Ventricular extrasystole, what is it? Treatment and consequences
Ventricular extrasystoles (VES) are extraordinary contractions of the heart that occur under the influence of premature impulses that originate from the intraventricular conduction system.
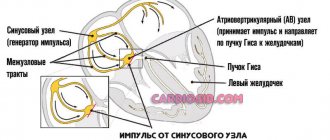
Under the influence of an impulse generated in the trunk of the His bundle, its branches, branching branches or Purkinje fibers, the myocardium of one of the ventricles contracts, and then the second ventricle without previous contraction of the atria. This explains the main electrocardiographic signs of PVCs: premature dilated and deformed ventricular complex and the absence of a normal P wave preceding it, indicating atrial contraction.
What it is?
Ventricular extrasystole is one of the types of arrhythmias, which are premature, out-of-order contractions of the ventricles. Ventricular extrasystole is characterized by a feeling of disturbances in the functioning of the heart in the form of failures, weakness, dizziness, anginal pain and lack of air.
This type of arrhythmia is established after listening to the heart, electrocardiogram and Holter monitoring. And to treat extraordinary contraction of the ventricles, sedatives, beta-blockers and antiarrhythmic drugs are used.
Causes
The reasons for ventricular extrasystole appear in heart disease:
- inflammatory nature (myocarditis, endocarditis, intoxication);
- myocardial ischemia (foci of cardiosclerosis, acute infarction);
- metabolic-dystrophic changes in the muscle and conduction system (impaired potassium-sodium electrolyte ratio in myocytes and intercellular space);
- a sharp depletion of the energy supply of cells caused by malnutrition, lack of oxygen in acute and chronic heart failure, and decompensated defects.
Ventricular extrasystoles may appear in people with a healthy cardiovascular system due to:
- irritation of the vagus nerve (due to overeating, insomnia, mental work);
- increased tone of the sympathetic nerve (smoking, physical work, stress, hard work).
If there are two sources of impulse formation in the heart, then the main one is the one that is capable of a higher frequency. Therefore, normal sinus rhythm is most often maintained. But extrasystoles can also occur against the background of atrial fibrillation.
Clinical manifestations
In most patients, in the absence of damage to the cardiovascular and nervous systems, extrasystole occurs hidden. There are no specific complaints inherent to the disease. Its pronounced clinical picture is usually represented by the following symptoms:
- weakness;
- irritability
- dizziness/headaches;
- feeling of discomfort in the chest (pain, tingling, heaviness);
- heart sinking feeling
- a push in the chest with frequent extrasystoles;
- arrhythmic pulse;
- feeling of pulsation in the veins of the neck;
- dyspnea.
The presence of concomitant cardiac pathology aggravates the course of the disease.
Classification
Not all specialists use the existing classification of ventricular extrasystole according to Laun and Wolf. She offers five degrees of extrasystole during myocardial infarction according to the risk of developing fibrillation:
- degree 1 - monomorphic extraordinary contractions are recorded (no more than 30 per hour of observation);
- grade 2 - more frequent, from one focus (over 30 per hour);
- degree 3 - polytopic extrasystole;
- degree 4 - subdivided depending on the ECG pattern ri - paired and "b" - salvo);
- degree 5 - the most dangerous type “R on T” in a prognostic sense is registered, which means that the extrasystole “climbed” onto the previous normal contraction and is capable of disrupting the rhythm.
In addition, a “zero” degree was allocated for patients without extrasystole.
M. Ryan's proposals for gradation (classes) supplemented the B. Lown - M. Wolf classification for patients without myocardial infarction. In them, “gradation 1”, “gradation 2” and “gradation 3” completely coincide with Launov’s interpretation.
The rest have been changed:
- “gradation 4” - considered in the form of paired extrasystoles in monomorphic and polymorphic versions;
- “gradation 5” includes ventricular tachycardia.
Examples of diagnosis formulation:
WPW syndrome, frequent paroxysms of supraventricular tachycardia (up to 2-3 times a month).
DCM, complete block of the left bundle branch, frequent polytopic ventricular extrasystoles, CHF II B, FC III. Cardiac asthma.
- Single polymorphic ventricular extrasystole
3. IHD: exertional angina, FC III. Post-infarction cardiosclerosis (with Q wave, infarction, date, localization). SSSU corrected with a pacemaker (date). CHF II A, cardiac asthma.
Background: Stage III hypertension, stage 2 hypertension, risk 4.
