort.
Pathological sinus arrhythmia can manifest itself in different ways. It most often occurs in three forms: sinus bradycardia, sinus tachycardia and extrasystole.
Sinus bradycardia is characterized by a heart rate below 60 beats per minute at rest. Patients with bradycardia complain of attacks of weakness, dizziness, and pain in the heart area. Periodically they experience fainting. These symptoms can be observed either all together or separately - each patient has individual manifestations.
Rare heartbeats lead to the fact that an insufficient amount of blood reaches the organs and tissues, they lack oxygen and nutrients, and this negatively affects their vital functions. Frequent complications of sinus bradycardia include strokes, heart failure, and myocardial infarction. This condition can even cause cardiac arrest (called sudden cardiac death).
Sinus tachycardia is an increase in heart rate, usually up to 120, sometimes up to 150 beats per minute. Its signs are a feeling of rapid heartbeat, squeezing pain in the chest (sometimes), attacks of weakness and dizziness, and loss of consciousness.
With sinus tachycardia, the heart fills with less blood than necessary. Blood pressure decreases, organs, and first of all, the heart muscle itself, are insufficiently supplied with blood. Sinus tachycardia is often complicated by the development of myocardial infarction and heart failure.
Pathological sinus extrasystole usually manifests itself as a feeling of a sinking heart followed by a strong shock in the chest, or attacks of increased heartbeat. They may be accompanied by pain in the heart area, pale skin, a feeling of anxiety, and lack of air.
Sometimes all these violations are not felt by a person at all.
To treat or not to treat sinus bradycardia?
It depends on its cause in the first place.
If bradycardia occurs while taking medications, then after they are discontinued, as a rule, it disappears and does not require treatment. If bradycardia is persistent, persists for a long time and is poorly tolerated by the patient, then it certainly requires correction, up to the implantation of a pacemaker. In case of mild sinus bradycardia, you can get by with taking Zelenin drops (20-30 drops in warm water 1-2-3 times a day, as needed). Your doctor will provide information on how to treat bradycardia in your case.
You can make an appointment by phone or through the appointment form on the New Hospital website
Treatment of sinus arrhythmia
Physiological sinus arrhythmia does not require treatment. Occasionally, herbal sedatives are prescribed.
To get rid of pathological sinus arrhythmia, you need to cure the disease from which it is a consequence.
For sinus tachycardia, treatment is predominantly medicinal and aimed at reducing the heart rate. For this purpose, sedatives (motherwort, valerian), beta-blockers, etc. are used.
Treatment of sinus bradycardia is aimed at increasing the heart rate. For this purpose, both medications (sympathomimetics, anticholinergics) and implantation of an electrical pacemaker are used for severe bradycardia that threatens the patient’s life.
Sinus extrasystole is treated with antiarrhythmic drugs.
Diagnosis of sinus bradycardia
It is carried out by recording an ECG and Holter ECG monitoring throughout the day.
Diagnosing sinus bradycardia is not easy. Additional examination may be required - echocardiography (ultrasound of the heart), examination of the abdominal organs, thyroid gland, etc. A cardiologist and arrhythmologist will help the patient with this.
Our clinic “New Hospital” offers examinations necessary for a full diagnosis and selection of the correct tactics for sinus bradycardia.
Symptoms of the disease
Moderate course is rarely accompanied by obvious clinical symptoms. A severe form of pathology provokes:
- dizziness;
- weakness;
- fainting conditions;
- decreased muscle tone;
- blood pressure surges;
- profuse sweating.
Patients may experience difficulty breathing and severe chest pain. Representatives of the older age group are faced with impaired concentration, short-term memory loss, and episodic visual impairment.
Violation of myocardial contractile function leads to cerebral hypoxia. In the background, attacks of convulsions lasting up to 60 seconds may develop. This condition is considered by cardiologists as the most dangerous with confirmed bradycardia. The patient needs urgent help, since prolonged attacks of convulsions provoke cessation of respiratory activity.
Are you experiencing symptoms of bradycardia?
Only a doctor can accurately diagnose the disease. Don't delay your consultation - call
Procedures and operations
In some cases, to treat bradycardia it is necessary to resort to surgical treatment:
- removal of tumors and neoplasms of the mediastinum;
- implantation of a pacemaker .
Main indications for pacemaker implantation:
- atrial fibrillation and atrial flutter with a pulse less than 50 beats per minute;
- sick sinus syndrome with circulatory failure of III-IV degree or episodes of Morgagni-Adams-Stokes attacks;
- AV blockade IIb-III degree , which cannot be corrected and occurs 3-4 weeks after myocardial infarction;
- acquired AV block of IIB-III degree with episodes of Morgagni-Adams-Stokes attacks or circulatory failure of III-IV degree.
