Are rapid heartbeats, chest pain and shortness of breath preventing you from living a full life? Arrhythmia may be the cause of your discomfort. Arrhythmia is disturbances in heart rhythm that occur as a result of other disorders in the body.
The normal heart rate for a person under the age of 60 is 60-80 beats per minute. The heart muscle contracts at regular intervals, so a person gets used to it and does not notice his heartbeat. Deviations from the norm are accompanied by a rapid pulse and irregular contractions. Or it may be completely asymptomatic. Therefore, the presence of arrhythmia and its type can only be determined using instrumental diagnostics. Arrhythmia occurs more often in men over 60 years of age. However, in rare cases it also occurs in children.
Diagnosis of arrhythmia
Arrhythmias are common and usually harmless. Sometimes cardiac arrhythmias are not felt by the patient.
- A doctor can detect arrhythmia during a routine clinical examination:
- The patient himself accidentally detects an arrhythmia when measuring blood pressure with an automatic tonometer.
- In most cases, a person is bothered by a feeling of palpitations and interruptions in the chest “it beats, then it doesn’t beat,” a very fast heart beat (tachycardia), an extremely slow heart beat, dizziness, loss of consciousness, or a feeling close to fainting.
- Sometimes arrhythmia is accompanied by shortness of breath and chest pain.
Even such significant symptoms of ill health do not always indicate a serious problem. However, we must remember that in a healthy person with a healthy heart, the development of a stable arrhythmia is impossible without the presence of a triggering moment.
Symptoms as a way to recognize the disease
Most qualified medical staff are convinced that it is quite difficult for a person to feel any changes in the heartbeat. But most likely, this opinion is due to the fact that the average person is simply not aware of what these or other changes mean. Surely it would not hurt anyone to learn about the main signs that are characteristic of arrhythmia.
As a rule, the pressure during arrhythmia decreases, and accordingly, weakness and dizziness are felt. Moreover, it is possible to acquire a pre-fainting state, which you can think about if your eyes get dark during the slightest movement or change of position. It is noted that uncharacteristic changes in the functioning of the heart entail a chain reaction of the body as a whole.
For example, due to untimely, insufficient oxygen saturation of the blood, breathing occurs unevenly. And inadequate oxygen enrichment of all structural and elementary units of the body leads to strange noises in the head and pain under the rib on the left side, which are also signs of arrhythmia.
Sign up for a consultation
The situation is more serious with people who suffer from a congenital type of heart or circulatory system pathology. If arrhythmia occurs at low pressure, the patient can easily faint, and there is also an increased level of sweating and a feeling of catastrophic lack of air.
Along with the inhibition of heart contractions, uneven breathing is noted, general weakness and the skin turns pale.
All symptoms are long-term and of a sluggish nature. In this regard, people often simply ignore them, but it is arrhythmia that in most cases contributes to cardiac arrest, and as a result, the death of the patient.
It is noteworthy that, despite the fact that arrhythmia does not cause virtually any discomfort, it is, in fact, a very life-threatening illness.
Causes of arrhythmia
The most common causes of arrhythmia are heart disease:
- cardiac ischemia;
- congenital and acquired heart defects;
- myocarditis;
- high blood pressure;
- diabetes;
- obesity;
- thyroid diseases;
- organs of the gastrointestinal tract.
More often, arrhythmia develops in old age.
- Smoking provokes arrhythmia;
- excessive consumption of alcohol and caffeine;
- drug abuse;
- stress;
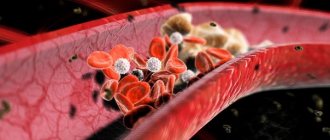
- electrolyte disorders of the blood.
In some cases, the causes of arrhythmias may be an overdose of medications, the use of dietary supplements and herbal preparations.
There are congenital arrhythmias caused by pathology of the system that conducts electrical impulses through the heart. In this case, arrhythmia develops at an early age and occurs suddenly for no apparent reason, and it can only be eliminated surgically.
Causes of arrhythmia, regardless of its type
As already mentioned, this disease is expressed by a violation of the following indicators: frequency, rhythm, sequence of compression of each of the chambers of the heart. And the reasons for this are:
- smoking and alcohol abuse;
- addiction to coffee;
- too much physical activity;
- insufficient or excess potassium in the heart;
- disease of the nervous system, on which the interaction of systems and organs depends;
- diabetes mellitus;
- disruptions in metabolic processes;
- curvature of the spine, as well as stress, depression, emotional shock and mental.