4. IHD: progressive angina. PIX (date, location), aneurysm of the anterior wall of the left ventricle. Incomplete AV block II degree (Mobitz II), CHF III, FC IV.
Symptoms
Single ventricular premature contractions are recorded in half of healthy young people during monitoring for 24 hours (Holter ECG monitoring). They do not affect your well-being. Symptoms of ventricular extrasystole appear when premature contractions begin to have a noticeable effect on the normal rhythm of the heart.
Ventricular extrasystole without concomitant heart diseases is very poorly tolerated by the patient. This condition usually develops against the background of bradycardia (slow pulse) and is characterized by the following clinical symptoms:
- a feeling of cardiac arrest, followed by a whole series of beats;
- from time to time, separate strong blows are felt in the chest;
- extrasystole may also occur after eating;
- a feeling of arrhythmia occurs in a calm position (during rest, sleep or after an emotional outburst);
- During physical activity, the disturbance practically does not appear.
Ventricular extrasystoles against the background of organic heart diseases, as a rule, are multiple in nature, but for the patient they are asymptomatic. They develop with physical activity and go away while lying down. Typically, this type of arrhythmia develops against the background of tachycardia.
Many women during pregnancy experience tachycardia and pain in the left side of the chest. The development of PVCs in an expectant mother is not uncommon. This is explained by the fact that the circulatory system and the heart have a double burden. In addition, one should take into account the physiological changes in hormonal levels, which affect the rhythm of impulses. Such extrasystole is not malignant and can be easily treated after childbirth.
Diagnostic methods
Diagnosis of the disease is carried out by two main methods, which include 24-hour ECG and Holter ECG monitoring.
- An electrocardiogram records all unscheduled contractions of the ventricle, allowing the frequency and sequence of the heart rhythm to be determined.
- The bicycle ergometry method makes it possible to identify the dependence of the manifestations of gallbladder extrasystoles on the load received, as well as to classify the disease, which greatly facilitates the development of a treatment program.
- Polycardography, TEE, sphygmography and other methods can also be used as diagnostic methods.
Extrasystole cannot always be detected on an ECG. This is due to the fact that this study is carried out quite quickly (about 5 minutes), and single extrasystoles may simply not be captured on film. In this case, other types of diagnostics are used. One of the techniques is Holter monitoring. It is carried out during the day, in the patient’s usual physical activity, after which the doctor determines whether any heart rhythm disturbances have occurred during this time and how dangerous they are to the patient’s life.
general information
Extrasystole means a disturbance in the rhythm of the heart muscle. For various reasons, it may contract prematurely. To determine pathological processes, an electrocardiogram is required. The graph will display an accelerated or premature extrasystolic complex.
It can be parasystolic and extrasystolic
It is important to promptly track these changes to prevent negative consequences and complications. Extrasystole and parasystole are responsible for the work of the main muscle in the body
When their functioning is disrupted, the treatment in both cases is the same.
Extrasystole often occurs in the ventricles of the heart. Pathological processes can occur in the supraventricular region, in the atrium, and atrioventricular muscle.
Treatment of ventricular extrasystole
For benign ventricular extrasystole, which is well tolerated by the patient, drug treatment is not carried out. It is recommended to give up bad habits, modify risk factors, and possibly take Corvalol.
In case of frequent PVCs, pronounced clinical manifestations, or malignant course, antiarrhythmic drugs are prescribed:
- Propafenone is a class I antiarrhythmic, used when the course is benign. Contraindicated in cases of LV aneurysm and severe heart failure.
- Bisoprolol is an adrenergic blocker that prevents ventricular fibrillation and regulates heart rate. Contraindicated in patients with bronchial asthma.
- Cordarone is the drug of choice for malignant and prognostically unfavorable PVCs. Reduces cardiac mortality rates.
Surgical treatment is carried out for frequent ventricular extrasystoles, which are difficult to treat with drugs. An electrophysiological study is performed to determine the exact location of the lesion and its radiofrequency ablation.
How to treat ventricular asystole
Treatment of asystole or cardiac arrest occurs in three stages:
- emergency help;
- emergency assistance with medications;
- surgical treatment.
First emergency aid in case of cardiac arrest must be provided immediately, since it determines whether the person will survive. First you need to perform an indirect cardiac massage, which is performed by punching the chest area. If special equipment is available, it is necessary to perform defibrillation, connect the victim to a ventilator and provide him with pure 100% oxygen using a mask or endotracheal tube.
