General information
In cardiology, the term myocardial dystrophy (myocardial dystrophy) combines a group of non-degenerative and non-inflammatory lesions of the myocardial cardiac muscle.
The code for myocardial dystrophy according to ICD-10 is I42.8 Other cardiomyopathies (dishormonal refers to I42.9 Cardiomyopathy, unspecified). The pathology is characterized by significant changes in metabolic processes and a pronounced decrease in the contractile function of the myocardium. Cardiac dystrophy is always a secondary process that combines electrolyte, dysmetabolic, neurohumoral, enzymatic and autonomic disorders. Dystrophy of the left ventricle of the heart is characterized by changes both in the myocytes themselves and in the structures of the conduction system of the heart, which leads to disturbances in the basic functions of the myocardium:
- excitability;
- conductivity;
- automatism;
- contractility.
Dystrophic degeneration of the myocardium, especially at the initial stage, is usually reversible, which greatly distinguishes it from the degeneration that occurs with cardiac amyloidosis and hemochromatosis .
Pathogenesis
metabolites accumulate . As a result of changes in biochemical processes in the myocardium, the contractility of muscle fibers is disrupted, heart failure arrhythmias develop .
Myocytes are able to fully recover after eliminating the influence of negative factors. However, too long an exposure can lead to partial death of cardiomyocytes, which are subsequently replaced by connective tissue. cardiosclerosis is formed .
Treatment of myocardial dystrophy
Treatment of myocardial dystrophy is aimed at normalizing metabolic processes in the myocardium, improving heart nutrition and eliminating the underlying disease that caused dystrophy.
In our Medical City Alexandrov, the appointment is conducted by an experienced cardiologist, a high-class specialist who will conduct a comprehensive diagnosis of the disease and prescribe the necessary treatment.
By contacting us, you can be sure of a quality result!
To make an appointment with a specialist and find out all the details, please call: 8 (49244) 9-32-49
Classification
Pathological changes in the heart are classified according to the causes of their occurrence, which will be listed below in the appropriate section, by stages and by the speed of development.
By stages
- Compensation stage . At this stage, all changes are reversible. Gradually, foci of dystrophy form in the heart muscle, which are noticeable at the microscopic level. Symptoms are minimal or completely absent.
- Subcompensation stage . All changes in cardiomyocytes are still reversible. Confluent foci of dystrophy are formed. All changes are visible at the macroscopic level, the chambers of the heart begin to enlarge. Symptoms are increasing.
- Stage of decompensation . The changes become irreversible. necrosis occurs with their gradual replacement by connective tissue, which is unable to perform the normal functions of cardiomyocytes. The structure of the heart changes, symptoms increase sharply, and the patient’s condition worsens significantly.
Classification by speed of development
- Acute form . It occurs abruptly against the background of intense exposure to negative factors ( pulmonary embolism , severe physical overexertion, complicated hypertensive crisis ).
- Chronic form . It is formed under prolonged exposure to internal and external factors of moderate strength (frequent acute infections, chronic intoxication).
Causes
Myocardial dystrophy can develop under the influence of a variety of internal and external factors that disrupt the flow of metabolic and energy processes in the heart muscle.
Degenerative changes can form under the influence of acute and chronic exogenous intoxications (drug, industrial, alcohol), various physical agents (overheating, vibration, radiation).
The structure of the myocardium
Quite often, changes in the heart muscle are formed as a result of:
- metabolic and endocrine disorders (pathological menopause, Itsenko-Cushing syndrome , vitamin deficiency , obesity , diabetes mellitus , hyperparathyroidism , hypothyroidism , thyrotoxicosis );
- infections (chronic tonsillitis );
- systemic diseases (neuromuscular dystrophy, collagenosis);
- diseases of the digestive tract ( pancreatitis , cirrhotic liver disease , malabsorption syndrome ).
In newborns and young children, myocardial dystrophy can develop as a result of intrauterine infection , perinatal encephalopathy , and cardiovascular maladaptation syndrome due to hypoxia .
Pathological changes in the heart can also be observed in athletes, which is associated with excessive physical overload ( pathological athletic heart ).
Dishormonal myocardial dystrophy
It is diagnosed mainly in women aged 45-50 years. Occurs as a result of disturbances in the estrogenic functions of the ovaries. Dyshormonal cardiodystrophy occurs extremely rarely in men aged 50-55 years as a result of disturbances in the production of the hormone testosterone .
Main complaints:
- pain in the heart area during hot flashes;
- sensations of heat in the chest;
- increased sweating;
- feeling of rapid heartbeat.
If the patient has concomitant hypertension , heart failure may develop as a complication.
The dyshormonal form of myocardial dystrophy also includes changes in the heart muscle caused by disturbances in the functioning of the thyroid gland.
Cross-section of the heart with myocardial dystrophy
With thyrotoxicosis (hyperfunction of the thyroid gland), metabolism accelerates, which leads to weight loss, rhythm disturbances, insomnia , thirst, increased excitability of the nervous system and excessive nervousness.
With hypothyroidism, metabolism slows down. Patients complain of low blood pressure , swelling, a feeling of chilliness, and aching chest pain.
