Vasculitis ( angiitis, arteritis ) is a general name for a group of diseases associated with inflammation and destruction of the walls of blood vessels. Inflammation of blood vessels can occur in any organ.
The disease vasculitis leads to the fact that the vessels cease to properly perform their function (supplying blood to tissues and removing metabolic products), so the organs adjacent to them are affected.
Vasculitis has different classifications and may differ in localization, etiology and severity of the clinical picture. Some vasculitis affects only the skin, while others affect vital organs.
Left untreated, vasculitis can result in serious complications. Intestinal and pulmonary bleeding, thrombosis, renal failure, liver failure, heart attack - this is not a complete list of the dangerous consequences of the disease. Vasculitis can lead the patient to disability and even death.
1 Consultation with a rheumatologist
2 Consultation with a rheumatologist
3 Consultation with a rheumatologist
General information
Vasculitis (a synonym for this name is the term angiitis ) is the name for a heterogeneous group of diseases, the basis of which is an immunopathological inflammatory process affecting the blood vessels. It affects different vessels - arteries, arterioles, veins, venules, capillaries. The consequence of this disease is changes in the functions and structure of the organs that the affected vessels supply with blood. The disease can provoke bleeding, necrosis , and ischemia .
Scientists are still conducting research, trying to more accurately determine vasculitis - what kind of disease it is, and what reasons lead to its development. The exact causes of the disease are still not known. It is assumed that the disease develops due to the influence of external factors in combination with a genetic disposition. There is also evidence that the disease can be caused by hepatitis virus or Staphylococcus aureus . The ICD-10 code is I77.6.
Vasculitis - what is this disease?
Vasculitis (lat. Vasculum) is the collective name for a group of vascular diseases characterized by inflammation and destruction of the walls of blood vessels - arteries, capillaries, veins and others.
Synonyms for vasculitis are angiitis, arteritis.
By the nature of the pathology, vasculitis resembles atherosclerosis - it is based on thickening of the vessel wall, which reduces the lumen of the bloodstream, disrupts blood circulation, as well as the normal blood supply to one or another part of the body or organ.
Blood, in addition to delivering nutrients to all organs, also delivers oxygen to them. Naturally, due to circulatory disorders, “starving” organs malfunction, and if there is a complete interruption in the supply of blood to them, they begin to die.
The causes of vasculitis are still (as of 2021) not fully understood. There are only assumptions, for example - a combination of genetic features (predisposition), infection (staphylococci, hepatitis viruses) and unfavorable environmental factors.
The classification of vasculitis includes a large number of types and forms, however, depending on the cause, they are divided into primary (an independent disease) and secondary (appears against the background of other diseases). According to localization, there are vasculitis on the skin, in which other organs are not damaged, and internal, the consequences of which can be not only serious cardiovascular diseases, but also death.
By form, the most popular are urticarial, allergic, skin, systemic and hemorrhagic vasculitis.
Vasculitis - ICD
ICD-10: I77.6, I80, L95, M30-M31; ICD-9: 446, 447.6.
Pathogenesis
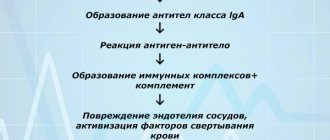
Work is still underway to study the etiology of systemic vasculitis. In particular, there is an opinion about the likely role of bacterial or viral infection in its development. The pathogenesis of the disease is complex, including a number of immune mechanisms. The following factors are believed to play a role in the development of systemic vasculitis:
- The formation in the body of autoantibodies to antineutrophil cytoplasmic antibodies, during which activation and adhesion of neutrophils to endothelial cells occurs, which leads to their damage.
- Formation of autoantibodies to antigens .
- Formation of pathogenic immunocomplexes and their deposition into the vascular wall. Which affects polymorphonuclear leukocytes after complement activation. In turn, they produce lysosomal enzymes that damage the vascular wall. Its permeability increases. thrombosis often occurs .
- Immune system reactions associated with the action of T lymphocytes . This mechanism is decisive in the development of Wegener's granulomatosis . Due to interaction with the antibody, sensitized T-lymphocytes produce lymphokines that inhibit the migration of macrophages. Next, they concentrate them where antigens accumulate. Macrophages are activated and produce lysosomal enzymes, which leads to damage to the vascular walls. These mechanisms lead to the manifestation of granuloma.