I want to know the cost of treatment
In addition to all this, diseases and defects of the heart muscle of congenital origin are important, and this also applies to the circulatory system and digestive organs. You must always understand that each case is individual, and the real cause can most likely only be determined by a qualified doctor. This is followed by the appointment of adequate therapy.
Arrhythmia and tachycardia are dangerous diseases
Arrhythmia and tachycardia are dangerous both as diseases that lead to heart rhythm disturbances, and as tachycardia itself, since arrhythmia can have a damaging effect on the heart (deplete the heart muscle, disrupt the functioning of the heart valves, cause an increase in the size of the heart cavities) and cause progressive heart failure. In addition, atrial fibrillation - atrial fibrillation - is the cause of every fifth ischemic stroke. An ischemic stroke in a patient with atrial fibrillation often ends in death and, compared with a stroke of another nature, leads to the most severe disability and is more likely to recur. There are arrhythmias, the symptoms of which are dangerous, even life-threatening; Most arrhythmias, having appeared once, progress; and advanced cases are difficult to treat. That is why the patient needs to consult a specialist if there is any suspicion of arrhythmia.
Currently, the doctor has diagnostic and therapeutic techniques that make it possible to identify, control and eliminate arrhythmias. To prevent the disease, it is necessary to lead a healthy lifestyle, eat right and exercise.
Ways to restore rhythm
Treatment can be carried out in various ways, it all depends on its form. One can even say more, the positivity or negativity of the prognosis directly depends on the location of the arrhythmia, it could be:
- area on the atrium vault;
- atrium;
- ventricle
If the arrhythmia greatly bothers the patient, then he is prescribed antiarrhythmic drugs. Today there is no universal remedy that could cure any type of disease. Therefore, in some situations it is necessary to try several drugs until a more suitable one is found.
In turn, such medications can have side effects, moreover, if they are used incorrectly, they can worsen the situation. When drug therapy does not help, and there is a threat to life, a method such as electrical cardioversion, or as it is also called, defibrillation, is used. For a number of cases of arrhythmia treatment, pacemakers are also used, which are surgically inserted under the skin. Alternatively, radiofrequency catheter ablation is widely used.
Any of these methods will be most effective if you consult a doctor in a timely manner. Therefore, you should not neglect the health of your body and the signals it can give.
Our specialists
Shcherbakova Lyudmila Aleksandrovna
The doctor is a cardiologist of the highest category. Candidate of Medical Sciences.
Experience: 23 years.
Gabrielyan Julietta Grigorievna
The doctor is a cardiologist of the highest category. Candidate of Medical Sciences. Experience: 25 years
Logacheva Olga Alexandrovna
The doctor is a cardiologist of the first category. Functional diagnostics doctor. Experience: 17 years.
Roshchina Ekaterina Anatolevna
Functional diagnostics doctor of the second category. Ultrasound diagnostics doctor. Cardiologist. Experience: 15 years.
Arterial hypertension and atrial fibrillation.
Vladimir Trofimovich Ivashkin , academician of the Russian Academy of Medical Sciences, Doctor of Medical Sciences:
– Well, now I will ask Oksana Mikhailovna Drapkina to continue our conference without interruption. Oksana Mikhailovna prepared a lecture “Arterial hypertension and atrial fibrillation.” Please, Oksana Mikhailovna.
Oksana Mikhailovna Drapkina , professor, doctor of medical sciences:
– I will also rely on the results of the latest recommendations on arterial hypertension and, according to these recommendations, arterial hypertension is defined as an increase in blood pressure above 140 and 90 mmHg, and the time interval has changed when we can talk about arterial hypertension as stable. Previously, it was 2 weeks, if a patient comes to us with high blood pressure, now we monitor the patient for 2 months and can already say that we have hypertension.
Regarding the prevalence of arterial hypertension, these recommendations also contain certain figures. This is one in three patients, somewhere between 30-45% of the general population, and there are differences in average blood pressure values between countries.