If the first emergency aid does not bring the person back to his senses, special medications must be used. These drugs include adrenergic agonists, antiarrhythmic drugs, and M-blockers. Such drugs will help improve the conduction of impulses throughout the organ, thereby increasing the number of heart contractions and restoring normal heart rhythm.
As for surgical treatment, it consists of pericardiocentesis and puncture of the pleural cavity.
Lifestyle with ventricular extrasystole
With ventricular extrasystole, especially caused by other heart diseases, you need to rest more, spend more time in the fresh air, observe a work-rest schedule, eat right, avoid drinking coffee, alcohol, and reduce or eliminate smoking.
Patients with a benign type of ventricular extrasystole do not need to limit physical activity. With the malignant type, significant stress and psycho-emotional situations that can lead to the development of an attack should be limited.
Traditional methods
If the extrasystole is not life-threatening and is not accompanied by hemodynamic disturbances, you can try to defeat the disease on your own. For example, when taking diuretics, potassium and magnesium are removed from the patient’s body. In this case, it is recommended to eat foods containing these minerals (but only in the absence of kidney disease) - dried apricots, raisins, potatoes, bananas, pumpkin, chocolate.
Also, to treat extrasystole, you can use an infusion of medicinal herbs. It has cardiotonic, antiarrhythmic, sedative and mild sedative effects. It should be taken one tablespoon 3-4 times a day. For this you will need hawthorn flowers, lemon balm, motherwort, heather and hop cones. They need to be mixed in the following proportions:
- 5 parts each of lemon balm and motherwort;
- 4 parts heather;
- 3 parts hawthorn;
- 2 parts hops.
Important! Before starting treatment with folk remedies, you should consult your doctor, because many herbs can cause allergic reactions.
Ventricular asystole
Ventricular asystole is cessation of electrical and mechanical activity of the ventricles, usually of the entire heart, cardiac arrest. Ventricular asystole leads to cessation of blood circulation and clinical death.
Etiology and pathogenesis. Ventricular asystole is usually caused by severe cardiac
- acute (myocardial infarction, pulmonary embolism) or chronic (ischemic disease
heart disease, hypertension, heart defects, myocarditis, myocardial dystrophy, myocardiopathy, heart surgery), the effects of myocardial depressing antiarrhythmic drugs, excessive vagotonia, reflex effects, electric shock, electric pulse treatment.
In the origin of cardiac
Hypoxia and hypercapnia are of greatest importance. At the same time, the pH of the blood decreases, which causes conduction disturbances up to cardiac arrest. An increase in the tone of the vagus nerve, leading to asystole when the blood pH decreases, also plays a certain role.
Electrolytes are important. Thus, rapid infusion of potassium solutions can lead to asystole.
Along with this, hypokalemia can cause cardiac arrest (more often with intoxication with cardiac glycosides). At the same time, in response to the action of cardiac glycosides, myocardial excitability sharply increases.
Clinic. Ventricular asystole leads to a sudden disappearance of the pulse (not only in the radial artery, but also in the carotid artery), heart sounds, and blood pressure. After a few seconds, the patient loses consciousness, turns pale, and stops breathing. 45 s after the cessation of cerebral circulation, the pupils begin to dilate, reaching a maximum after 1 min 45 s, convulsions, involuntary urination and defecation appear. The electrocardiogram shows a straight line (no electrical activity of the heart).
Diagnostics. It should be borne in mind that circulatory arrest and clinical death are more often associated with ventricular fibrillation than with asystole. And the latter is often preceded by ventricular fibrillation. The clinical picture is the same in both cases. Differentiation can be made only by observing the electrocardiogram on the monitor or by recording the electrocardiogram curve. With asystole, there is no electrical activity of the heart, and therefore a straight line is recorded; with ventricular fibrillation, large or small random biphasic waves are recorded.
Treatment: external cardiac
and artificial respiration - should be started immediately after the first clinical signs of ventricular asystole appear. If the patient was not under electrocardiographic monitoring and there is no certainty that this is not ventricular fibrillation, ventricular defibrillation should be performed. If asystole is diagnosed, electrical stimulation of the heart is necessary as soon as possible. If cardiac stimulation is not possible, 0.5-1 ml of 0.1% adrenaline solution and 5 ml of 10% calcium chloride solution are injected intracardially, norepinephrine, sodium bicarbonate (150-200 ml of 5% solution) are administered intravenously.
The prognosis for ventricular asystole is usually unfavorable. Mortality in certain diseases (for example, heart attack
myocardium) reaches 90-95%.