- The direct influence of various infectious agents on the vascular wall.
- Vasospastic and coagulation disorders.
- Effects resulting from the release of inflammatory mediators and cytokines.
- Processes of interaction between leukocytes and endothelial cells, resulting in the release of a large number of reformed and newly synthesized adhesive molecules.
- The appearance of antibodies to phospholipids. Such antibodies are found in patients with systemic vasculitis. Their cross-reaction with endothelial proteins is noted, which leads to an increase in the coagulating properties of the blood.
Types and classification of vasculitis
Vasculitis is divided into types:
- primary;
- secondary;
- systemic.
In the first case, we are talking about an independent and still just beginning disease. The second type may appear with other pathologies, for example, tumors. It can also occur as a reaction to an infection. Systemic vasculitis can occur in different ways. It leads to inflammation of blood vessels and damage to their walls, and tissue necrosis cannot be ruled out. Without proper treatment, complications usually occur, including death.
Based on the caliber of the affected vessels, a classification of vasculitis was identified. It may be in the form:
- arteritis (affects large vessels);
- phlebitis (affects the walls of the veins);
- arteriolitis (inflames the arteries and arterioles);
- capillaritis (affects capillaries).
Also included in a separate category is vasculopathy, which is characterized by the absence of clear signs of inflammation and infiltration of the vascular walls.
The degree of vascular damage can be mild, moderate and severe.
Classification
First of all, vasculitis is divided into primary and secondary .
- Primary lesions are an independent process in which the vessels become inflamed. Their cause is unknown.
- Secondary are lesions that develop as complications of ongoing infectious or oncological diseases. The cause of such diseases can also be the use of drugs, the influence of toxins , and infectious agents.
Vasculitis photo
In turn, primary vasculitis, taking into account the size of the inflamed vessels, is divided into the following groups:
- Inflammatory process of small vessels: Wegener's granulomatosis , hemorrhagic vasculitis (Henoch-Schönlein purpura), cryoglobulinemic vasculitis , microscopic polyangiitis , hypocomplementary urticarial vasculitis , Churg-Strauss syndrome , hypersensitivity vasculitis.
- Inflammatory process of medium vessels: Kawasaki disease , periarteritis nodosa .
- Inflammatory process of large vessels: giant cell arteritis , Takayasu disease .
- Inflammation of vessels of different sizes: Behçet's disease , vasculitis in Cogan's syndrome .
- Inflammation in systemic diseases: lupus, sarcoidosis, rheumatoid vasculitis.
- Vasculitis of individual organs: primary angiitis of the central nervous system, cutaneous arteritis , isolated aortritis , cutaneous leukocyte-clastic angiitis , others.
Isolated cutaneous vasculitis is also isolated. It can be a manifestation of the following diseases:
- Henoch-Schönlein hemorrhagic vasculitis;
- hypersensitivity allergic vasculitis;
- nodular vasculitis;
- erythema nodosum;
- periarteritis nodosa .
Depending on the caliber of the affected vessels, where exactly they are localized and the type of lesion, a certain clinical picture is present.
The secondary form of vasculitis may be as follows:
- associated with syphilis ;
- with hepatitis B ;
- with hepatitis C ;
- with cancer;
- immune complex, associated with drugs;
- ANCA drug-associated vasculitis;
- other.
Since systemic vasculitis is determined by immune mechanisms, then, depending on the type of immunopathological process, systemic primary vasculitis is divided into the following groups:
- Those associated with immune complexes: lupus and rheumatoid vasculitis, Behçet's disease , hemorrhagic vasculitis , cryoglobulinemic vasculitis .
- Those associated with organ-specific antibodies : Kawasaki disease.
- Those associated with antineurophilic cytoplasmic antibodies: microscopic polyarteritis , Wegener's granulomatosis , classical polyarteritis nodosa , Churg-Strauss syndrome .
Treatment of vasculitis
The effectiveness of treatment for vasculitis largely depends on timely and accurate diagnosis, treatment of affected organs and concomitant diseases. In some cases, the disease goes away on its own, as is the case with primary allergic vasculitis.
Complex therapy for vasculitis includes:
1. Drug treatment; 2. Physiotherapeutic methods of treatment; 3. Diet; 4. Preventive measures (at the end of the article).
Important! Before using medications, be sure to consult your doctor!