Fatty degeneration of the myocardium
With severe metabolic disorders, fats begin to be deposited in the heart muscle, completely replacing the cytoplasm of cardiomyocytes over time. Fatty degeneration of the myocardium leads to a significant decrease in the contractility of the heart.
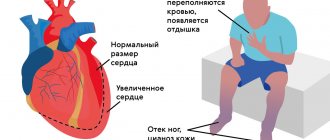
Patients complain of severe shortness of breath and aching pain in the area where the heart is located. In more advanced cases, swelling of the lower extremities occurs. Such patients are primarily indicated for lifestyle correction in parallel with drug therapy.
Dysmetabolic myocardial dystrophy
What is dysmetabolic myocardial dystrophy and when does it develop?
This pathology is observed in patients suffering from diabetes. It occurs as a result of metabolic disorders, which leads to damage to the coronary arteries . Patients complain of chest pain, simulating angina . The pain is not relieved by Nitroglycerin and is less intense.
Myocardial dystrophy of mixed origin
Several factors contribute to the development of this pathology.
What is it and how does it manifest itself? Most often, mixed myocardial dystrophy is observed in children suffering from chronic anemia . In young patients, neuroendocrine myocardial dystrophy develops, and electrolyte metabolism changes. A similar disease can also occur in adults. The very first diagnostic signs on the ECG are dysfunction of contraction (especially in the left ventricle). In the absence of adequate timely therapy, the negative effect on the heart is aggravated, disturbances begin to be registered in relation to automaticity, excitability and conductivity of the heart. And as a complication, the patient develops an acute hemodynamically significant pathological disease.
Myocardial dystrophy of complex origin
This variant is characterized by a more severe course. The disease is provoked by a systematic disturbance in the metabolism of organs and tissues, which leads to systemic changes. The first symptoms of the disease are nonspecific, which makes early diagnosis difficult. In more advanced cases, patients complain of respiratory disorders, arrhythmias, and increases in blood pressure.
Alcoholic cardiac dystrophy
It is generally accepted that this form develops with systematic, daily consumption of alcohol for 10 years. However, with a hereditary deficiency of specific enzymes that are responsible for processing ethanol, the disease can develop within 3 years. Most often, males aged 25-55 years are affected.
Myocardial dystrophy with anemia
When hemoglobin decreases below the level of 90-80 g/l, hemic hypoxia , which is accompanied by an energy deficiency in the heart muscle. The disease develops against the background of chronic blood loss, hemolytic and iron deficiency anemia, and DIC syndrome .
Causes of myocardial dystrophy
The etiology of myocardial dystrophy causes much debate among doctors. Experts believe that the list of causes of metabolic disorders in the heart is extremely wide.
Heart nutritional disorders, as a result of which the cells do not receive enough oxygen and nutrients.
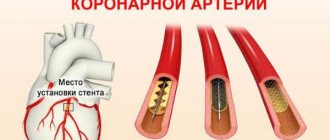
- violation of coronary circulation;
- chronic pulmonary heart disease;
- anemia, hemoglobin level in the blood less than 90-80 g/l;
- altitude sickness;
- arterial hypertension;
- heart defects;
Nervous tension , leading to a significant increase in adrenaline and excessive work of the heart;
- prolonged stress;
- depression;
- neuroses;
Excessive physical activity
- excessive loads in trained athletes;
- intense physical activity in untrained people
- intense physical activity during the period after infectious diseases (sore throat, flu);
Chronic diseases of the digestive system leading to nutritional deficiencies;
- pancreatitis;
- cirrhosis;
- malabsorption syndrome (malabsorption in the intestine);
Eating disorders accompanied by electrolyte imbalance;
- avitaminosis;
- diets with minimal protein and minerals;
Metabolic disorders. Common diseases affect the heart;
- renal and liver failure;
- gout;
- diabetes;
- obesity;
Hormonal disorders. High concentrations of hormones increase heart rate. During intense work, the energy reserves of the myocardium are depleted.
- thyrotoxicosis;
- Cushing's disease;
- menopause;
- puberty;
Poisoning with toxins that damage myocardial cells or disrupt metabolic processes.
- alcohol;
- nicotine;
- drugs;
- taking medications (cardiac glycosides);
- industrial poisons;
The causes of myocardial dystrophy in newborns are:
- oxygen starvation of the fetus;
- intrauterine infections;
- perinatal encephalopathy;
Symptoms of myocardial dystrophy
The symptoms of myocardial dystrophy directly depend on its stage. In the early stages of development, cardiac complaints may be absent. Patients experience decreased performance, rapid fatigue, and poor tolerance to habitual physical activity.
Later, as the disease progresses, patients begin to complain of prolonged, aching pain in the heart area that is not associated with physical activity and does not stop after taking Nitroglycerin . But at the same time, emotional and physical stress can provoke chest pain in such patients, but after a certain time. Most often the pain is causeless.
Often there is a feeling of rapid heartbeat, a feeling of lack of air, and shortness of breath. At later stages, swelling appears in the lower extremities, arrhythmias , and shortness of breath appears at rest. During an objective examination, you can hear a weakening of the first sound above the apex of the heart, tachycardia and a short systolic murmur.
