The portal vein collects blood coming from the abdominal organs (intestines, spleen, stomach) and carries it to the liver. The organ ensures blood purification, after which it flows into the general circulatory system. The portal blood vessel is formed by the confluence of the splenic, inferior and superior mesenteric veins. The pancreatic and gastric veins (right and left) flow directly into the portal vascular trunk. The portal blood vessel of the liver ensures the normal functioning of the digestive tract and is an important unit of the circulatory system, the pathologies of which affect the functioning of the entire body.
Normal dimensions of the gallbladder:
- length up to 8-12cm[1,5,7];
— transverse size up to 3.5-5 cm [1,5,7];
— wall up to 3-4mm*[1,5,7].
*All measurements are given on an empty stomach, i.e. when the gallbladder is full. The wall of the gallbladder in a contracted state can be thicker!
When conducting a food test to determine the function of the gallbladder using ultrasound, it should shrink by 2/3 of its original volume by about 30 minutes after eating.
The pancreas normally has an even contour, a fine-grained structure and an echogenicity slightly lower than the hepatic (but may be higher than the hepatic, which, with normal sizes, can also be regarded as a variant of the norm - slight fatty involution, against the background of an “active” lifestyle, in particular abuse fatty foods, smoked meats, alcohol...), measured by transverse scanning, usually three dimensions are measured (anterior-posterior dimensions): head, body and tail; although some authors [5] also suggest measuring the isthmus of the pancreas (the border of the head and body), but in practice this is rarely used.
Treatment of pathology
Treatment of the disease involves an integrated approach and includes taking medications and surgery. Drug therapy includes the following medications:
- drugs from the group of anticoagulants - prevents the formation of blood clots and improves vascular patency;
- thrombolytics - dissolve existing blood clots, freeing the lumen of the portal vein.
Medicines are prescribed by the attending physician based on current symptoms
If there is no therapeutic result from the selected drug therapy, the person is prescribed surgical treatment. Transhepatic angioplasty or thrombolysis may be performed.
The main complication of surgical treatment is bleeding of the esophageal veins and the development of intestinal ischemia. Any pathology of the portal vein of the liver is a serious condition that requires the appointment of therapy adequate to the condition.
Normal stomach wall thickness:
- up to 3.5+-1.1mm[6].
Normally, on an empty stomach there should be no liquid contents in the stomach.
Kidneys normally have an oval shape in a longitudinal section, the echogenicity of the cortical layer of the parenchyma is lower or equal to that of the liver/spleen**[4], the echogenicity of the medullary layer of the parenchyma is lower than the cortical layer. The collecting-pelvis system, which is also sometimes called the renal sinus (which often causes antipathy among some urologists), is not normally dilated, which means the size of both the cups and pelvis is on average up to 5 mm; although depending on the type of pelvis and water load (therefore, the kidneys also look on an empty stomach, if the patient drank water before the ultrasound, the size of the collecting system may be larger), the size of the pelvis can normally reach 8-10 mm, with an increase in the pelvis of more than 1- 1.5 cm requires consultation with a urologist and urography (X-ray).
**Except for the neonatal period, in newborns the echogenicity of the renal cortex may be higher than the echogenicity of the liver/spleen!
[8]
The kidneys are usually measured in a longitudinal section, most often two sizes are measured, but sometimes three, and even the volume is calculated. It should be noted that the size of the kidneys may differ even in the same person when measured from different accesses (water load must also be taken into account), i.e. from the side and from the back. The error can reach 1 cm or more. By analogy with the liver indices, the ratio of length and transverse size of the kidney is also sometimes calculated[7], normally this ratio should be within 2:1 (i.e. oval shape). With nephritis of various etiologies, this ratio is smoothed out, i.e. the bud begins to tend to a round shape.
Portal hypertension
Portal hypertension often causes dilatation of the portal vein and visceral veins. However, if collateral blood flow is sufficient, there may not be significant expansion. In rare cases, dilatation of the portal vein system occurs without portal hypertension. Therefore, signs of collateral circulation and accompanying findings should always be checked in patients with dilated visceral veins and suspected portal hypertension. Collaterals between the visceral veins and the vena cava system can form at different levels. The first group of collaterals is formed by the junction areas between the protective and resorptive epithelium in the esophagus and anus. Periumbilical collaterals drain blood from the portal vein directly into the saphenous veins of the umbilicus.