Drug treatment of vasculitis
Drug treatment of systemic vasculitis is aimed at the following goals:
- Suppression of immunopathological reactions that are the basis of the disease;
- Maintaining stable and long-term remission;
- Treatment of disease relapses;
- Preventing the development of secondary diseases and complications;
Medicines for vasculitis:
Glucocorticoids are a group of hormonal drugs that have anti-inflammatory, antiallergic, immunoregulatory, anti-stress, anti-shock and other properties. In this case, these hormones play one of the most important roles in the treatment of giant cell arteritis (GCA) and Takayasu arteritis, contributing in many cases to achieving stable and long-term remission. In the case of a very rapid response to glucocorticoids, the response can be considered as an additional diagnostic feature of GCA and polymyalgia rheumatica (PPR).
Among the glucocorticoids we can distinguish: Prednisolone, Hydrocortisone.
Cytostatic drugs (cytostatics) are a group of antitumor drugs that disrupt and slow down the mechanisms, division, growth and development of all cells of the body, which is especially important in the presence of malignant (cancerous) tumors. Also effective for nephritis.
Good effectiveness in therapy should be given to the simultaneous use of cytostatics with glucocorticoids, especially in cases of treatment of vasculitis such as ANCA, urticarial, hemorrhagic, cryoglobulinemic, giant cell arteritis, Takayasu arteritis. The duration of taking cytostatics ranges from 3 to 12 months.
Among the cytostatics we can highlight: Cyclophosphamide, Methotrexate, Doxorubicin, Fluorouracil.
Monoclonal antibodies are antibodies produced by immune cells that have immunosuppressive and antitumor properties and have been shown to be effective against skin cancer (melanoma), breast cancer and lymphatic leukemia. Medicines from the group of monoclonal antibodies are no less effective than cytostatics and are used in the treatment of ANCA vasculitis. The appointment is advisable in case of undesirable use of cytostatic drugs. Contraindications for use are the presence of hepatitis B virus (HBV), a positive intradermal tuberculin test, neutropenia, as well as low levels of IgG (immunoglobulins class G) in the blood.
Among the monoclonal antibodies against vasculitis are: Rituximab.
Immunosuppressants are a group of drugs that suppress the action of the immune system. Prescribed in combination with glucocorticoids.
Among the monoclonal antibodies against vasculitis are: “Azathioprine”, “Mycophenolate mofetil”.
If there are contraindications to Azathioprine, Leflunomide may be prescribed.
"Mycophenolate mofetil" is prescribed as an alternative treatment for patients with refractory or recurrent systemic vasculitis, for example, with kidney damage, however, with an increase in ALT and AST in the peripheral blood by 3 times or more, as well as a decrease in platelets (100×109/l ) and leukocytes (2.5×109/l), the drug is stopped.
Normal human immunoglobulin - prescribed for severe kidney damage, infectious complications, hemorrhagic alveolitis.
Anti-infectious therapy – used for diseases of infectious etiology or concomitant infectious diseases.
If bacteria are present, antibacterial drugs are prescribed - Trimethoprim, Sulfamethoxazole.
Read also Arthritis - symptoms, causes, types and treatment of arthritis
If viruses are present, antiviral drugs are prescribed - Interferon alfa, Vidarabine, Lamivudine.
For hepatitis, drugs are prescribed by a hepatologist, depending on the type of hepatitis virus.
Detoxification therapy – used to bind toxins and biologically active substances, as well as remove them from the body.
The following detoxification drugs can be identified: Atoxil, Nutriclins, Polyphepan, Enterosgel.
Non-steroidal anti-inflammatory non-steroidal drugs (NSAIDs) - are prescribed for persistent and necrotic lesions, thrombophlebitis and nodular vasculitis.
Among NSAIDs one can highlight: Acetylsalicylic acid, Ibuprofen, Indomethacin, Phenylbutazone.
Anticoagulants are a group of drugs that prevent the formation of blood clots in blood vessels.
Anticoagulants include Warfarin and Heparin.
Antihistamine therapy is used if the patient is allergic to medications or foods.
Antihistamines include Diazolin, Claritin, Tavegil, Terfen, and Fenkarol.
Treatment of vasculitis in children also includes transfusion therapy.
Can also be used:
- Hemosorption;
- ACE inhibitors;
- Vasodilators.
2. Physiotherapeutic methods for treating vasculitis
Plasmapheresis – helps improve kidney function, reducing the risk of developing end-stage renal failure.