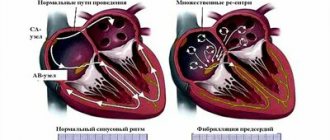
Yuri Aleksandrovich also touched upon and dwelled on the numbers that we must know in order to rank arterial hypertension according to optimal, normal, high normal and, accordingly, arterial hypertension of the 1st, 2nd, 3rd degree and isolated systolic arterial hypertension. Indeed, these recommendations already include levels of evidence and stratification of cardiovascular risk. A new column has appeared, a new line - these are three or more risk factors separately. Diabetes mellitus and chronic kidney disease occupy a completely separate position. Well, today I had the chance to talk about arterial hypertension and atrial fibrillation. Indeed, there is a separate chapter that is devoted to this condition, this complication or concomitant condition of arterial hypertension, and this chapter provides definitions and recommendations, but does not provide an understanding of why atrial fibrillation occurs with arterial hypertension. Experts note that even with high normal blood pressure, atrial fibrillation may develop. But the question arises: “Why?” After all, if we are talking about arterial hypertension, its friend, its ally and complication - left ventricular hypertrophy, then we can predict that it is ventricular arrhythmias that will be more characteristic of these patients. But no. It turns out that in the proportion of atrial fibrillation and its causes, the first place is given to arterial hypertension. And this diagram, not a recommendation, sheds a little light on the cause-and-effect relationship. So, we have before us a patient with arterial hypertension and, as a rule, as a consequence, with diastolic heart failure, that is, he has shortness of breath and preserved ejection fraction. And look at how many negative consequences both atrial and ventricular cardiomyocytes can experience in this patient.
Let me start with the fact that in the atria, cardiomyocytes practically cannot hypertrophy, they degenerate, and they lead to fibrosis occurring in the atria. This leads to heterogeneity in the conduction of the electrical impulse. And here you are, your heart is already prepared for atrial fibrillation. Atriomegaly itself or, for example, a large left ventricle, the pressure in it increases. In order to overcome this change in the pressure gradient, the pressure increases and atriomegaly occurs in the left atrium - this leads to mechano-electrical changes also in the conduction pathways, and here again atrial fibrillation.
Hypertrophy often occurs with arterial hypertension and a violation of not only the uptake, but also the excretion of calcium. And here trimetazidine can be useful, because working on calcium ATP phases, the so-called serka, the pump that pumps calcium out of cardiomyocytes, also leads to disruption of the conduction of electrical impulses, and here is a vicious circle when fibrillation generates fibrillation.
Let's get back to the recommendations. What do the experts tell us? They divide this combination of arterial hypertension with atrial fibrillation into prevention in terms of treatment and rhythm maintenance. Today I will be more interested in prevention, and here experts recommend drugs that affect the activity of the renin-angiotensin-aldosterone system, beta blockers or mineralocorticoid receptor antagonists.
When it comes to rhythm control, beta blockers and non-dihydropyridine calcium channel blockers come first, which makes sense since both reduce heart rate.
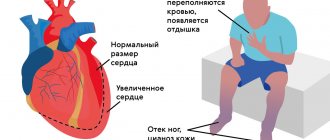
And here it is, as it were, an unkind heart. An unkind heart is a hypertrophied heart. It is shown schematically here. We see a thickened posterior wall of the left ventricle, the interventricular septum. We see a decrease in the lumen, that is, the chambers do not enlarge, and we can almost certainly say that this is a consequence of poorly treated or poorly corrected arterial hypertension, since, please note, everything is normal with the right ventricle. It is not hypertrophied, it is not dilated, that is, the entire shock falls on the left ventricle.
And here I would like to connect atrial fibrillation with left ventricular hypertrophy. This is where the dog is buried. This is why we see atrial fibrillation so often in patients with hypertension. There are two “responses” of the myocardium to damage – atrophy or hypertrophy. Today we are more concerned about the second. And how the myocardium will behave when damaged depends on whether protein synthesis predominates or protein breakdown predominates. If protein synthesis is regulated by many different enzymes, then protein breakdown - a very interesting indicator - is regulated mainly by an agent such as atrogin-1. And we see that with hypertrophy, protein synthesis prevails over breakdown and, conversely, with atrophy, protein synthesis is subordinate to protein breakdown.
And the mediators of hypertrophy are the same as the mediators of fibrosis. Dear colleagues, we have had a whole educational series about fibrosis not only of the heart, but also the molecular mechanisms of fibrosis in general, and we still see the same players - angiotensin II, aldosterone, norepinephrine and prorenin. It is very important to remember here that even if we blocked, say, angiotensin II with angiotensin receptor blockers or with ACE inhibitors, the synthesized renin and prorenin will still lead to hypertrophy, in particular, of the left ventricle.