Prevention of ventricular asystole consists of timely and active treatment
diseases that cause it. The risk of early relapse can be reduced by intramuscular administration of ornid (bretylium tosylate) 0.3-0.6 g every 6 hours. If long-term use for prophylactic purposes is necessary, beta-blockers are the drugs of choice: anaprilin (Inderal, Obzidan) 0.02 -0.04 g, oxprenolol 0.04-0.08 g, cordan 0.05 g 3-4 times a day.
All information on the site, including recipes, is posted and distributed “as is” and does not encourage you to take any action. The site administration is not responsible for the correct description of medications and recipes; one incorrectly defined symptom can lead to an error. We strongly recommend that you consult your doctor.
Consequences
Ventricular extrasystole type 1, according to the classification given above in the article, is not life-threatening and usually does not cause any complications. With type 2 ventricular extrasystole, complications may develop, but the risk is relatively low.
If the patient has polymorphic extrasystoles, paired extrasystoles, unstable paroxysmal tachycardia or early group extrasystoles, there is a high risk of life-threatening consequences:
- Stable ventricular tachycardia is characterized by prolonged (more than half a minute) attacks of group ventricular extrasystoles. This, in turn, provokes the consequences shown later in this table.
- Ventricular flutter Contraction of the ventricles at a rate of 220 to 300 beats per minute.
- Ventricular fibrillation (flickering) Chaotic contractions of the ventricles, the frequency of which reaches 450 beats per minute. The fibrillating ventricles are unable to pump blood, so the patient usually loses consciousness due to lack of oxygen to the brain. This condition, if left untreated, can cause death.
- Asystole (cardiac arrest) May occur against the background of an attack of ventricular arrhythmia or suddenly. Often, asystole inevitably leads to death, since doctors are not always able to perform resuscitation within a few minutes after cardiac arrest.
To avoid life-threatening consequences, do not delay starting treatment if you are diagnosed with ventricular extrasystole.
Where is the source of extrasystoles located?
Ventricular extrasystoles occur in the wall of the left or right ventricle, most often directly in the fibers of the conduction system. If extrasystole occurs at the end of the ventricular relaxation phase, then it coincides in time with the next contraction of the atria. The atrium does not empty completely; a reverse wave travels through the vena cava.
Typically, ventricular extrasystoles cause contraction only of the ventricles themselves and do not transmit impulses in the opposite direction to the atria. “Supraventricular” refers to extrasystoles from ectopic foci located above the level of the ventricles, in the atria, and atrioventricular node. They can be combined with ventricular ones. There are no pancreatic extrasystoles.
The correct rhythm from the sinus node is maintained and disrupted only by compensatory pauses after extraordinary beats.
The order of occurrence of impulses must not be disturbed
Forecast
With a benign course and the absence of an underlying cardiac disease, the prognosis is favorable.
With a potentially malignant type and in the presence of organic damage to the heart, the prognosis is relatively unfavorable and is determined not only by the characteristics of ventricular extrasystoles according to ECG monitoring (frequent, average, paired, group), but also by the nature of the underlying disease and the stage of heart failure, in the later stages of which the prognosis is not favorable . With a malignant course, the prognosis is unfavorable due to the very high risk of sudden cardiac death.
Taking antiarrhythmic drugs in combination with beta blockers can improve the prognosis, since the combination of these drugs not only improves the quality of life, but also significantly reduces the risk of complications and death.
Modern forecasting
Over the 40 years of existence, the above classifications have helped train doctors and enter the necessary information into automatic ECG interpretation programs. This is important for quickly obtaining research results in the absence of a specialist nearby, in the case of a remote (in rural area) examination of the patient.
To predict dangerous situations, it is important for a doctor to know:
- if a person has ventricular extrasystoles, but there is no confirmed heart disease, their frequency and location do not matter for the prognosis;
- the risk to life is increased for patients with heart defects, organic changes in hypertension, myocardial ischemia only in the case of a reduction in the strength of the heart muscle (increasing heart failure);
- The risk for patients after myocardial infarction should be considered high if there are more than 10 ventricular extrasystoles per hour of observation and a reduced volume of blood ejection is detected (extensive infarction, heart failure).
The patient should consult a doctor and be examined for any unclear interruptions in heart rhythm.
Prevention of the disease
The following are usually offered as preventative recommendations:
- maintaining a more active and mobile lifestyle;
- giving up bad habits, including smoking, excessive consumption of alcohol and strong coffee;
- regular medical examinations.
Detection of a disease can occur even during a routine preventive examination; for this reason, a health check in a medical institution is a mandatory event for everyone.