09/19/2017 Olga Migunova 0 comments
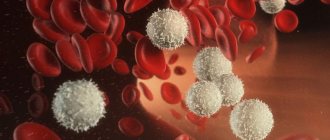
Monocytes are a type of white blood cells (leukocytes) that are responsible for protecting the human body from tumor cells and pathogenic microorganisms, as well as for the resorption and elimination of dead tissue. Thus, these cells cleanse the body, which is why they are also called “janitors”.
The clinical significance of monocytes in a blood test is that their level can suggest the presence of a particular disease. Experts recommend that both adults and children undergo a general blood test twice a year for prevention in order to promptly identify deviations from the norm.
Today we want to tell you why a child may have elevated monocytes and who to contact in this case.
Functions of monocytes in the body
In the medical literature you can also find other names for monocytes, for example, mononuclear phagocytes, macrophages or histiocytes.
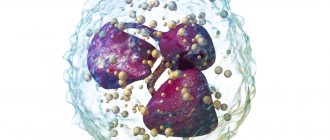
Macrophages are one of the main immune cells. Their role for the body is to fight pathogenic microorganisms (viruses, bacteria, fungi), waste products of microbes, dead cells, toxic substances and cancer cells.
Macrophages remain working in the pathological focus even after neutralizing the foreign agent in order to process dead pathogenic microorganisms and decayed tissues of the body, due to which they are called “orderlies”, “cleaners” or “janitors” of the body.
In addition, macrophages prepare the body for recovery by enclosing the lesion with a “wall” that prevents the spread of infection to intact tissues.
The norm of monocytes in the blood of children: table
In most cases, the relative number of monocytes in the blood is determined, that is, the number of a given type of leukocyte is indicated as a percentage (%) in relation to other types of white blood cells.
| Child's age | Monocyte count, % |
| from 0 to 28 days | from 3 to 12 |
| from 1 month to a year | from 4 to 10 |
| from 1 to 15 years | from 3 to 9 |
| teenagers | from 1 to 8 |
As you can see, the levels of monocytes in the blood change with the age of the child.
Also, the doctor who ordered a general blood test may require the laboratory technician to provide the absolute number of monocytes, which also depends on the age of the child.
| Child's age | Monocyte count, g/l |
| up to 12 months | from 0.05 to 1.1 |
| 1-2 years | from 0.05 to 0.6 |
| 3-4 years | from 0.05 to 0.5 |
| Over 4 years old | from 0.05 to 0.4 |
Leukocytes or white blood: evolution of the immune system
Leukocytes are different. Some are responsible for fighting bacteria, others deal with viruses, others “specialize” in very large adversaries - for example, in plant cells (this happens more often than you think - I mean an allergy to pollen) or even in multicellular scoundrels - worms.
So looking at the total white blood cell count during an acute infection is good, but damn low. At best, the doctor will determine that there is an infection. But to understand what exactly caused this infection, you need to look at which leukocytes are elevated. This study is called the leukocyte formula.
That's what we'll talk about.
Norms
The main changes in the red blood of children occur not only up to a year, but up to a month, and this is due to the fact that during the first month of life, traces of the transition to lung breathing still remain in the child’s blood. With the immune system, everything is much more complicated - it changes continuously during the first six years of life, and extremely unevenly. So, get ready: there will be more numbers.
Leukocytes . They are WBC. Their number is measured in billions per liter of blood (which, compared to red blood cells, seems somehow frivolous). And since at birth a child moves from a sterile environment (the mother’s womb) to an extremely unsterile environment, the number of leukocytes, even normally, in children is much higher than in adults. True, it decreases with age. In a one-month-old child, the normal rate of leukocytes in the blood is from 6.5 to 13.8, at six months from 5.5 to 12.5, from one year to six years (yes, at the very time when the child most often gets sick) from 6 to 12. And only when the child’s immunity becomes strong enough to withstand numerous infections, the number of leukocytes approaches the number in adults - from 4.5 to 9 (some for some reason consider 12 to be the norm, but this is not entirely true).
Neutrophils , also known as NEU. Their number is counted not in absolute units (how many per liter of blood) but as a percentage of the total number of leukocytes. The task of these cells is to fight bacteria. It's a pretty fair fight: neutrophils simply eat the unwary bacterial cells and digest them. True, in addition to bacterial cells, neutrophils also act as a kind of cleaners - in exactly the same way they remove any cellular debris from the body, not just microbes.
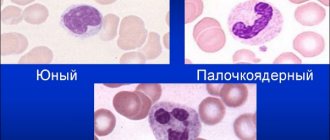
There are different neutrophils: there are band neutrophils (these are a kind of juniors among the eater cells), but there are not very many of them in the blood - things like destroying infections are not a child’s task. Their number almost does not change with age: in a one-month-old, one-year-old, and even a six-year-old child, it is from 0.5 to 4.5%. Only in children over seven years of age (as, indeed, in adults) the upper limit of the norm for band neutrophils rises to 6%. The child has grown, the body has become stronger - the immune system is ready for invasion.