Let's dive a little deeper into left ventricular hypertrophy and look at the molecular pathways of hypertrophy, and then return to the host level. So there are two main ways. Combining together, angiotensin II, increased endothelin and a slight mechanical stretch, when the chamber begins to dilate a little, leads to the fact that alpha-1 adrenergic receptors begin to activate, this in turn leads to an increase in NAD oxidase and the kinase cascade is launched. When the synthesis of those same proteins occurs, hypertrophy of cardiomyocytes occurs and, in addition to hypertrophy, something that does not work occurs completely in parallel, the same pump from the artoendoplasmic calcium ATP phase of the sercus, which is responsible for pumping out calcium and, accordingly, for reducing calcium contracture. And here it is a small chamber with thick walls, the so-called concentric hypertrophy. But, if the myocardium takes a different path - the path of serious stretching, that is, dilatation of the chamber, this leads to the fact that the basic mechanisms begin to affect the mitochondria, and here the cell takes the path of apoptosis, when the release of cytochrome C already occurs like an avalanche, it is exfoliated from the mitochondria. Here the caspase cascade is activated, and apoptosis of cardiomyocytes occurs.
At the macroorganism level, we can say that at the molecular level we have now briefly examined the formation of concentric and eccentric hypertrophy of the left ventricle. Accordingly, concentric hypertrophy of the left ventricle is based on pressure overload, and eccentric hypertrophy of the left ventricle is based on volume overload, as, for example, it happens with various regurgitations, oral, for example, regurgitation, and so on. Extracellular and intracellular signaling pathways are approximately the same.
And here is the continuum of cardiovascular diseases that is well known to us, at the beginning of which is hypertension, together with obesity, diabetes, and, perhaps, this path ends with chronic heart failure, which often brings the patient to our hospital bed.
If we look at electron microscopy of cardiomyocytes, we see that cardiomyocytes behave differently at different stages of left ventricular hypertrophy. Small myofibrils are already appearing, there are mitochondria, and you see how the mitochondria gradually increase in size with increasing hypertrophy. And this is what a patient with severe hypertrophy demonstrates. There are absolutely no well-readable z-stripes, respectively, this myocardium will not be able to contract normally, we see a large amount of extracellular matrix, and we see a large number of myofibrils, and the architecture of the contractile myocardium completely changes.
Thus, the fate of a hypertrophied cardiomyocyte at the basis of arterial hypertension, and, as we said, one of the consequences of atrial fibrillation, is unenviable: either it takes the path of apoptosis, samurai style, or the path of necrosis.
It is very important to analyze the relationship between the extracellular matrix and the cardiomyocyte in determining which path the cardiomyocyte will take. The extracellular matrix is a terribly interesting system, it is constantly in motion, processes of either synthesis or, conversely, degradation of collagen occur there all the time, and all this is also controlled by the relationship between matrix metalloproteinases and their inhibitors.
It is interesting, or even surprising, but a fact: it turns out that with left ventricular hypertrophy, the average size of the cardiomyocyte does not increase, but even decreases, and it is the specific gravity of the extracellular matrix that increases. This was demonstrated in one very elegant work by our colleagues from the Almazov Institute.
Now, pay attention, this is an atrial cardiomyocyte. And we see under the letter A - a histological study of a patient with a permanent form of atrial fibrillation, the middle one, letter B - this is a paroxysmal form of atrial fibrillation and C - this is a healthy myocardium. Please note that the average diameter of cardiomyocytes when it is a healthy myocardium is 15 µm. If a patient has atrial fibrillation, and he came to it through hypertrophy, then the average size of cardiomyocytes decreases, and the density of capillaries increases and the fraction of fibrosis increases. Accordingly, the main message of my speech today is that the composition of hypertrophy must necessarily include fibrous changes. Accordingly, the beneficial effects of ACE inhibitors and ARBs that we see in reducing left ventricular hypertrophy and preventing atrial fibrillation are probably largely related to their effect on fibrosis, that is, with their antifibrotic properties.
Thus, inflammation and fibrosis are the substrate of atrial fibrillation. And the basic mechanisms of development of atrial fibrillation and its relationship with atrial fibrosis are analyzed.
First, structural remodeling occurs with the participation of fibrous changes. Together with electrical remodeling, a substrate for atrial fibrillation is provided. The degree of fibrosis and the persistence of atrial fibrillation correlate. And even when the ventricular rate is controlled, rapid activation of the atria stimulates the development of atrial fibrosis.
Where do these processes take place? First of all, they begin to occur in the atrium, and you see that the most profibrogenic factor, the so-called growth factor TGFβ, can be activated both with the help of angiotensin II - the left edge of this figure, and with the help of large mechanical stretching, that is, the dilatation of the chamber itself will lead to the fact that the processes of fibrinogen and fibroformation are started and it becomes very difficult to stop them.
The main signaling pathways that are involved in the development of atrial fibrosis have been revealed. In addition to what I said, the intimate connections between angiotensin II and transforming growth factor, here we must remember about connective tissue growth factor and platelet growth factor.