Clinical symptoms largely depend on the cause that led to changes in the heart. With menopausal pathology, patients complain of a feeling of heat, frequent “hot flashes”, excessive sweating, and a feeling of paresthesia in the extremities. With thyrotoxicosis , rhythm and conduction disturbances develop quite quickly, and with anemia , the symptoms of heart valve defects are simulated (a pathological systolic murmur appears, characteristic of insufficiency of one of the valves: aortic, tricuspid or mitral).
Manifestations of myocardial dystrophy.
Manifestations of myocardial dystrophies are nonspecific and include pain in the heart of various types (stabbing, aching, dull) , not similar to angina, rapid heartbeat (sometimes this is only a subjective sensation with an objectively normal frequency of 80-90 per minute), sensations of “fading” of the heart, associated with extrasystole and other rhythm disturbances, sensations of lack of air. Heart pain is not associated with physical activity and does not change when taking nitroglycerin. An ECG interpretation will not show changes that are nonspecific, are not associated with physical activity and nitrate intake, and may disappear after intravenous administration of potassium chloride.
Causes of myocardial dystrophy.
The most common types of myocardial dystrophies encountered in everyday life are dishormonal (with endocrine diseases ), dysmetabolic (with diabetes, chronic renal, liver failure, other types of metabolic disorders), toxic (including alcohol), anemic (with a decrease in hemoglobin ).
Dishormonal myocardial dystrophies.
Of the hormonal disorders leading to the development of myocardial dystrophy, the most common cause is menopausal syndrome . In most women, manifestations of this syndrome appear 3-4 years before the final cessation of menstruation, and all problems that appear during this period are associated with the gradual decline of ovarian function and a decrease in the content of female sex hormones - estrogens - in the blood. Research in recent decades has shown that not only the uterus and mammary glands are sensitive to sex hormones, but also many other organs and tissues, including the heart and blood vessels. Moreover, estrogens have a protective effect on the vascular wall and myocardium, due to which women of reproductive age are significantly less at risk of cardiovascular diseases than their male peers. With a decrease in estrogen levels, these protective effects weaken, the heart becomes more vulnerable to influence from various factors of the autonomic nervous system, which intensify during menopause, resulting in various chest pains, episodes of rapid heartbeat, interruptions, and a feeling of lack of air. Hormonal changes during menopause can lead to increased blood pressure and fluid retention, which also increases the load on the heart muscle. Nervous and endocrine influences and the metabolic and dystrophic changes in the myocardium caused by them lead to the appearance of certain changes on the ECG. All this in combination - the patient’s complaints, objectively identified signs of increased heart rate and rhythm disturbances, electrocardiographic changes - requires a thorough examination, since the diagnosis of dyshormonal myocardial dystrophy associated with menopause can be made only after excluding coronary heart disease, hypertension and other serious diseases , which may also appear during this period. Signs similar to menopausal myocardial dystrophy may appear in other diseases accompanied by suppression of ovarian function, as well as after surgical removal of the ovaries.
Another common cause of dishormonal myocardial dystrophy is dysfunction of the thyroid gland, its hypo- and hyperfunction . Thyroid hormones are a necessary factor for the implementation of normal metabolic processes in all tissues of the body, including the myocardium; their deficiency leads to dystrophic processes, and their excess has a toxic effect, increases the load on the myocardium and its need for oxygen. Both hypothyroidism and thyrotoxicosis can lead to increased blood pressure. Hypothyroidism also causes weight gain and significant fluid retention. Both hyper- and hypothyroidism are fraught with the development of various types of extrasystole and atrial fibrillation. Thyrotoxicosis is also characterized by severe tachycardia - a constant, even at rest, increase in heart rate to 120 or more per minute. Actually, damage to the heart muscle due to hyperfunction of the thyroid gland, thyrotoxicosis, largely belongs to the next group of myocardial dystrophies - toxic myocardial dystrophies.
Toxic myocardial dystrophy.
In addition to thyrotoxicosis, toxic myocardial dystrophies include myocardial damage due to various intoxications, for example, when exposed to occupational factors, taking certain medications, drug use and, of course, alcohol abuse. The last group is one of the most common causes of heart damage, not related to coronary disease, but having serious, sometimes fatal, consequences.
Alcohol has a pronounced toxic effect on the heart muscle, especially when consumed systematically . The action of ethanol leads to the development of a deficiency of potassium, magnesium, calcium, vitamins, especially group B, and glucose necessary for normal cell functioning. The level of adrenaline and other catecholamines circulating in the blood increases, negatively affecting the myocardium, increasing its need for oxygen and accelerating the heart rate. Arterial hypertension develops. Over time, all this leads to the development of severe myocardial dystrophy, which is manifested by tachycardia, extrasystole, atrial fibrillation and, ultimately, heart failure.
Treatment of myocardial dystrophies.
Treatment is primarily associated with the elimination or correction of the underlying disease - hormone replacement therapy for menopause, the administration of thyroxine for hypothyroidism, surgical treatment or the prescription of special drugs for thyrotoxicosis. If it is impossible to completely eliminate the cause, then therapy is carried out depending on the existing symptoms, their severity and significance. If necessary, antiarrhythmic drugs, potassium, magnesium and others are prescribed. In all cases of cardiac complaints, especially in combination with any changes on the ECG, a comprehensive examination of the patient is necessary, taking into account his age, gender, professional factors, his life history, diseases and bad habits, to establish the cause and exclude possible emergencies states.