But the real “workhorses” of the immune system are segmented neutrophils - by the way, they are the main and almost the only protection for children under 2 years of age. In children under one year of age, the normal number is from 15 to 45%, and from one to six years of age (when work increases significantly), the number of neutrophils increases significantly - from 25 to 60%. Finally, by the age of seven, the number of segmented neutrophils reaches the adult norm. True, this norm is very vague - from 30 to 60%. That is, thirty percent is the norm, and sixty is the norm too.
Monocytes , also known as MON. These are the “younger brothers” of neutrophils . For the time being, they sit in the tissues, and only rarely emerge into the blood. Normally, their number does not exceed 2 to 12% in children under one year old or from 2 to 10% in children over one year old. Adults and children are no different in this indicator - still the same 2-10%. True, when there is a catastrophic shortage of neutrophils monocytes and the number of monocytes in the blood, although not greatly, increases.
Eosinophils , also known as EOS. It is rumored that eosinophils are responsible for allergic reactions. To put it mildly, this is not entirely true. Eosinophils do not produce class E immunoglobulins, the level of which is increased in allergy sufferers. Eosinophils , if you like, are the “highest caste” of eater cells (before this, we talked about neutrophils and monocytes as eater cells). They are able to devour everything that is not capable of consuming themselves. Even multicellular aggressors (worms) and very large foreign cells (for example, intestinal amoebas) are desperately afraid of eosinophils . The fact is that eosinophils do not swallow cells - they stick to them, inject their digestive enzymes into the cells and then suck out the contents of these cells, like a child sucking out a liter carton of juice. Just turn away - and all that remains from the package (in our case, from a small worm, for example) is an empty shell. Normally, eosinophils in the blood - from 0.5 to 6%
Lymphocytes , also known as LYM. These are the main cells of the mature immune system. Their specialization is the fight against both viruses and bacteria. But especially recklessly, lymphocytes deal either with viruses or with their own cells, which, due to the naivety of these viruses, have sheltered. Normally, the blood of a child under one year of age lymphocytes , although they work, to be honest, at half capacity. But when the baby’s immune system begins to develop (I remind you, the development of the immune system after a year and ends mainly by 6-7 years), the number of lymphocytes in the blood drops quite sharply - to 26-60%. Finally, after 7 years, lymphocytes “stop” at around 22-50%.
Basophils, BAS. Just young lymphocytes. Their number never exceeds 1%.
All. Uf-f-f-f...
Advertising
Level of monocytes in the blood: how to determine?
The content of monocytes in the blood is determined using a general blood test. This study allows you to count the total number of all white blood cells and calculate the leukocyte formula.
The leukocyte formula is the percentage of individual types of white blood cells, such as neutrophils, basophils, lymphocytes, monocytes and eosinophils. Changes in the leukocyte formula are markers of various diseases.
Blood for analysis is taken from a child’s toe or heel, depending on his age, and in rare cases, from a vein.
Average cost of analysis in Russia
A general clinical blood test with calculation of the leukocyte formula can be done free of charge under the compulsory medical insurance policy at your medical organization.
You can also get tested for a fee. On average, a general clinical blood test along with a leukocyte count will cost between 400 and 600 rubles. You can only request a white blood cell count. Such a study will cost 250–350 rubles.
I would recommend examining the level of leukocytes along with a general clinical blood test. The indicators together help to choose the right direction for further diagnostic measures.
How to prepare for a general blood test?
The well-known television pediatrician Komarovsky focuses in his program on a general blood test on the fact that the objectivity of the results depends on the correct preparation for the study, so it is important to observe the following principles:
- blood is donated exclusively on an empty stomach, since after eating the white blood cells in the blood increase. If a blood test is performed on an infant, the interval between the last feeding and the blood draw should be at least two hours;
- the day before blood sampling, the child must be ensured calm and protected from stress, as well as from physical activity and active games;
- It is not recommended to give your child fatty foods on the eve of a blood test;
- If the child is taking any medications, this should be reported to the doctor who referred him for a blood test, since some drugs can provoke monocytosis.
What to do if deviations from the norm are detected?
First of all, don’t panic or get upset. It is worth showing your test results to a competent doctor.
A hematologist specializes in blood tests and more. He will be able to answer all your questions, give competent advice, and prescribe a proper examination of the body.
To further examine and search for the true causes of abnormal monocyte levels, specialists resort to various studies: from X-ray examination to studying the material obtained after bone marrow puncture. The main thing is to promptly identify breakdowns that have occurred in the body (both in adults and children) and prescribe adequate treatment.
What is monocytosis?
Monocytosis is an increase in the level of monocytes in the blood, which can be determined by a general blood test.
Monocytosis is not a separate nosological form, but a symptom of many diseases.