Diet for vasculitis
The diet for vasculitis is hypoallergenic, which is important if the disease is of an allergic nature.
Products from the highly allergenic group are excluded from the diet - eggs, whole milk, seafood (shellfish), caviar, strawberries, wild strawberries, bananas, melon, mango, persimmon, citrus fruits, tomatoes, carrots, bell peppers, nuts, coffee, cocoa, chocolate, baked goods , industrial canned food, as well as individually intolerable food products.
In case of severe nephritis, diet No. 7 is prescribed, with a further gradual transition to a hypochloride diet. For abdominal syndrome, the use of diet No. 1 is indicated.
Causes
Until now, the causes of the development of this disease have not been studied enough. The causes of the manifestation of the primary form of the disease are determined only tentatively. It can develop due to viral and chronic infections, allergies , chronic autoimmune diseases, taking certain medications and contact with chemicals. The factors that provoke this disease are hypothermia, burns, radiation, trauma, and hereditary factors. However, these phenomena are not the causes of the disease, but its triggering factors.
Causes of vasculitis
As we have already mentioned, the etiology of vasculitis is not fully understood, however, there is confirmed data on some of the causes.
Vasculitis can be caused by:
- Genetic predisposition;
- Infection of the body against the background of weakened immunity;
- Overactivity of the immune system to infection;
- Allergic reaction to certain medications;
- Inflammatory processes in the thyroid gland;
- Autoimmune processes;
- Complications of diseases such as reactive arthritis, glomerulonephritis, Schwartz-Jampel syndrome, systemic lupus erythematosus.
Symptoms of vasculitis
Common clinical symptoms for vasculitis of all types are undulating fever , in which body temperature rises during outbreaks of vascular damage. Skin-hemorrhagic and muscular-articular syndrome are also noted. The peripheral nervous system may also be involved in the pathological process. This leads to the development of polyneuritis. There is also exhaustion and multifaceted visceral lesions.
In the specialized literature, the term “ vasculopathy ” is sometimes used to define signs of vascular damage in this disease.
In general, the symptoms of systemic vasculitis, depending on the type, can be varied and affect different systems and organs. The following manifestations are possible:
- Skin - rashes, ulcers appear, fingers turn blue, ulcers may form in the genital area, gangrene .
- Lungs - shortness of breath , coughing, spitting up blood, episodes of suffocation are possible.
- Nervous system – headache, dizziness , convulsions, impaired sensitivity and motor function, strokes .
- Mucous membranes - the appearance of rashes and ulcers.
- Kidneys – increased blood pressure , swelling.
- Digestive system - diarrhea , abdominal pain, blood in the stool.
- Musculoskeletal system - swelling and pain in the joints, muscle soreness.
- Vision - pain and pain in the eyes, blurred vision, redness of the eyes.
- Heart and blood vessels - cardiac dysfunction, chest pain, blood pressure surges.
- ENT organs - deterioration of smell and hearing, discharge from the ears and nose, hoarse voice, nosebleeds.
Hemorrhagic vasculitis
Photo of vasculitis on the legs
This form is mostly benign. Typically, remission or recovery occurs within a few weeks. However, hemorrhoidal vasculitis can be complicated by damage to the intestines or kidneys. Most often, with this form of the disease, damage to the skin develops. A person is affected by a hemorrhagic rash - palpable purpura , which is faintly visible, but can be identified by touch. At the very beginning of the disease, vasculitis appears on the legs - the rash is localized in the distal parts of the lower extremities, and then moves to the thighs and buttocks.
Also with this form of the disease, articular syndrome is observed. The large joints of the legs are most often affected. Migrating pain in the joints is noted at the time when skin rashes appear. Some patients may experience abdominal syndrome, in which the gastrointestinal tract is affected. In this case, abdominal pain, nausea, vomiting, abdominal pain, and gastrointestinal bleeding are noted. Renal syndrome is also possible.
Cutaneous
With this type of disease, small or medium-sized vessels of the dermis are affected. However, the vessels of the internal organs are not affected. The symptoms of this type of disease are similar to those of a number of skin diseases. In particular, capillary effusions, capillary damage, nodules, and urticaria . If this form accompanies systemic diseases, the patient is also concerned about joint pain and increased body temperature.
