Hypothyroidism is a hormonal disease in which the thyroid gland does not produce enough hormones. Most often it affects older women. Hypothyroidism and cholesterol levels are closely related. An increase in sterol concentration almost always accompanies a deficiency of thyroid hormones. Therefore, the latest medical protocols recommend that all people with high cholesterol levels check their thyroid health.
Why is cholesterol dangerous?
Your doctor has probably warned you about cholesterol, a fatty, waxy substance that circulates in your blood. Too much of the wrong type of cholesterol can clog your arteries and put you at risk for heart disease.
High cholesterol may be a result of your diet, especially if you eat foods high in saturated fat, such as red meat and butter. Sometimes, however, your thyroid gland may be to blame. Too much or too little thyroid hormone can cause cholesterol levels to rise or fall.
In this article, you will learn how your thyroid gland affects cholesterol.
Diet for hypothyroidism caused by Hashimoto's
The diet for hypothyroidism caused by Hashimoto's disease requires some changes. Patients suffering from autoimmune thyroiditis are advised to increase their intake of omega-3 fatty acids due to their anti-inflammatory properties, and to take vitamin D and B12 supplements due to the high risk of pernicious anemia.
Vitamin D supplement
The diet should also be rich in healthy protein, which should account for 25% of daily energy needs.
Patients with Hashimoto's disease are advised to undergo diagnostic tests for celiac disease, as the diseases often coexist. Sometimes doctors recommend that patients go on a gluten-free diet regularly, as this can help alleviate the autoimmune process.
ONLINE REGISTRATION at the DIANA clinic
You can sign up by calling the toll-free phone number 8-800-707-15-60 or filling out the contact form. In this case, we will contact you ourselves.
If you find an error, please select a piece of text and press Ctrl+Enter
What is the thyroid gland?
Your thyroid gland is a butterfly-shaped gland in your neck. It produces hormones that control metabolism. Metabolism is the process by which your body converts food and oxygen into energy. Thyroid hormones also help the heart, brain, and other organs function normally.
At the base of the brain is the pituitary gland, which directs the activity of the thyroid gland. When your pituitary gland detects that you have low thyroid hormone levels, it releases thyroid-stimulating hormone (TSH). TSH directs the thyroid gland to produce more hormones.
What to eat for hypothyroidism?
So what should you eat if you have hypothyroidism? Fish is an excellent source of iodine in the diet. Most of this element contains cod (100 mcg of iodine per 100 g), salmon (50 mcg / 100 g) and mackerel (45 mcg / 100 g). Iodine is also present in mineral water, but not in all its types, so you should keep an eye on the label when looking for this element.
Table salt is also a source of iodine, as many countries have passed legislation requiring salt manufacturers to iodize table salt. Selenium, in turn, is found in grain products, meat, fish, dairy products, eggs and vegetable sprouts.
Iodized table salt
In general, the diet for hypothyroidism should be properly balanced. Healthy protein should make up 15% of your daily energy needs, complex carbohydrates 55%, fats 30% (with 20% unsaturated fatty acids and saturated fats maximum 10%).
Dietary fiber should be an important part of the diet because constipation is very common in patients suffering from hypothyroidism. It is recommended to consume 25-40 grams of dietary fiber per day.
About cholesterol
Cholesterol is found in every cell of your body. Your body uses it to produce hormones and substances that help digest food.
Cholesterol also circulates in your blood. It enters the bloodstream in two forms of lipoproteins:
- High-density lipoprotein (HDL) cholesterol is good for your heart. They help remove cholesterol from the body and protect against heart disease.
- Low-density lipoprotein (LDL) cholesterol is bad for your heart. If LDL cholesterol levels are too high, the cholesterol can clog arteries and contribute to heart disease, heart attacks and strokes.
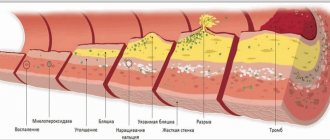
Myth No. 4. High cholesterol levels in the blood provoke atherosclerosis.
Actually: YES
An increase in cholesterol concentration—hypercholesterolemia—is a reliable fact of the development of atherosclerosis. High risks of atherosclerosis of the coronary arteries are observed already at values above 5.2-6.5 mmol/l (200-300 mg/dl) - this is a border zone or risk zone. Indicators of 6.5-8.0 mmol/l indicate moderate, and above 8.0 mmol/l indicate severe hypercholesterolemia. A level of less than 5.2 mmol/L (200 mg/dL) is considered safe. In this case, the risk of atherosclerosis is minimal.