To avoid serious consequences, you should, at the first signs of myocardial dystrophy, consult a doctor who will conduct hardware diagnostics and prescribe a course of treatment. Call our medical center, which is open 7 days a week and make an appointment with a doctor. This will help you avoid serious consequences. It's better to be safe than to end up in a hospital bed .
What happens to the body during prolonged drinking.
Tests and diagnostics
In the anamnesis, patients with myocardial dystrophy reveal various pathological conditions and diseases, which are manifested by disturbances in metabolic processes and tissue hypoxic syndrome. Objectively, when examining the heart, you can hear a weak systolic murmur, a weakening of the first sound at the apex of the heart, muffled heart sounds and irregular rhythm.
The electrocardiogram records nonspecific changes in the myocardium, disturbances in repolarization processes, arrhythmias, and signs of decreased myocardial contractile function.
Drug and stress tests give a negative result (coronary artery disease is excluded).
When performing phonocardiography , the ratio of the duration of electrical and mechanical systole changes.
Echocardiography confirms the expansion of the cavities of the heart, changes in the structures of the heart muscle are recorded. In this case, no organic pathology is observed.
If chest x-ray a myopathic configuration of the heart , then this indicates deep damage to the myocardium.
Using scintigraphy, you can assess the perfusion and metabolism of the heart muscle, detect diffuse/focal changes, which will indicate a decrease in the number of normally functioning cardiomyocytes.
In extremely doubtful cases, they resort to myocardial biopsy , when all non-invasive studies performed have not yielded any result. Differential diagnosis is carried out with such diseases as:
- myocarditis;
- IHD;
- cor pulmonale;
- cardiosclerosis;
- heart defects.
UAC indicators are usually normal.
Ischemic myocardial dystrophy
Ischemic myocardial dystrophy , or acute focal myocardial dystrophy, develops during relatively short-term episodes of coronary crisis, when characteristic changes in the electrocardiogram occur, but fermentemia (increased activity of transaminases, lactate dehydrogenase, etc.) is absent, which is one of the proofs of the absence of myocardial necrosis.
The myocardium is flabby and pale, in areas of ischemia it is sometimes mottled and edematous. A fresh thrombus is often found in the coronary artery.
Macroscopic diagnosis of foci of ischemic dystrophy is possible using tetrazolium salts and potassium tellurite. In areas of ischemia, where the activity of redox enzymes is sharply weakened, formazan grains and reduced tellurium do not fall out, so the areas of ischemia appear light against the dark background of the unchanged myocardium.
Microscopically, paretic expansion of capillaries, stasis of erythrocytes, and edema of interstitial tissue are found. These changes may be associated with hemorrhages and leukodiapedesis, accumulations of leukocytes along the periphery of the ischemic zone. Muscle fibers lose their striations, are deprived of glycogen, they are intensely stained with eosin, fuchsin, pyronin and Schiff's reagent, which indicates necrobiotic changes. Stained with acridine orange, they give a green, rather than orange, glow in a fluorescent microscope, which makes it possible to distinguish the ischemic zone from the intact myocardium.
Early electron microscopic and histochemical changes are reduced to a decrease in the number of glycogen granules, a decrease in the activity of redox enzymes (especially dehydrogenases and diaphorases), swelling and destruction of mitochondria and the sarcoplasmic reticulum. These changes, associated with impaired tissue respiration, increased anaerobic glycolysis and uncoupling of respiration and oxidative phosphorylation, appear within a few minutes from the onset of ischemia. An important role in primary ischemic changes in myocardial ultrastructures belongs to the release of catecholamines and ionic shifts (loss of magnesium, potassium and phosphorus, accumulation of sodium, calcium and water), which determine hydropic-destructive changes in ultrastructures in the late stages of myocardial ischemia.
A complication of ischemic myocardial dystrophy is most often acute heart failure, which also becomes the direct cause of death. Apparently, this is why clinicians usually refer to this form of coronary heart disease as “acute heart failure.”
Treatment of myocardial dystrophy with folk remedies
Traditional methods of treatment can only be an addition to the main therapy, but not replace it.
Rosehip flower tincture
The prepared solution helps to normalize cardiac activity, even out heart rhythm during arrhythmia, and replenish the lack of vitamin C.
Pour two cups of boiling water over 2 tablespoons of rosehip flowers and let it brew for an hour. The prepared infusion should be taken before meals, 1 tablespoon.
Lemon harvest
Citrus collection will help normalize heart function and strengthen the heart muscle. To prepare a thick paste, you need to grind 150 grams of fresh figs and 250 grams of lemon in a meat grinder. Then add 50 grams of vodka and 100 grams of liquid bee honey to the resulting consistency. Lemon infusion should be taken three times a day, 1 teaspoon.
Honey-beet tincture
To improve blood circulation in the heart muscle and get rid of tachycardia, honey-beetroot tincture is recommended. Additionally, the solution has a sedative effect.
To prepare, stir 1 teaspoon of bee bread in 100 ml of a mixture of beetroot juice and honey (50/50). Let sit in the refrigerator for 3 hours. The resulting infusion should be taken three times a day, 3 tablespoons.
Folk remedy for shortness of breath
A frequent companion to myocardial dystrophy is shortness of breath . Breathing practices help combat it. Additionally, you can use proven traditional methods.