In the abdominal cavity and retroperitoneal space, various paths of collateral outflow of blood can form with the participation of gonadal veins, collaterals between the mesentery and the lumbar veins or veins of the abdominal wall, diaphragmatic veins and even veins in postoperative scar tissue. Finally, there is the possibility of the formation of natural shunts between the splenic or gastric veins and the left renal vein. Such shunts may be large enough to reduce portal pressure to near normal levels despite a marked reduction in portal blood flow toward the liver. However, large portocaval shunts can lead to encephalopathy or septicemia by intestinal microflora.
• CT morphology
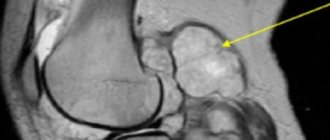
Direct morphological symptoms of portal hypotension are dilatation of the portal vein (> 13 mm), splenic vein (> 10 mm) or superior mesenteric vein (Fig. 1 a). On native sections, varicose veins can be confused with non-enhanced intestinal loops, enlarged adrenal glands and other space-occupying lesions. Varicose veins may have a diameter larger than the aorta. They can be recognized after intravenous contrast, but scanning too early leads to incomplete filling of the venous system with contrast agent.
Esophageal varices are the most common complication of portal hypertension. These veins form anastomoses between the visceral venous system and the azygos vein system through the fundus of the stomach and the esophageal mucosa. The anterior branch of the left gastric vein drains into the veins located in the wall of the esophagus, which leads to thickening of the latter with a noticeable accumulation of contrast agent in the central part of the wall near the lumen of the esophagus. The posterior branch drains into the azygos vein through the paraesophageal veins, which form multiple contrasting tubular structures in the periesophageal tissue. They communicate with the veins of the esophagus through perforating veins, which are rarely visible on CT. Paraesophageal varices may not respond to sclerotherapy and lead to early relapses of esophageal varices. Large paraesophageal nodes sometimes cause a picture of pathological formation in the mediastinum and form varicose aneurysms. Collaterals between the veins of the cardia and the diaphragm may be relatively small (average value <3 mm).
By tracing the veins of the esophagus down into the abdominal cavity, gastric collaterals, usually the coronary veins and short gastric veins, can be demonstrated. Anorectal varices form anastomoses between the inferior mesenteric vein and rectal veins from the internal iliac vein system. While rectal varices often cannot be assessed on CT, pararectal varices are easily detected. As a result of anorectal bypass surgery, the inferior mesenteric vein or internal iliac veins may be enlarged. Collaterals between the inferior mesenteric vein and the internal iliac veins can also form varices in the colon, but they are much less common than rectal varices. Collaterals along the old tracts of the obliterated umbilical vein cause enlargement of one or more periumbilical veins. These veins leave the liver as a direct continuation of the proximal part of the left branch of the portal vein and form anastomoses with the superficial superior and inferior epigastric veins (Fig. 2 b). The collaterals extend into the chest wall and down to the groin areas, forming a jellyfish head pattern.
Periumbilical varices are seen in patients with intrahepatic or posthepatic portal flow obstruction (liver cirrhosis, chronic Budd-Chiari syndrome). Large subcutaneous varices are very common and can complicate laparotomy. Collaterals between the visceral veins and the veins of the retroperitoneum or abdominal wall include anastomoses between the liver capsule and the diaphragm, as well as those located in the splenorenal ligament or between the greater omentum and the veins of the abdominal wall, lumbar veins and veins in postoperative scars. Paracaval anastomoses are also observed. Collaterals with the pulmonary veins have been described. In women, a bypass outflow tract may develop between the mesenteric and ovarian veins. Collaterals around the common bile duct can be life-threatening during endoscopic cholecystectomy.
Local occlusion of the visceral veins is caused by a tumor or thrombosis and leads to segmental portal hypertension with local collaterals (Fig. 1 c). Spontaneous splenorenal shunt is a relatively common finding in long-standing portal hypertension. It arises between the portal venous system and the left renal vein or directly from the splenic vein or through the phrenic, pancreatic, gastric and left adrenal veins. A typical CT finding is a dilated left renal vein. Some patients have short anastomoses between the splenic and left renal veins (Fig. 1a), while in others the collaterals in the left upper quadrant of the abdomen may be so tortuous that they are difficult to follow in transverse sections. In such cases, displaying the image in cinema mode or using MIP and VRT will help.