Underactive or overactive thyroid
Sometimes the thyroid gland can produce too little or too much hormone.
A condition in which the thyroid gland does not work effectively is called hypothyroidism. When the thyroid gland is weakened, the entire body feels that it is working slowly. You become tired, lethargic, cold and sore.
An underactive thyroid may develop if you have the following conditions:
- Hashimoto's thyroiditis, an autoimmune disease in which the body attacks and destroys the thyroid gland
- inflammation of the thyroid gland (thyroiditis)
Other factors that can lead to underactive thyroid:
- removal of all or part of the overactive thyroid gland
- radiation for cancer or an overactive thyroid gland
- some medications such as lithium, interferon alpha, and interleukin-2
- damage to the pituitary gland from a tumor, radiation, or surgery
Hyperthyroidism is a condition that occurs when the thyroid gland is overactive. When the thyroid gland is overactive, the body begins to work faster. Your heart rate increases, and you feel nervous and trembling.
Hyperthyroidism may develop if you have:
- Graves' disease, an immune system disorder that runs in families
- toxic nodular goiter, which includes lumps or nodules on the thyroid gland
- inflammation of the thyroid gland (thyroiditis)
How does the thyroid gland cause cholesterol problems?
Your body needs thyroid hormones to make cholesterol and get rid of cholesterol it doesn't need. When thyroid hormone levels are low (hypothyroidism), the body does not break down and remove LDL cholesterol as efficiently as usual. LDL cholesterol can build up in the blood.
Thyroid hormone levels do not have to be very low to raise cholesterol levels. Even people with moderately low thyroid levels, called subclinical hypothyroidism, may have higher LDL cholesterol levels than normal. A 2012 study found that high TSH levels alone can directly increase cholesterol levels, even if thyroid hormone levels are not low.
Hyperthyroidism has the opposite effect on cholesterol levels. It causes cholesterol levels to drop to abnormally low levels.
It is known that hypothyroidism is caused by a persistent decrease in the effect of thyroid hormones on target tissues, which is associated with a lack of thyroid hormones in the body or a decrease in their biological effect at the tissue level [3, 4]. Thyroxine (T4) and triiodothyronine (T3) secreted by the thyroid gland regulate protein synthesis and influence the metabolic and functional activity of nervous system structures [8]. The key component of thyroid hormones is iodine. The synthesis of thyroid hormones is regulated by thyroid-stimulating hormone (TSH), which is synthesized in the anterior pituitary gland. The formation of TSH decreases under the influence of glucocorticoids and increases under the influence of estrogens. The level of TSH is regulated by the structures of the hypothalamus with the participation of somatostatin and dopamine. It is subject to circadian fluctuations and can change under the influence of environmental factors, such as ambient temperature. The inhibitory effect is realized under the influence of the serotonergic system of the brain. TSH is present in many parts of the central nervous system and itself has the ability to inhibit the bioelectrical activity of neurons.
Hypothyroidism occurs in the population in 0.2-2% of cases, among the elderly - in 2-4%, and in women 3 times more often than in men [3, 4, 16]. Women aged 40-60 years are especially susceptible to this disease; the prevalence rate among women in the older age group reaches 12% [3]. Subclinical hypothyroidism (increased TSH levels without any clinical symptoms) is observed in 7.5-10% of women and 3% of men [3, 8, 23].
Hypothyroidism can be caused by various reasons: congenital changes in the thyroid gland (hypo- or aplasia), its surgical removal, pituitary dysfunction. However, in adults it is more often a consequence of autoimmune processes. Chronic autoimmune thyroiditis occurs in 3-4.5% of individuals in the general population. The biosynthesis of thyroid hormones is disrupted by drugs such as amiodarone, sulfonamides, and lithium preparations [15]. Sometimes hypothyroidism is accompanied by other endocrine disorders.