Relative indications for pacemaker implantation:
- chronic bi- and trifascicular blockade;
- congenital complete AV block in adults with 3rd degree circulatory failure;
- congenital AV block with circulatory failure of 3-4 degrees or SSU with episodes of Morgagni-Adams-Stokes attacks;
- an increase in the width of the QRS complex on the ECG by more than 0.8 s and a prolongation of the HR interval by more than 100 ms.
The pacemaker is selected individually depending on the degree of hemodynamic disturbances and the causes that caused them.
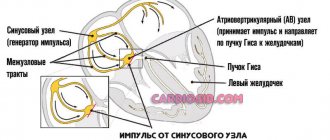
Disturbances of atrioventricular and intraventricular conduction
Heart block
- slowing down or interrupting the conduction of an impulse through a certain area of the conduction system of the heart. In some cases, the disorder leads to a lack of bioelectrical activity and cessation of heart function.
Atrioventricular block (AV block)
- disruption of the conduction of impulses from the atria to the ventricles. AV blockades can be congenital or acquired, transient or permanent. The causes of acquired AV blocks and symptoms are in many ways similar to SSSS.
There are three degrees of AV block:
- 1st degree - each impulse is carried out from the atria to the ventricles, but more slowly. As a rule, it is asymptomatic and is detected during electrocardiography or 24-hour ECG monitoring. A diagnostic sign is a prolongation of the PQ interval of more than 200 ms on the ECG;
- 2nd degree - the conduction of impulses from the atria to the ventricles is periodically interrupted. Divided into types 1 and 2. Symptoms may occur: episodes of weakness, darkening of the eyes, dizziness. In cases of advanced AV block of the 2nd stage, when several impulses in a row do not reach the ventricles, fainting may occur. ECG sign - periodic loss of the ventricular QRS complex;
- 3rd degree - complete absence of conduction of impulses from the atria to the ventricles. In this situation, the atria and ventricles contract each in its own rhythm. On the ECG, P waves and ventricular QRS complexes are not related to each other; the frequency of the atrial rhythm is more frequent than the ventricular one. Depending on the level of blockade, proximal and distal types can be distinguished. Proximal type AV block at the level of the AV node and His bundle is characterized by a high frequency of escape rhythm (usually up to 40 per minute) with narrow or slightly widened QRS. Distal AV block at the level of the His bundle branches is always characterized by widened QRS complexes with a frequency of less than 40-35 per minute. Complete AV block leads to disruption of the blood supply to vital organs, the development of heart failure, and an increased risk of sudden cardiac arrest.
In case of first degree AV block, asymptomatic 2nd degree AV block of type 1, a wait-and-see approach is used with regular diagnostics and treatment of the underlying disease. For AV block of the 3rd degree, 2nd degree of the 2nd type, symptomatic AV block, the main method of treatment is the installation of a pacemaker.
Prevention
First of all, you need to be regularly monitored by a cardiologist in order to recognize the pathology in time. In addition, preventive measures include:
- control blood pressure and bring it to normal;
- maintaining adequate weight;
- regular physical activity appropriate for age;
- diet;
- choosing foods high in vitamins and minerals that are good for the heart;
- limiting smoking and alcohol;
- if possible, minimizing stressful situations;
- good sleep, rest and relaxation.
Bradycardia is a symptom that may indicate the presence of serious diseases. Under no circumstances should it be ignored. A timely visit to the doctor will help to avoid complications and begin appropriate treatment in time if necessary.
FIND OUT PRICES
Questions and answers
What preventive measures can prevent the development of bradycardia?
Sustained heart rhythm disturbances can be avoided by promptly seeking medical help due to intoxication or deterioration in health while taking medications. Patients with a family history are recommended to undergo annual examinations with a cardiologist.
At what age can a person experience symptoms of bradycardia?
Disturbances in the functioning of the heart rhythm driver are possible at any age. The likelihood of developing a stable form increases significantly when a person reaches 65 years of age.
Treatment of bradycardia with folk remedies
How to treat bradycardia at home? The basic treatment regimen prescribed by the doctor can be supplemented with traditional medicine methods:
- decoction of rose hips;
- tincture of pine shoots;
- garlic with lemon juice;
- radish with honey;
- yarrow decoction;
- walnuts with sesame oil;
- Tatar decoction;
- tincture of Chinese lemongrass;
- yarrow decoction;
- infusion of immortelle flowers.
Treatment with folk remedies must be agreed with your doctor in order to take into account possible contraindications and exclude individual intolerance to the components of the prescription.