Squeeze the juice out of 10 whole heads of garlic and 10 lemons, and mix the resulting solution with 1 liter of bee honey. Place the finished mixture in a container, seal it tightly, and place it in a cool, dark place for 7 days. You need to take 4 teaspoons of the mixture daily for two months. The mixture should not be swallowed immediately; try to dissolve it slowly.
Vitamin cocktail
One of the primary tasks in the treatment of heart pathology is the general strengthening of the body and acceleration of metabolism. A healthy vitamin cocktail will solve these two problems at once.
Mix the juice of 1 grapefruit, 2 kiwis and 4 oranges. Pour a glass of rose hips into a liter of water and cook for 20 minutes. Let cool, then strain with cheesecloth and add to the berry mix. Additionally, grate the ginger root and add 1 teaspoon of honey to the resulting mixture.
Healing herbal tea
The presented recipe will allow you to prepare a collection that has a positive effect on the functioning of the cardiovascular and endocrine systems.
You'll need:
- 2 tbsp. spoons of oregano and valerian;
- 1.5 tbsp. spoons of adonis flowers and mint leaves;
- 1 tbsp. a spoonful of motherwort herb, juniper and dill fruits.
Pour boiling water over everything at the rate of 1 tbsp. spoon of herbal mixture per 1 liter of water. Bring the infusion to a boil and let it sit for 24 hours. You need to take the resulting solution before meals, 100 g.
Prevention
Lifestyle is of great importance in the prevention of myocardial dystrophy. Almost all preventive measures are aimed at correcting an existing lifestyle.
It is recommended to stop drinking alcoholic beverages and smoking. It is necessary to promptly treat all identified pathological changes in the heart muscle and various infectious diseases.
It is important to monitor the correct functioning of the endocrine system. obese people - dietary. Weight correction is important.
It is better to avoid excessive physical activity so as not to force the heart once again. When playing sports, you must take into account your physical fitness. Don't forget about warming up, which allows you to balance physical activity. Try to refuse to work in hazardous industries - health is more valuable than any money.
Main aspects of the prevention of myocardial dystrophy
- sanitation of foci of infection;
- complete, healthy, balanced diet;
- timely maintenance drug therapy (if cardiac pathology is detected, especially with dystrophic changes in the myocardium).
In children
In children, myocardial dystrophy can develop as a result of hypervitaminosis , rickets , chronic dietary disorders, bacterial and viral infections. Often this pathology is observed at an early age due to lack of physical activity, or, on the contrary, due to excessive force overload.
In pediatric practice, myocardial dystrophies that developed as a result of drug poisoning were observed.
Most often, the cause of the disease is vegetative, nervous and endocrine disorders.
The main symptoms in children consist of:
- asthenia;
- shortness of breath with minimal physical activity;
- weakening the sonority of heart sounds.
Myocardial dystrophy in children
Cardiac dystrophy in children usually occurs for the same reasons as in adults, but it also has a number of features.
Newborns often suffer from myocardial dystrophy - if the mother’s pregnancy was disturbed and the fetus did not receive enough nutrients. In preschool children, myocardial dystrophy can develop due to poor nutrition, often leading to anemia. At school age and during puberty, the cause of the disease is great emotional and physical stress, as well as hormonal changes in the body.
During pregnancy
The most common myocardial disease in pregnant women is myocardial dystrophy.
Gynecologists quite often have to deal with this diagnosis in everyday practice, although it is not always justified. If we move away from all cases where myocardial dystrophy borders on other organic heart diseases ( valvular defects , myocarditis , etc.), then only those pathological changes that occur with anemia, vitamin deficiency, intoxication, overwork can be attributed to cardiac muscle dystrophy. pregnant women.
For pregnant women who suffer from myocardial dystrophy, according to the Institute of Obstetrics and Gynecology of the Academy of Medical Sciences, the following are typical: the addition of late toxicosis (35%), premature rupture of water (28%), weakness of labor (12%), perinatal mortality (6%).
Therapy for pregnant women with myocardial dystrophy consists of eliminating the underlying disease that caused this pathology, compensating for cardiac activity and eliminating pregnancy complications. Termination of pregnancy is not necessary in most cases.
Diseases of the myocardium, endocardium and pericardium in pregnant women
Myocardial diseases during pregnancy
Myocardial diseases of inflammatory and non-inflammatory etiology are represented by myocarditis, myocardial dystrophy, cardiosclerosis and myocardiopathy.
Myocarditis is an inflammatory disease of the heart muscle of an infectious, infectious-allergic or infectious-toxic nature. Myocarditis during pregnancy can be caused by viral, bacterial, purulent-septic infection, and are also observed with parasitic and protozoal infestations. In pregnant women, rheumatic carditis, both primary and developed against the background of various defects, is more common. Pregnancy worsens the course of the disease, so myocarditis in the early stages of pregnancy is an indication for its termination. In the case of uncomplicated myocarditis and the absence of serious concomitant diseases, pregnancy continues and proceeds safely.