In a significant proportion of cases, hypothyroidism is associated with iodine deficiency. WHO recommends a daily iodine intake of 150 mcg for adults, 200 mcg for pregnant and lactating women, and 50 to 120 mcg for children. With a daily iodine intake of less than 50 mcg, the thyroid gland begins to produce less hormones than required, which is clinically manifested as hypothyroidism. Almost one billion people worldwide are thought to be at risk of developing iodine deficiency disorders [17]; Almost 13% of the population has iodine deficiency [15]. These are mainly countries in Asia and Africa, where there is no iodine in water and food or its consumption in the form of iodized salt is insufficient [15]. In areas where there is iodine deficiency, the incidence of hypothyroidism is 10-20 times higher.
Pathogenesis
The pathogenesis of clinical disorders in hypothyroidism is based on metabolic disorders caused by a sharp decrease in the production of a number of cellular enzymes due to a deficiency of thyroid hormones [3, 15]. This leads to a decrease in metabolic processes and a slowdown in redox reactions. In this case, mucinous edema (myxedema) of the tissue develops [3]. Disturbances in the metabolism of glycosaminoglycans, which have increased hydrophilicity of protein breakdown products (protein derivatives, glucuronic and chondroitinsulfuric acids), lead to infiltration of the mucous membranes, skin and subcutaneous tissue, muscles, and myocardium [3]. Cerebral hypoxia occurs, contributing to the development of episodes of confusion and syncope. In the pathogenesis of cognitive disorders in this category of patients, certain importance is attached to neurotransmitter disorders, caused, in particular, by the influence of thyroid hormones on the acetylcholinergic system [10, 22]. In this regard, it should be noted that thyroid pathology is detected in 38% of patients with frontotemporal dementia, and hypothyroidism is a risk factor for the development of Alzheimer’s disease [22]. Even in a euthyroid state, in clinically healthy older adults, there is a relationship between lower levels of thyroid hormones (within normal values) and decreased cognitive function. Reduced cerebral blood flow, cerebral hypoxia, cerebral edema and hyponatremia are also of pathogenetic significance. The influence of thyroid hormones on electrolytes and blood pressure occurs through the reticular activating system [15]. Even a slight decrease in the level of thyroid hormones in the blood can lead to severe cognitive impairment [15].
Thyroid hormones play a very important role in the development of the nervous system. In particular, when they are deficient during pregnancy, the development of the nervous system in the fetus is disrupted, which is manifested by cortical hypoplasia, delayed myelination processes and slowed formation of cerebral vessels. If hypothyroidism is not corrected in the early postnatal period, these changes become irreversible. However, if hypothyroidism occurs in adults, then changes in the nervous system are less pronounced and usually reverse with treatment.
Clinical manifestations
The most common clinical manifestations of hypothyroidism are increased fatigue, general weakness, drowsiness, decreased appetite, weight gain, hypomia, and impaired tolerance to low ambient temperatures [3, 8, 16]. Patients often complain of constipation, muscle and joint pain, especially headaches (it should be noted that headaches in these cases often disappear with adequate hormone replacement therapy for hypothyroidism).
The listed symptoms of hypothyroidism are very nonspecific. In this regard, hypothyroidism is often diagnosed months and even years after the onset of its first symptoms [8]. Signs such as weight gain (even against the background of decreased appetite), baldness and slowness of movement are often taken as signs of “normal” aging, and hypomimia is a manifestation of depression or parkinsonism. Since depression can develop with hypothyroidism, diagnostic errors regarding this form of affective disorders become less obvious [5]. In addition, according to some data, subclinical hypothyroidism is often detected in patients with depression [5]. It has therefore been suggested [5] that thyroid function testing is mandatory in any depressed patient who does not respond to antidepressant therapy.
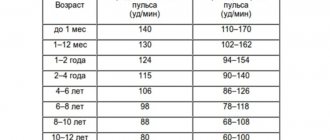
In patients with hypothyroidism, sweating decreases and the skin becomes dry. The hair on the body changes until it is completely lost, especially in the pubic area and in the outer third of the eyebrows. There is swelling of the hands and feet. The appearance of patients changes, which is largely due to swelling of the eyelids and face. Hoarseness and articulation disorders are quite characteristic, which is caused by infiltration of glycosaminoglycan into the vocal cords and tongue. The pulse often drops to 60 beats per minute or less. There may be an expansion of the borders of the heart, but heart failure rarely develops. Echocardiography may reveal pericardial effusion. Against this background, aggravation (or occurrence) of pain such as angina pectoris may occur. Hypercholesterolemia, characteristic of hypothyroidism, increases the risk of developing vascular diseases. With hypothyroidism, women often experience heavy periods and infertility.