Allergic vasculitis
Photos of symptoms of allergic vasculitis
With this form, the patient exhibits erythematous and hemorrhagic spots, rashes, and nodules. A skin infarction is likely when a black crust forms in the area of the rash. At the sites of the rash, burning pain or itching appears. There are hemorrhages under the nails on the toes, muscles and joints hurt. Characteristic signs of the disease can be seen in the photo of allergic vasculitis.
Most often, with this form of vasculitis, a rash appears on the thighs, feet, and legs. If the disease becomes generalized, rashes on the torso and forearms may be bothersome.
This group includes acute and chronic erythema nodosum , erythema induratum of Bazin , temporal angiitis , and Behçet's disease .
The most important symptoms of Behçet's disease are recurrent stomatitis and ulcers on the genitals. Behcet's syndrome also affects the mucous membrane of the eyes and skin. The characteristic symptoms of this type of disease are the formation of ulcers and erosions.
Photo of Behçet's disease
In patients with acute erythema nodosum, large nodules appear, and the color of the skin underneath them changes from red to greenish.
Systemic vasculitis
Speaking about systemic vasculitis - what kind of disease it is, it should be noted that this form of the disease develops in the event of a violation of immune mechanisms in people with a variety of systemic diseases with connective tissue lesions.
With the development of Wegener's granulomatosis, the disease is manifested by the following symptoms: destructive changes in the respiratory tract, vascular walls and kidneys develop; ulcerated granulomas appear on the mucous membranes of the mouth, nose, and bronchi; glomerulonephritis develops . The disease leads to severe complications - internal organs, nervous system, visual organs, and skin suffer.
Autoimmune vasculitis in rheumatism spreads to the body as a whole. Its manifestations depend on the stage of development. An autoimmune type of disease affects the skin, blood vessels of internal organs and the brain. The likelihood of internal bleeding increases.
Cryoglobulinemic vasculitis
This is a type of systemic form of the disease, which is characterized by the appearance of cryoglobulin . They are deposited on the walls of blood vessels and gradually destroy them. A characteristic sign of this disease, which has a progressive form, is damage to peripheral nerves and gradual loss of sensitivity. If treatment is not started promptly, this disease can cause motor paralysis and loss of speech.
Urticarial vasculitis
Photo of urticarial vasculitis
This type of disease is one of the varieties of the allergic form, in which chronic inflammation of the superficial vessels of the skin develops. At the very beginning, such patients are often diagnosed with “chronic urticaria”. The disease progresses in waves. A person develops hemorrhagic nodules, blisters, and spots on the skin. He often feels a burning sensation in the affected areas. The temperature rises, pain in the lower back, joints, muscles, abdomen, and headache. The temperature rises and glomerulonephritis develops.
Periarteritis nodosa
It develops mainly in males. I am worried about muscle pain, weight loss, and fever. Sometimes nausea and vomiting and severe pain in the abdomen appear sharply. The disease can lead to strokes and mental disorders.
Takayasu's disease (nonspecific aortoarteritis)
Takayasu arteritis is a progressive granulomatous inflammatory process of the aorta and its main branches. Nonspecific aortoarteritis (Takayasu's disease) mainly affects young women. About half of patients who develop arteritis suffer from primary physical symptoms. They develop fever, insomnia , fatigue, weight loss, and joint pain. Often nonspecific aortoarteritis leads to the development of anemia and increased ESR.
In approximately half of the patients, preliminary somatic symptoms do not develop, and only late changes in the vascular system are noted. During the development of the disease in its later stages, due to the weakness of the vessel walls, localized aneurysms can develop. The disease also provokes the development of Raynaud's phenomenon . Therefore, it is important that treatment is started as early as possible and that the treatment protocol for patients with Takayasu's disease is strictly followed.
Wegener's granulomatosis
This form causes pain in the paranasal sinuses, ulcers on the nasal mucosa, and ulcerative necrotic rhinitis . Destruction of the nasal septum may occur, leading to a saddle nose deformity. kidney failure develops rapidly shortness of breath , and coughing up blood are noted
Churg-Strauss syndrome
This disease is also called eosinophilic granulomatosis with angiopathy. During its development, blood vessels are affected, as a result of which the blood supply to vital organs deteriorates. The most common symptom of Churg-Strauss vasculitis is asthma . However, in addition to it, other symptoms also appear: fever, rash, bleeding in the gastrointestinal tract, pain in the feet and hands. Sometimes the symptoms are mild, while in other cases severe, life-threatening symptoms develop.