Myocardial dystrophies are based on biochemical or metabolic disorders in the heart muscle, caused by endocrine diseases or intoxication, as well as metabolic disorders. Myocardial dystrophy does not have a clear clinical picture; the latter usually manifests itself as symptoms of the underlying disease. In severe thyrotoxic cardiodystrophy with atrial fibrillation, pregnancy is contraindicated. Anemic myocardial dystrophy goes away as the anemia is cured, which is usually done effectively.
Cardiomyopathies during pregnancy can be primary or secondary against the background of various general diseases. The primary forms of this pathology include idiopathic myocardial hypertrophy of the non-obstructive and obstructive type. With mild obstruction, pregnancy proceeds favorably, but one should remember the genetic determination of this pathology and the risk of giving birth to a sick child.
Endocardial diseases during pregnancy
There are acute, subacute and prolonged septic endocarditis during pregnancy. The disease is caused by infection during pregnancy (usually strepto- and staphylococci). It is characterized by growths (consisting of fibrin, platelets, polymorphic leukocytes) of various sizes and shapes on the valve leaflets, chordae tendineae and parietal endocardium. The mitral, aortic, or both valves are most often affected. Pregnancy predisposes to the development of endocarditis against the background of various defects, especially in the presence of infection.
Pregnancy with bacterial endocarditis should be interrupted, although this is unsafe and may be accompanied by thrombo-embolic complications and heart failure. Subsequently, if the outcome of the disease is favorable, pregnancy is permissible after a year.
Pericardial diseases during pregnancy
The cause of illness during pregnancy is infection (viral, bacterial, fungal, parasitic). Pericarditis can develop with collagenosis, allergic conditions and metabolic disorders, as well as with radiation injury, after heart surgery. Constrictive pericarditis is a contraindication for pregnancy.
Pregnancy and systemic lupus erythematosus
Systemic lupus erythematosus is an autoimmune disease of connective tissue. It occurs more often in women of reproductive age. It is detected during pregnancy, after childbirth and abortion, sometimes after taking medications (with individual intolerance to sulfonamides, antibiotics), as well as after stressful situations (surgeries, colds, mental trauma). The diagnostic criterion is the presence of lupus cells and specific antibodies in the blood.
Systemic lupus erythematosus during pregnancy - forms and symptoms
The clinical course of the disease can be slow or rapid progression. There are the following forms of lupus erythematosus: visceral, endocardial, polyarthritic, renal, anemic and neuropsychic. It is characterized by a polymorphism of symptoms: skin manifestations, cardiac changes, damage to the lungs, spleen and lymph nodes, vasculitis and thromboembolic complications. Kidney damage with pronounced changes indicates the progression of the disease, is a difficult-to-reversible process and can quickly lead to death. Pregnancy worsens the patient's condition and is contraindicated in most cases.
Pregnancy in women with heart surgery
This contingent of pregnant women (even after successful surgical interventions) should be considered as suffering from heart disease. The decision on the admissibility of pregnancy and childbirth in women undergoing heart surgery should be made taking into account the effectiveness of the operation, the activity of the rheumatic process, possible relapse of the disease, pulmonary hypertension, arrhythmias, heart failure, etc.
Heart surgeries are also performed during pregnancy (at 16-26 weeks).
Management and treatment of pregnant women with heart disease
The question of the possibility of pregnancy in women with heart disease should be decided jointly by a cardiologist (general practitioner) and an obstetrician-gynecologist. If pregnancy occurs, then they must develop an action plan for its management in order to prevent or promptly identify possible complications. If the pregnancy needs to be terminated, this is done in the early stages (up to 12 weeks).
Pregnancy is contraindicated or termination is indicated before 12 weeks in the following conditions:
- any form of anatomical lesion with symptoms of circulatory failure or activity of the rheumatic process;
- bacterial endocarditis;
- pronounced mitral stenosis and combined mitral disease with a predominance of stenosis;
- severe aortic stenosis;
- combined aortic disease;
- coarctation of the aorta and stenosis of the pulmonary artery;
- tricuspid valve defects;
- pulmonary hypertension with any heart defect;
- heart defects in combination with arterial hypertension or chronic glomerulonephritis;
- all “blue” heart defects;
- congenital defects of the “pale” type with signs of severe pulmonary hypertension;
- defects of the interatrial and interventricular septa, as well as patent ductus arteriosus with severe symptoms of reverse blood flow, enlargement of the right heart, signs of decompensation and pulmonary hypertension;
- acute and subacute forms of myocarditis;
- myocardial dystrophy and myocardiosclerosis with dysfunction of the conduction system and arrhythmia;
- myocardial diseases with circulatory failure;
- incomplete surgical correction or recurrence of acquired or congenital heart diseases.
Clinical observation of pregnant women is carried out by an obstetrician-gynecologist together with a therapist and a cardiologist with the participation of a midwife. A thorough examination of the state of the cardiovascular system and all major organs and systems is carried out every 2 weeks, and if necessary, more often.
All pregnant women with diseases of the cardiovascular system are hospitalized at least three times during pregnancy:
within a period of up to 12 weeks for a complete examination, making a full diagnosis and deciding whether it is permissible to continue the pregnancy, developing management tactics and the necessary therapy;
in 28 - 32 weeks of pregnancy - during the period of the most unfavorable hemodynamic conditions and maximum load on the heart for appropriate therapy;
2 - 3 weeks before birth to prepare for childbirth, appropriate therapy and develop management tactics, method of delivery.