Neurological and mental disorders, which have been known since the end of the 19th century, range from mild disorders of higher cerebral functions, peripheral myoneuropathy and pathology of the cranial nerves to psychoses, ataxia, paroxysmal disturbances of consciousness (syncope, epileptic seizures) and coma [1, 5, 8] .
Hypothyroidism may not be accompanied by neurological symptoms for several years. The development of neurological disorders is characterized by an insidious onset and slow progression [25]. In these cases, the presence of increased fatigue and drowsiness often does not attract the proper attention of either the doctor, the patient himself or people close to him and relatives.
In some cases, the disease begins acutely with the onset of seizures. At one stage or another of the disease, they are observed in 20-25% of patients with hypothyroidism [5]. It is important to note that anticonvulsants do not lead to thyroid dysfunction [5]. A rare debut of hypothyroidism is acute psychosis, occurring with visual and auditory hallucinations. It is believed that hypothyroidism as a cause of the disease should be taken into account when making a differential diagnosis in any patient with sudden onset mental disorders, depression or hallucinations [15].
With untreated hypothyroidism, in approximately 1% of cases, a coma quickly develops (often accompanied by epileptic seizures). In these cases, in addition to hypothermia, arterial hypotension, bradycardia and rare breathing are noted [5]; the prognosis is often unfavorable, with the cause of death in most cases being cardiac arrhythmia. Pathomorphological examination reveals only severe cerebral edema, and in the most severe cases, diffuse neuronal damage [5]. Older women are most susceptible to developing a coma during the winter season [15].
For patients with hypothyroidism, vestibuloatactic disorders are quite common [1, 4]. Cerebellar dysfunction occurs in 5-10% of patients [5, 16]. Most often, it manifests itself as gait disturbances in the form of a gait with legs wide apart, tandem walking is impaired, and patients often experience impaired coordination in the limbs, tremor, dysarthria and nystagmus. The basis of such disorders is probably atrophy of the anterior parts of the cerebellar vermis, which, however, (with adequate therapy) is reversible [5].
Neuromuscular disorders in the form of neuropathies and dysmetabolic myopathy are very characteristic disorders of hypothyroidism and occur in 30-80% of patients (differences in the figures given depend on the severity of hypothyroidism). With therapy, these disorders may regress. The main manifestation of hypothyroid myopathy is a slowdown in muscle contraction and relaxation. Microscopic examination of the muscles reveals local necrosis of muscle fibers and basophilic degeneration of skeletal muscles. In rare cases, muscle hypertrophies are detected, reminiscent of those in Hoffman syndrome. Severe muscle weakness is rare, but mild disorders are observed in almost 40% of cases [12]. The proximal limbs are most often affected [19, 20]. Myopathic syndrome in hypothyroidism can occur with both muscle atrophy and hypertrophy [4]. The severity of muscle weakness increases at low temperatures. However, much more often, patients experience muscle cramps, pain and paresthesia, usually in the proximal limbs, as well as reduced tolerance to physical activity [14, 16]. There is also a description in the literature [6] of “treatable dropped head syndrome” in hypothyroidism, as well as myopathy in acute hypothyroidism (with its development within 2-6 weeks) [18]. In the blood serum of patients with hypothyroid myopathy, increased levels of creatine phosphokinase (CPK) may be detected [4, 14, 16]. This is especially typical for cases occurring with muscle weakness in the proximal extremities, however, no correlation of increased CPK with the severity of muscle weakness was noted [12].
In some cases, patients with hypothyroidism may exhibit myasthenic syndrome with corresponding changes in the EMG.
An association between hypothyroidism and fibromyalgia has been noted [26]. It has been suggested that fibromyalgia is a form of hormone-resistant hypothyroidism. However, it should be noted that during therapy for hypothyroidism, there is a decrease in the severity of pain caused by fibromyalgia.
The presence of hypothyroidism is an important factor in the development of dystrophic changes in the spine, which is associated with impaired synthesis of collagen, which is part of the disc structure [4]. Therefore, for this category of patients, it is quite typical to have pain in various parts of the spine, impaired mobility, pain in the spinous processes and paravertebral points, and the occurrence of tension symptoms [4].