Polymorphic dermal angiitis
Angiitis of the skin photo
This is angiitis, in which chronic recurrent dermatosis develops due to a nonspecific inflammatory process in the walls of skin vessels. During the development of the disease, the skin of the legs is predominantly affected. But rashes can appear in other places. Sometimes their appearance is preceded by general symptoms - fever, weakness, headache. The rash does not go away for several months. After recovery, there is a risk of relapse. There are many varieties of this disease depending on the characteristics of the rash.
Livedo angiitis
It mainly develops in women during puberty. Initially, persistent livedo-cyanotic spots appear on the legs. They appear less frequently in other places. The spots can have different sizes and shapes. When cooled, the severity increases. Over time, small ulcers, necrosis, and hemorrhages may develop at the spots. Patients are concerned about chilliness, pain in the legs, and painful ulcers.
Cerebral vasculitis
A serious disease characterized by the development of an inflammatory process in the walls of blood vessels in the brain. The cerebral form of this disease can provoke hemorrhages and tissue necrosis. As the disease progresses, the patient may experience severe headaches. Epileptic paroxysm and focal neurological deficit are possible. During the development of the disease, one of the following complexes of symptoms is likely to occur:
- multifocal manifestations resembling the clinical picture of multiple sclerosis ;
- acute encephalopathy with mental disorders;
- symptoms characteristic of a brain mass.
Microscopic vasculitis
This form mainly affects small vessels. It is rare and can begin as pulmonary-renal syndrome, which is accompanied by rapidly progressing glomerulonephritis and alveolar hemorrhages . At the very beginning of the disease, general manifestations develop: fever, myalgia, arthralgia, weight loss. Other symptoms depend on which organs and systems are affected. Most often, damage occurs to the kidneys, less often to the skin, respiratory system, and gastrointestinal tract.
Giant cell temporal arteritis
The disease affects older people. Its symptoms are weakness, undulating fever, malaise, severe throbbing headaches, and swelling in the temples.
Tests and diagnostics
During the diagnostic process, the following studies are carried out:
- Blood and urine tests are carried out multiple times. In the process of such studies, in patients with vasculitis, an acceleration of ESR, an increase in fibrinogen , and an increase in C-reactive protein levels are often determined. Leukocytosis may be detected. Blood and urine tests help determine kidney damage.
- Immunogram study. In the process of immunological research, in some forms of vasculitis, antineutrophil cytoplasmic antibodies (ANCA) are determined. This greatly simplifies the diagnosis.
- Allergy testing.
- Instrumental research methods - ultrasound, radiography, echocardiography, etc.
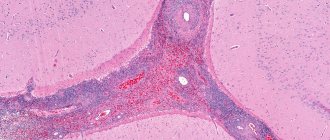
- Biopsy of the affected organ or tissue for immunohistochemical and histological examination. Such a study helps confirm the diagnosis.
But the most important thing in the diagnostic process is still the determination of ANCA in blood serum by the method of indirect immunofluorescence or by enzyme immunoassay.
The set of studies that the doctor prescribes depends on the clinical picture and the patient’s complaints.
Doctors often encounter difficulties at the stage of early diagnosis, since the symptoms of the disease are often not clearly expressed and are also similar to the signs of other diseases. Therefore, differential diagnosis often causes certain difficulties. For example, with hemorrhagic vasculitis, abdominal syndrome sometimes appears, which can be perceived as a gastrointestinal disease requiring surgical intervention.
To correctly establish a diagnosis, the following algorithm is practiced:
- Determination of clinical signs of vasculitis . When vascular damage occurs, skin syndrome, trophic disorder syndrome, and ischemic syndrome develop; mucosal involvement, arterial hypertension, venous involvement and organ changes are noted.
- Determination of laboratory and clinical signs of the disease . The presence of general symptoms and laboratory parameters is assessed.
- Distinguishing between the primary and secondary nature of the disease.
- Instrumental examination of blood vessels. To confirm vascular damage, dopplerography, angiography, biomicroscopy, angioscanning, capillaroscopy are performed and the presence of characteristic signs of damage is assessed.
- Identification of specific markers of damage to the vascular wall, laboratory diagnosis of vasculitis.
- Morphological study of material taken by biopsy. For this purpose, histochemical and immunomorphological methods are used.