Thus, we can say that angiotensin II dramatically reduces the activity of matrix metalloproteinases and the implementation of the effects, namely the stimulation of TGFβ, is not all that angiotensin II does. This stimulation of effects extends beyond the activation of collagen synthesis, for example, angiotensin II is involved in the transformation of fibroblasts into myofibroblasts, and they are extremely aggressive agents that begin to synthesize extracellular matrix proteins. And the production of connective tissue growth factor is also activated.
Accordingly, there is every reason to believe that agents that block the renin-angiotensin-aldosterone system may also reduce fibrosis. This has been demonstrated in many experimental models. I want to say that this has been demonstrated in clinical practice, for example, by the work of Professor Tatarsky, who has been studying atrial fibrillation for a long time, and even now, he showed that not only antiarrhythmic drugs can reduce the incidence of atrial fibrillation, but also in his works it was lisinopril, and when taking lisinopril, the frequency of atrial fibrillation paroxysms, their tolerability, and their duration decreased.
We also analyzed some data on this issue, in particular, a study was done called “Conductor”. We saw that, against the background of adequate antihypertensive therapy, left ventricular hypertrophy decreased and diastolic heart failure increased or improved, in particular, against the background of Diroton and Co-Diroton also showed the same results. Therefore, we can also say with a certain degree of assumption that this may be due to the influence of these agents on the antifibrotic processes. Both these processes and these effects are summarized on this slide. We see that ARAs and angiotensin-converting enzyme inhibitors can reduce left ventricular hypertrophy and, consequently, wall stiffness, optimize diastolic function, reduce pressure in the left atrium - all this will lead to inhibition of atrial remodeling and fibrosis and, accordingly, reduce the risk of developing paroxysms of fibrillation atria.
And, in fact, what have we come to? This is my final slide - “Management of patients with arterial hypertension and atrial fibrillation.” This is, after all, first of all, control of blood pressure, we have many helpers, this includes changing lifestyle and reducing salt intake, necessarily an agent that will influence the renin-angiotensin-aldosterone system. Secondly, we know a little less about this, but still, it will probably develop very rapidly - this is the prevention or treatment, one might say, of fibrosis. And finally, reducing oxidative stress. Thank you for your attention.
Read also
Cardiac ischemia
Coronary heart disease is a disease that can begin at an early age and remain asymptomatic for decades.
The disease is characterized by damage to the coronary arteries due to a violation... Read more
Relevance of high cholesterol
The normal course of all physiological processes in the body is determined not only by the proper activity of all organs and systems, but also by the state of lipid metabolism. Disruption of this process is practically...
More details
The problem of myocardial infarction
Myocardial infarction remains a very significant social problem. This condition leaves quite serious consequences, which in almost all cases lead to disability. In other cases…
More details
Coronary artery bypass grafting
The concept of coronary artery bypass grafting This surgical intervention is one of the first and most effective approaches to the treatment of heart disease. After the intervention, patients feel improvement...
More details
Heart failure
What is Heart Failure? Heart failure occurs when the myocardium cannot pump blood properly. Certain conditions such as narrowing of the blood vessels in the heart...
More details
Types of arrhythmia:
Atrial fibrillation.
An abnormal heart rhythm during which the atria contract faster than the ventricles. This is a complication due to coronary heart disease. Diseases of the endocrine system can also cause the development of atrial fibrillation. Unlike normal heartbeat, muscle fibers in atrial fibrillation are excited frequently and chaotically. In addition to frequent contractions of the heart muscle, the disease is accompanied by increased sweating, darkening of the eyes, muscle weakness and fainting.
Sinus arrhythmia.
During the disease, the sinus node, the main “engine” of impulses in the heart, is damaged. Because of this, the sinus node begins to malfunction. With sinus arrhythmia, an alternation of rapid and slow rhythm occurs. A common type of sinus arrhythmia occurs, in which during inhalation the heart rate increases, and when exhaling, on the contrary, it decreases. This disease is also called respiratory arrhythmia. The pathology is accompanied by dizziness, severe fatigue, breathing problems, and loss of consciousness.
Atrial flutter.
This is a rapid atrial rhythm, reaching 200-400 beats per minute. The reasons for the deviation may be complications after other cardiovascular diseases, the postoperative period, severe stress, or pathological processes in the body. Accompanied by symptoms such as general weakness, discomfort in the chest or behind the sternum, shortness of breath and sudden attacks of rapid heartbeat.