Damage to peripheral nerves is one of the characteristic manifestations of hypothyroidism [2, 16, 17]. In this case, damage to sensory fibers develops at earlier stages of the disease, when there are no changes in the propagation of excitation along motor fibers [11], however, there is evidence indicating a more frequent involvement of motor fibers in the pathological process [13]. The most common (14-81% of patients) complaint is paresthesia [17]. Paresthesia may be based on tunnel syndrome (for example, carpal tunnel syndrome), the presence of which is noted in 70% of patients [4]. Its development is associated with the deposition of mucopolysaccharides in the skin and around peripheral nerves [5]. A significant decrease in axonal regeneration in conditions of thyroid hormone deficiency may also be important [4]. The most common tunnel syndrome in hypothyroidism is carpal tunnel syndrome - in 10-35% of patients [5, 12, 16]. As a rule, it is bilateral in nature. However, in clinical practice there may be situations when existing disorders on one side do not manifest clinical symptoms [5]. A feature of tunnel neuropathies is their multiple, combined nature [4].
One of the typical manifestations of nervous system pathology in hypothyroidism is also demyelinating polyneuropathy [16]. Polyneuropathy caused by hypothyroidism is characterized by a decrease in reflexes and the development of muscle weakness; in addition, patients may experience a decrease in vibration sensitivity and muscle-joint sense. According to electron microscopy, there are ultrastructural changes in the endoneurial vessels [9]. Damage to peripheral nerves can be detected by electromyography even in patients without neurological symptoms [13]. Changes caused by segmental demyelination are manifested by a decrease in the speed of propagation of excitation along the nerve fiber. In this case, damage to peripheral nerves can be observed even with subclinical hypothyroidism [17]. Under the influence of hormone replacement therapy, the corresponding symptoms may undergo reverse development. Experimental studies [24] have established a positive effect of thyroid hormones on the condition of nerve fibers and the regeneration of nerve tissue.
The pathogenesis of peripheral (including cranial) neuropathies, in addition to compression, is based on other factors, including microcirculation disorders and metabolic neuronal disorders. Sensorimotor axonal polyneuropathy occurs in 40-90% of patients [4, 12].
Pyramidal symptoms occur rarely, but decreased deep reflexes are one of the characteristic (in 85% of patients) signs of hypothyroidism. Despite the normal process of muscle contraction, there is a significant prolongation of the muscle relaxation phase [5, 8]. This phenomenon is detected in more than 2/3 of patients with hypothyroidism. It should be noted that similar changes can occur with hypothermia, edema of the extremities, diabetes mellitus, parkinsonism, neurosyphilis, sarcoidosis and pernicious anemia. In hypothyroidism, reflexes are normalized with hormone replacement therapy.
Hypothyroidism can also cause damage to the II, V, VII, VIII pairs of cranial nerves [5]. Quite often various ophthalmological disorders develop. Thus, with primary hypothyroidism, there may be loss of visual fields due to an enlargement of the pituitary gland. It is possible to develop pseudotumor, leading to swelling of the optic discs. This syndrome mainly occurs in children a few weeks after the start of hormone replacement therapy, but similar cases have been described in adults [5]. Rare manifestations include uveitis and ptosis. With hypothyroidism, typical and atypical trigeminal neuralgia is sometimes detected. Peripheral facial paresis may also develop. There is evidence [5] about damage to the VIII pair of cranial nerves (although some researchers do not confirm this). Tinnitus and hearing loss, probably caused by damage to the cochlea, may regress with therapy. Patients with hypothyroidism receiving L-thyroxine may also experience a decrease in taste, accompanied by a burning sensation in the mouth [5].
Cognitive and mental disorders can vary from slow mental functions and mild mnestic disorders (in some cases resembling the initial manifestations of Alzheimer's disease) to severe psychotic disorders occurring with illusions and hallucinations [5]. In severe cases, patients become apathetic, the speed of mental processes decreases sharply, and speech slows down. In the neuropsychological status, in addition to memory and attention disorders, disorders of constructive praxis and visual-spatial functions are revealed. This category of patients is characterized by sleep apnea, both central and peripheral, and in the second case, improvement can be obtained with hormone replacement therapy [4, 5].