- Determination of the main pathogenetic links of vascular damage. At this stage, the type of disease is determined (vasculitis associated with immune complexes; associated with ANCA; organ-specific antibodies; cell-mediated vasculitis with the formation of granulomas).
- Determination of the probable etiology of the disease. In most cases, the etiology of primary vasculitis is unknown, but exposure to certain viruses and bacteria cannot be ruled out. Immunogenetic markers are identified.
- Clarification of the form of vasculitis using classification criteria.
Diagnosis of vasculitis
The earlier the examination is carried out, the diagnosis is established and treatment is started, the greater the chances of avoiding damage to vital organs and disruption of their functions.
If necessary, consultations with a vascular surgeon, therapist, ophthalmologist, neurologist, otolaryngologist, etc. are scheduled.
The diagnosis is made based on a number of data:
- physical examination;
- laboratory tests.
Tests for vasculitis (see also rheumatological examination)
The following tests are required:
- general blood test (usually an increase in ESR is noticed);
- biochemical blood test (protein fractions, etc.);
- immunological tests (gamma globulin, C-reactive protein, rheumatoid factor, ANCA, etc.);
- blood for HBsAg if viral hepatitis is suspected.
In addition, instrumental methods such as:
- Doppler ultrasound;
- radiography;
- angiography (examination of blood vessels using X-ray contrast agents);
- CT scan.
1 General blood test
2 Doppler ultrasound
3 Plasmapheresis procedure
Treatment with folk remedies
If you visit any thematic forum, you can learn about many methods of treating vasculitis using traditional methods. But it is always important to remember that such treatment methods are only auxiliary in the process of main therapy. Before using them, it is better to consult a doctor about the advisability of such actions.
- If it is necessary to treat superficial vasculitis, herbal preparations are used that have a positive effect on the permeability of vascular walls and produce an anti-inflammatory effect. This effect is possessed by: Japanese sophora, buckwheat, water and bird knotweed, horsetail, and nettle.
- The use of decoctions and infusions of herbs that produce a general stimulating effect is also indicated: oat grains and straw, yarrow, rowan and black currant leaves, rose hips.
- The following will help reduce swelling in deep forms of vasculitis: string, stinging nettle, and cinquefoil erecta.
- In order to stimulate the function of the adrenal cortex, which is important in severe forms of vasculitis, treatment with drugs and decoctions containing ginseng, black elderberry, and eleutherococcus is recommended. Often patients are prescribed alcoholic infusions of ginseng and eleutherococcus.
- It is also recommended to drink green tea, which strengthens the walls of blood vessels and reduces their permeability, and also has a positive effect on metabolic processes in the body. It should be drunk every day, alternating with other herbal teas.
The following herbal remedies can be used:
- First collection. Knotweed, stinging nettle, sophora thick-fruited - 4 parts each, yarrow - 3 parts, black elderberry - 1 part. The infusion is prepared by pouring 5 g of the mixture with 1 cup of boiling water. Drink half a glass twice a day.
- Second collection. Black elderberry, horsetail - 3 parts each, peppermint - 2 parts. The infusion is prepared by pouring 5 g of the mixture with 1 cup of boiling water. Drink the infusion warm, half a glass 4 times a day. This infusion is also used for lotions. Applications are applied to the affected areas and kept for 15 minutes. This procedure can be carried out several times a day.
- The third gathering. is used as a general tonic and provides the body with vitamin K. To prepare it, St. John's wort, plantain, lungwort, black currant and rose hips are mixed in equal proportions. 10 g of product should be poured into 1 tbsp. water and boil for a few minutes. Drink half a glass 2 times a day.
Products for external use:
- Compresses made from pine resin. They are applied to the affected areas when applied to the skin. To prepare the product, 200 g of resin must be melted and added to it 40 g of unrefined vegetable oil, 50 g of beeswax. Mix everything, and when the mixture has cooled, apply it to the affected areas without removing it for 24 hours.
- Birch buds and nutria fat. To prepare the product you need to take 1 tbsp. grated dry or fresh birch buds and mix them with 500 g of nutria fat. Leave the product in a clay container for a week, keeping it on low heat in the oven for 3 hours every day. Place in jars and use every day as an ointment.
Vasculitis in children
Photos of hemorrhagic vasculitis in children
Children suffer from this disease quite rarely. But all types of vasculitis have characteristic features of their course in childhood.