If the disease progresses, treatment is ineffective, or complications occur in the heart (arrhythmias, heart failure, thromboembolism, activity of the rheumatic process) and pregnancy (preeclampsia, fetal hypoxia, threat of miscarriage), immediate hospitalization is indicated.
It is advisable to terminate pregnancy at a later stage by cesarean section.
The issue of lactation is decided individually; it is inappropriate in all cases of decompensation, circulatory disorders, and activity of the rheumatic process. To suppress lactation, parlodel is used, 1 tablet (2.5 mg) 2 times a day for two weeks. Dispensary observation continues by an obstetrician-gynecologist and therapist in the postpartum period, then women are under the supervision of a cardiologist.
Complex therapy for pregnant women with heart disease includes
. protective regime, therapeutic nutrition, prevention and treatment of circulatory failure, increased reactivity of the mother and fetus, pathogenetic and symptomatic treatment of the main and concomitant diseases, prevention and treatment of hypoxia and acidosis of the mother and fetus.
Pregnant women with full compensation and the absence of various complications and concomitant diseases do not need special restrictions on physical activity compared to healthy pregnant women.
For all decompensated conditions, heart failure, strict bed rest is indicated, often in a hospital setting.
Drug therapy for pregnant women with heart surgery
Drug therapy is carried out according to traditional principles of cardiology, but taking into account its possible effect on the fetus. It is known that women with heart disease are more likely to give birth to children with congenital defects, including heart defects, which are mainly due to multifactorial causes. Defects are often discovered several months or years after birth. When drug therapy, it is important to take into account the timing of pregnancy: the phase of organogenesis is critical in relation to teratogenicity (8 weeks, for the heart - up to 40 days), after this period the embryotoxic effect of pharmacological agents appears. Of the antihypertensive drugs, nitroglycerin is preferred as an ambulance - 1 tablet under the tongue. Of the anticoagulant agents, heparin is prescribed in the first 10-12 weeks and the last 2-4 weeks of pregnancy, and indirect anticoagulants are prescribed in the remaining periods. Prescribe medications aimed at treating maternal and fetal hypoxia (riboxin, multivitamins, methionine, ascorbic acid, 20-40% glucose solution, unithiol, trental). Oxygen therapy is always indicated.
Careful treatment of myocardial, endocardial and pericardial diseases in pregnant women is very important.
Diet for myocardial dystrophy
Diet for heart failure
- Efficacy: therapeutic effect after 20 days
- Timing: constantly
- Cost of products: 1700-1800 rubles. in Week
Diet for vegetative-vascular dystonia (VSD)
- Efficacy: Healing effect
- Timing: constantly
- Cost of products: 1500-1600 rubles per week
Basic rules in nutrition:
- restriction in salt consumption (no more than 3 g per day);
- counting calories consumed;
- drinking enough liquid;
- weight control;
- eating foods rich in potassium, magnesium and fiber;
- consumption of multivitamins and fortified foods;
- avoidance of coffee and alcohol-containing products.
Consequences and complications
Dangerous complications and consequences of an untreated disease:
- Chronic heart failure. Manifested by swelling, severe shortness of breath and general weakness. Initially, symptoms appear only during exercise, in more advanced cases - at rest and with minimal physical activity. Without adequate therapy, CHF progresses quite quickly and leads to death.
- Rhythm and conduction disorders . Changes concern the generation and conduction of nerve impulses through the heart muscle. It all can start with rare, seemingly harmless extrasystoles . Further, the disease progresses and affects conduction, provoking sinoatrial and atrioventricular blockades. Atrial fibrillation is often recorded . Patients complain of loss of consciousness, shortness of breath, and a feeling of arrhythmia. Treatment can be medication or emergency surgery (EC implantation).
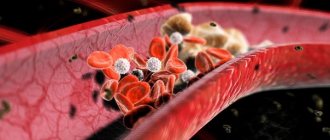
- With severe hemodynamic disturbances, blood clots , which can travel through the bloodstream to the brain, kidneys, eyes, etc.
Myocardial dystrophy
Myocardial dystrophy with anemia
Disturbances in the myocardium develop when hemoglobin decreases to 90-80 g/l.
Against this background, hemic hypoxia develops, accompanied by energy deficiency in the myocardium. Anemic myocardial dystrophy can occur with iron deficiency and hemolytic anemia, with acute and chronic blood loss, and disseminated intravascular coagulation syndrome. Clinical manifestations of myocardial dystrophy in anemia include pallor of the skin, dizziness, shortness of breath, tachycardia, and increased pulsation of the carotid arteries. Percussion examination reveals expansion of the borders of the heart, indicating myocardial hypertrophy. Auscultation reveals loud heart sounds, systolic murmurs over the heart and blood vessels, and a “spinning top noise” on the cervical vessels. Heart failure develops with prolonged anemia and inadequate treatment.
Myocardial dystrophy with thyrotoxicosis
Under the influence of an excess amount of thyroid hormones in the heart muscle, the synthesis of adenosine triphosphoric acid (ATP) and creatine phosphate (CP) is reduced, which is accompanied by energy and then protein deficiency. At the same time, thyroid hormones stimulate the activity of the sympathetic nervous system, causing an increase in heart rate, minute blood volume, blood flow velocity, and bcc. Under such conditions, changes in intracardiac hemodynamics cannot be supported energetically, which ultimately leads to the development of myocardial dystrophy.