Cretinism, a term that was proposed at the beginning of the 19th century. to designate severe encephalopathy in hypothyroidism, develops when pathology occurs in early childhood (even from the moment of birth). In these cases, we are usually talking about congenital absence of the thyroid gland, congenital metabolic disorders, iodine deficiency during pregnancy and in the early postpartum period. However, the onset of clinical symptoms can be “delayed” by hormones received from the mother. It should be noted that the prevalence of congenital hypothyroidism has decreased significantly due to the introduction into clinical practice of appropriate methods of early diagnosis and adequate therapy [15]. However, studies in adolescents, even after correctly and actively treated congenital hypothyroidism, report impairments in memory, attention, and visuospatial functions [15].
Mild cases of iodine deficiency encephalopathy currently occur in almost 50 million children worldwide, resulting in an average reduction in IQ of 15 points [15]. In the cognitive sphere, this category of patients exhibits memory and attention impairments, apathy, drowsiness, depression, as well as behavioral disorders [15]. Selenium deficiency, which accompanies iodine deficiency, also plays a role in the pathogenesis of neurological disorders in cretinism. In patients with cretinism, in addition to mental retardation, a decrease in body weight, pathology of dental development, thinning of the tongue, a protruding abdominal wall (usually with the presence of an umbilical hernia) and bone abnormalities are usually detected. The neurological status also often reveals deafness, pyramidal and sometimes extrapyramidal symptoms, and strabismus. Pyramidal symptoms in the form of muscle rigidity are more often detected in the lower extremities, and revitalization of knee reflexes is often noted. Unfortunately, therapy for already developed cretinism with neurological disorders is ineffective. Therefore, it is so important to start hormonal treatment immediately after the birth of a child with signs of hypothyroidism or if the possibility of its development is suspected.
In patients with hypothyroidism, an increase in gamma globulins in the blood serum and cerebrospinal fluid (CSF) is often detected, and in 40-90% of patients there is an increase in total protein in it. CSF pressure is usually not elevated in hypothyroidism. According to the EEG, there is a decrease in -activity. X-ray or magnetic resonance computed tomography (CT or MRI) of the brain shows mild cerebral atrophy. In hypothyroidism associated with an autoimmune process, reversible diffuse changes in the white matter of the cerebral hemispheres can also be detected [15].
Diagnostics
Diagnosis of hypothyroidism is carried out on the basis of anamnestic data, the results of a clinical study and the identification of a low free thyroxine index, the identification of primary hypothyroidism is based on the determination of an elevated TSH level. Secondary (associated with pituitary dysfunction) and tertiary (associated with hypothalamic dysfunction) hypothyroidism is characterized by the presence of a low level of TSH in combination with low levels of T3 and T4.
Making a differential diagnosis between secondary and tertiary hypothyroidism is challenging and not always possible. For this purpose, a thyroid-releasing stimulation test is used - intravenous administration of 400 mcg of thyroid-releasing hormone with determination of the level of TSH in the blood serum initially and 30 and 60 minutes after administration. Normally, the TSH level increases 2 times compared to the original level. This indicates normal functioning of the pituitary gland and allows one to suspect hypothalamic dysfunction as the cause of hypothyroidism. Another method that helps in the differential diagnosis of these two conditions is an MRI of the brain with a detailed assessment of the pituitary gland and hypothalamus.
Prevention and treatment
Prevention of hypothyroidism in areas with iodine deficiency involves adding iodine to food, in particular in the form of iodized salt [15]. To treat hypothyroidism, L-thyroxine and, in some cases, oral triiodothyronine are used. In most cases, adults require 100 to 150 mcg of L-thyroxine per day; To treat coma, L-thyroxine is administered parenterally [15].
Treatment begins with small doses of the drug and gradually increases over the course of months, achieving a euthyroid state [15]. It should be noted that the effectiveness of such therapy in the presence of severe neuromuscular disorders in patients with hypothyroidism is significantly lower than in patients with thyrotoxicosis [12]. With adequate treatment of hypothyroidism, patients may experience positive changes in the cognitive sphere [7, 21]. Therefore, dementia in patients with hypothyroidism is considered a potentially reversible condition (although relevant epidemiological and placebo-controlled clinical studies have not been conducted) [25].
What are the symptoms?
You may have an underactive thyroid gland if you notice the following symptoms:
- weight gain
- slow heartbeat
- increased sensitivity to cold
- muscle pain and weakness
- dry skin
- constipation
- problems remembering or concentrating
An overactive thyroid gland has exactly the opposite symptoms:
- weight loss
- fast heartbeat
- increased sensitivity to heat
- increased appetite
- nervousness
- shake
- more frequent bowel movements
- sleep problems