Elevated monocytes in a child, depending on the reasons, can be accompanied by a variety of symptoms, namely:
- general weakness;
- fast fatiguability;
- increased body temperature;
- cough;
- nasal congestion;
- swollen lymph nodes;
- stomach ache;
- nausea and others.
It is customary to distinguish between absolute and relative monocytosis.
Absolute monocytosis is diagnosed when there is o.
With relative monocytosis, there is an increase in the percentage of monocytes against the background of a normal number of leukocytes due to a decrease in the number of other types of white blood cells.
Diagnostics
The level of monocytes is measured during the calculation of the leukocyte formula in a clinical blood test. Detection of monocytosis requires consultation with a medical specialist, preferably a therapist. The doctor must conduct a survey of the patient’s complaints, collect anamnestic data, and perform a general examination to identify signs of a particular disease. The data obtained serve as support for prescribing additional examination to determine the cause of monocytosis:
- Blood tests
. In a general blood test, the total number and percentage of all forms of leukocytes (leukocyte formula) are calculated, and the ESR is determined. The blood smear checks for the presence of atypical mononuclear cells. The level of autoantibodies (to DNA, muscle cells, topoisomerase), antigranulocyte antibodies, and CRP is examined. Immunohistochemical analysis and immunophenotyping of cells are performed to identify surface-specific or tumor CD markers. - Microbiological Research
. To identify the infectious pathogen, bacteriological culture and sputum microscopy are performed. The method of enzyme immunoassay and polymerase chain reaction determines antibodies to viruses, bacteria, and their DNA. Serological tests are carried out (indirect hemagglutination reactions, microprecipitation reactions). - Radiography
. In tuberculosis and sarcoidosis, X-rays of the lungs reveal an increase in the mediastinal and hilar lymph nodes; in histiocytosis, bilateral small-focal opacities are detected. Histiocytosis is also characterized by areas of osteolysis and destruction on radiographs of the flat bones of the skull and long tubular bones. - Sonography
. During ultrasound of the abdominal cavity in patients with infectious mononucleosis, brucellosis, and oncohematological diseases, splenomegaly and, less commonly, hepatomegaly are observed. Echocardiography in patients with collagenosis sometimes reveals thickening of the pericardial layers and effusion into the pericardial sac. - Histological studies
. In case of malignant blood diseases, a large number of blast cells are detected in a bone marrow smear obtained by sternal puncture or trepanobiopsy. Microscopic examination of bronchoalveolar fluid in patients with histiocytosis reveals giant Langerhans cells with eosinophilic cytoplasm. In a lymph node biopsy for lymphomas, proliferation of lymphoid cells and Berezovsky-Sternberg cells are detected.
Laboratory diagnosis of monocytosis
Elevated monocytes in a child’s blood: reasons
The following diseases can lead to an increase in monocytes in children:
- Infectious mononucleosis;
- brucellosis;
- malaria;
- toxoplasmosis;
- roundworm infestation;
- syphilis;
- lymphoma;
- leukemia;
- rheumatoid arthritis;
- systemic lupus erythematosus;
- inflammation of the mucous membrane of the digestive tract (gastritis, enteritis, colitis and others);
- intoxication with phosphorus or tetrachloroethane.
Monocytosis can also be detected in children who have had an infectious disease, removal of tonsils, adenoids, as well as during the period of teething and changing teeth.
Monocytes are elevated in a child: examples of interpretation of the results of a general blood test
Of clinical significance is not only the increased content of monocytes in the blood, but also the combination of monocytosis with deviations of other hematological parameters. Let's look at examples.
- Lymphocytes and monocytes are increased. The combination of lymphocytosis and monocytosis can often be observed in children with acute viral infections, childhood infectious diseases and indicates the viability of the immune system. In cases where, against the background of elevated monocytes, lymphocytes are reduced, a weakening of the immune system can be assumed, since these cells are responsible for cellular immunity.
- Monocytosis and eosinophils are increased. This combination of indicators is characteristic of pathological processes of an allergic and parasitic nature. Monocytosis and eosinophilia can be detected in the blood of children suffering from atopic dermatitis, hay fever, bronchial asthma, ascariasis, giardiasis, etc. In rare cases, such changes can occur as a result of more serious diseases such as leukemia and lymphoma.
- Basophils and monocytes are increased. The main role of basophilic leukocytes is the destruction of foreign agents (viruses, bacteria, fungi), and this type of cell is the first to migrate in areas of inflammation. Basophils and monocytes can simultaneously increase in diseases of allergic or autoimmune origin.
- An increase in monocytes in a child against the background of high neutrophils. This combination is quite common and occurs in diseases caused by various bacteria and sometimes fungi. Also in such cases, lymphopenia is often observed.
- Increased monocyte count and high ESR (erythrocyte sedimentation rate) . Erythrocytes, or red blood cells, are cells that carry oxygen on their surface from the lungs to organs and tissues. Various infectious, allergic or autoimmune diseases affect erythrocyte sedimentation, in most cases accelerating it.