In the clinic of myocardial dystrophy in thyrotoxicosis, arrhythmias (sinus tachycardia, extrasystole, paroxysmal tachycardia, atrial fibrillation) predominate. Long-term thyrotoxicosis causes chronic circulatory failure, mainly of the right ventricular type, which is manifested by pain in the heart, edema, and hepatomegaly. Sometimes, with thyrotoxicosis, the symptoms of myocardial dystrophy dominate, and therefore patients turn, first of all, to a cardiologist, and only then go to an endocrinologist.
Myocardial dystrophy with hypothyroidism
The pathogenetic basis of myocardial dystrophy in hypothyroidism is a deficiency of thyroid hormones, leading to a decrease in metabolic activity in the myocardium. In this case, as a result of increased vascular permeability, fluid retention occurs in myocytes, which is accompanied by the development of dysmetabolic and electrolyte disorders (increased sodium content and decreased potassium).
Myocardial dystrophy in hypothyroidism is characterized by constant aching pain in the heart, arrhythmias (sinus bradycardia), blockades (atrial, atrioventricular, ventricular).
Alcoholic and toxic myocardial dystrophy
It is believed that alcoholic myocardial dystrophy is caused by daily intake of 80-100 ml of ethyl alcohol for 10 years. However, with a hereditary deficiency of a number of enzymes that break down ethanol, stress, and frequent viral infections, myocardial dystrophy can develop in a shorter time - within 2-3 years, even when consuming smaller amounts of alcohol. Alcoholic myocardial dystrophy occurs mainly in men 20-50 years old.
Toxic myocardial dystrophy occurs in individuals receiving long-term therapy with immunosuppressants (cytostatics, glucocorticosteroids), NSAIDs, some antibiotics, tranquilizers, as well as in cases of poisoning with chloroform, phosphorus, arsenic, carbon monoxide, etc. Such variants of myocardial dystrophy can occur in cardialgic (painful) conditions. , acute arrhythmic, combined and congestive forms.
The cardialgic form of myocardial dystrophy is characterized by pinching or aching pain in the chest, a transient sensation of heat or chilliness in the extremities, and sweating. Patients are concerned about general weakness, fatigue, decreased physical endurance, and headaches.
The arrhythmic form of myocardial dystrophy is accompanied by tachycardia, disturbances of rhythm and conduction of the heart (sinus tachy- or bradycardia, extrasystole, bundle branch blocks), sometimes - attacks of fibrillation and atrial flutter. In the combined form of myocardial dystrophy, arrhythmias and cardialgia are observed. Manifestations of congestive myocardial dystrophy are caused by heart failure and include shortness of breath on exertion, cough, attacks of cardiac asthma, swelling in the legs, hydropericardium, hydrothorax, hepatomegaly, ascites.
Tonsillogenic myocardial dystrophy
Myocardial lesions during tonsillitis occur in 30-60% of patients. Tonsillogenic myocardial dystrophy usually develops after a series of tonsillitis, occurring with high fever and intoxication. In the clinic of tonsillogenic myocardial dystrophy, complaints of intense pain in the heart area, severe weakness, irregular pulse, shortness of breath, focal or diffuse sweating, low-grade fever, and arthralgia prevail.
Myocardial dystrophy of physical overexertion
Develops in athletes who perform physical activity that exceeds their individual capabilities. In this case, myocardial damage can be caused by hidden chronic foci of infection in the body - sinusitis, tonsillitis, adnexitis, etc.; lack of proper rest between workouts, etc. Regarding the pathogenesis of myocardial dystrophy of physical exertion, a number of theories have been put forward: hypoxic, neurodystrophic, steroid-electrolyte.
This variant of myocardial dystrophy is mainly manifested by general symptoms: weakness, lethargy, fatigue, depressed mood, decreased interest in sports. Palpitations, tingling in the heart area, and interruptions may occur.
Menopausal myocardial dystrophy
Develops as a result of dishormonal processes in women aged 45–50 years. Menopausal myocardial dystrophy is manifested by pain in the heart area of a pressing, stabbing or aching nature, radiating to the left arm. Cardialgia intensifies due to “hot flashes” and is accompanied by a feeling of heat, rapid heartbeat, and increased sweating. Heart failure in menopausal myocardial dystrophy can develop with existing concomitant arterial hypertension.
Forecast
The prognosis is considered favorable for stages I and II. Heart functions can be fully restored after the cause-and-effect factor is eliminated. The duration of the recovery period is largely influenced by the general condition of the body (the fastest recovery is observed at a young age and in the absence of concomitant pathology), the time of initiation of therapy (the earlier competent treatment is prescribed, the faster the disease regresses). The duration can range from 1 year to several years.
At stage III, the prognosis directly depends on the presence of complications and the severity of already formed changes. When changes in the heart muscle are diagnosed, the emphasis is not on the patient’s well-being and restoration of normal heart parameters, but on reducing the rate of progression of chronic heart failure and restoring the rhythm. In the third stage, lifelong therapy is required. In the absence of adequate treatment, the life prognosis is extremely unfavorable.