Hemorrhagic vasculitis in children can occur against the background of infectious diseases - influenza , ARVI, scarlet fever , chickenpox. Other provoking factors may also influence this – hypothermia, injury, allergies, etc.
The disease leads to the fact that babies develop a lot of red hemorrhages on the mucous membranes in the mouth and lips. These hemorrhages rise slightly above the mucosa. Sometimes they bleed. A papular-hemorrhagic rash appears on the body. It forms on the limbs, legs, torso, and buttocks.
Other symptoms also appear, in particular articular syndrome. Joint pain appears simultaneously with skin manifestations or a little later. The pain disappears after a few days, but when a new rash appears, it reappears. Children also often experience abdominal syndrome , the main manifestation of which is severe abdominal pain. This can complicate the diagnosis, since the pain is similar to the symptoms of appendicitis , intestinal obstruction, etc.
Lung damage in the hemorrhagic form of the disease appears less frequently in children, but in this case there is a risk of rapid pulmonary hemorrhage. With various forms of the disease, children may experience blood in their urine.
Treatment of vasculitis must be carried out in a hospital setting. As a rule, heparin , vascular drugs, sorbents, and antiplatelet agents are prescribed. In some cases, treatment with prednisolone . When the disease progresses rapidly, plasmapheresis .
During the treatment process, adherence to a strict diet is very important. If the disease has subsided, the child is under medical supervision for 5 years. After all, there is a danger of relapse.
Diet
Hypoallergenic diet
- Efficacy: therapeutic effect after 21-40 days
- Timing: constantly
- Cost of products: 1300-1400 rubles. in Week
During illness, it is important to exclude from the diet all foods that can provoke allergic reactions. It is necessary to completely remove chocolate, cocoa, eggs, and citrus fruits from the diet. If you have kidney failure, you should not eat too salty foods or foods containing a lot of potassium. Alcohol should be completely avoided and food should not be too cold or too hot.
It is important to adhere to the following recommendations:
- Eat in small portions and at least 6 times a day.
- Introduce foods containing vitamins C, B, K and A into your diet.
- The amount of salt per day should not exceed 8 g.
- It is important to eat plenty of fermented milk products to restore calcium reserves in the body.
- The menu should include vegetable soups, boiled vegetables, cereals with milk and regular ones, vegetable oils, sweet fruits, boiled meat and fish, white bread crackers.
- You need to drink green tea, herbal infusions, jelly and compotes.
- As you recover, the diet is adjusted.
Consequences and complications
If the disease is not treated on time, the following complications may occur:
- liver and kidney failure;
- abdominal abscesses
- pulmonary hemorrhage;
- intussusception;
- polyneuropathy.
If, as the disease progresses, part of a blood vessel stretches and dilates, the risk of an aneurysm .
If during the inflammatory process the vessels narrow, the blood supply to individual organs and tissues may stop, which increases the likelihood of necrosis.
FAQ
What is the prognosis for vasculitis?
With timely consultation with a doctor, patient survival is 90%.
Is it possible to treat vasculitis at home?
If the patient’s condition and the identified stage of disease development allows this, then it is possible. Only the most difficult cases are hospitalized. Others can take medications on their own.
If you suspect vasculitis, who should you turn to for help?
First of all, you should make an appointment with a therapist, who, after collecting an anamnesis, will refer the patient to specialized specialists: a vascular surgeon, cardiologist, hematologist, etc.
List of sources
- Dunaeva N.V., Nikitina O.E., Stukov B.V., Karev V.E., Mazing A.V., Lerner M.Yu., Lapin S.V., Totolyan A. Cryoglobulinemic vasculitis associated with chronic hepatitis B: clinical observations and literature review.
- Nasonov E.L., Baranov A.A., Shilkina N.P. Hemorrhagic vasculitis (Henoch-Schönlein disease) // Vasculitis and vasculopathies. - Yaroslavl: Upper Volga, 1999. - 616 p.
- Handbook of a practicing physician. Under. ed. Vorobyova A.I. “Medicine”, 1981.
- Shostak N.A., Klimenko A.A. Systemic vasculitis: new in classification, diagnosis and treatment. Clinician. 2015;9(2):8-12
- Shilkina N.P., Dryazhenkova I.V. Systemic vasculitis and atherosclerosis. Ter. Arch. 2007; 3: 84-92.