Image number 1
Portal hypertension. (a) Dilated mesenteric vein and spontaneous splenorenal shunt (arrowheads), indicated by a markedly dilated left renal vein. Note the occlusion of the portal vein (arrow) by hepatocellular carcinoma. (6) MIP of periumbilical colla terae with thin slab (4×1/6). (c) Volumetric representation of collaterals through the gastroepiploic vein in a patient with splenic vein occlusion by pancreatic cancer (3/5/2).
Image number 2
Case Discussion: Patient 25 years old with nausea, vomiting, abdominal pain CT scan of abdomen 25 year old patient with cystic fibrosis (CF), distal ileus syndrome. Advanced cirrhosis of the liver (nodules in the liver structure) and extensive dilatation of collaterals of the portal system, as a complication of portal hypertension. Splenomegaly. Also pay attention to complete fatty atrophy of the pancreas - as a feature of the manifestation of cystic fibrosis. The small intestine is dilated and filled with intestinal fluid up to the distal ileum.
Material taken
1) Matthias Prokop Michael Galansky Spiral and multi-slice computed tomography 2) radiopaedia. Org
Normal kidney sizes:
- length 9-12 cm [1,5,7] (length less than 9 cm can be considered as hypoplasia), sometimes in tall people the kidneys can be longer than normal, also when lengthening the kidney, it is necessary to exclude doubling of the kidney, which is often asymptomatic (t i.e. often not dangerous to health) and is detected by chance (i.e. for another reason) on urography;
— transverse size 4-6cm[1,5,7];
— parenchyma thickness 1.3-25 mm[1].
The adrenal glands are normally visible only in infants, usually up to 1-2 months of life. On ultrasound they appear as hypoechoic curved linear structures.
https://www.uzgraph.ru/forum/ugadayka/7/479/nadpoc...
Sometimes you can find a description of the size of the adrenal glands in some literature sources[6] and in reports on adults; most often this is simply a measurement of a piece of fatty tissue in the area of the upper pole of the kidney, because according to classical ideas about anatomy, this is where the adrenal gland should be located (as the name suggests). In fact, in adults, the adrenal glands are not visible on ultrasound (i.e., they are indistinguishable on ultrasound from the fatty tissue around the kidney), and they can be located not only in the area of the upper pole of the kidney. And the main task of ultrasound is to search for formations of the adrenal gland, which are often visible on ultrasound!
Normally, the ureters are also not visible on ultrasound; they become visible when they expand due to diseases. The exception is when the bladder is full. In such cases, the patient should be asked to go to the toilet and look again.
The bladder normally has an oval shape and an anechoic lumen, the thickness of the wall when filled is up to 4 mm [1,7], if the bladder is empty or poorly filled, the wall may be thicker.
Diagnostic measures
The main diagnostic technique for detecting changes in the portal vein remains ultrasound. The study can be prescribed to pregnant women, children and elderly patients. Doppler ultrasound, used in conjunction with ultrasound, helps assess the speed and direction of blood flow. Normally, it should be directed towards the organ.
With the development of thrombosis, a hyperechoic (dense) heterogeneous formation is detected in the lumen of the vessel. It can fill the entire lumen of the vessel, or cover it only partially. In the first case, blood movement stops completely.
One of the most common liver vascular pathologies
With the development of portal hypertension syndrome, dilation of the vascular lumen is detected. In addition, the doctor detects an enlarged liver and fluid accumulation. Doppler ultrasound will show a decrease in blood flow velocity.
A possible sign of portal hypertension is a cavernoma. The patient is required to undergo an FGDS to assess the condition of the esophageal anastomoses. Additionally, esophagoscopy and radiology of the esophagus and stomach may be recommended.
In addition to ultrasound examination, computed tomography with a contrast agent can be used. The advantage of using CT is the visualization of the liver parenchyma, lymph nodes and other formations located in close proximity.
Angiography is the most accurate method for diagnosing portal vein thrombosis. Instrumental studies are complemented by blood testing. Of clinical interest are indicators of leukocytes, liver enzymes, and bilirubin.