What is the cause of hypercholesterolemia?
The most common cause of increased cholesterol levels is excess nutrition and a sedentary lifestyle. Modern man spends too few calories with a “full” diet. Hereditary predisposition plays a certain role.
In addition, hypercholesterolemia can be secondary and provoked by diseases such as:
- diabetes;
- decreased thyroid function (hypothyroidism);
- kidney damage in the form of nephrotic syndrome;
- liver dysfunction;
- genetic diseases (familial hypercholesterolemia).
Hypercholesterolemia can also occur while taking certain groups of pharmacological drugs.
These include:
- progestins;
- anabolic steroid;
- different types of immunosuppressants.
Risk factors for the development of hypercholesterolemia are:
- hereditary predisposition;
- excess body weight;
- low physical activity;
- chronic or acute stress.
Hypercholesterolemia - symptoms and treatment
The main goal in treating hypercholesterolemia is to prevent serious complications or at least reduce their risk.[8] This is achieved through the intermediate goal of correcting cholesterol levels in the blood, as well as by influencing other known risk factors for atherosclerosis.
When the cholesterol level in the blood is normalized and its concentration is maintained in the optimal range for a long time, the risk of myocardial infarction, stroke, and death from cardiovascular causes gradually decreases. Therefore, it is so important to maintain an optimal concentration of cholesterol in the blood (primarily “bad”) for as long as possible, ideally for life.
Of course, in many cases, changing lifestyle alone is not enough for this, especially since few people manage to maintain a healthy lifestyle for a long time - there are too many temptations along the way.
If there is a high risk of cardiovascular complications, medications that reduce the level of “bad” cholesterol must be prescribed, regardless of the patient’s intention to improve their lifestyle.
Currently, cardiology has abandoned the concept of “normal cholesterol levels”. Instead, the term “optimal cholesterol level” is used, and what it will be depends on the total cardiovascular risk. Based on the data obtained about the patient, the doctor calculates this risk:
- If the risk is very high (and this is, for example, all patients who already have coronary heart disease or have suffered an ischemic stroke, suffer from diabetes mellitus and a number of other categories), then the optimal level for “bad” cholesterol will be less than 1.8 mmol /l.
- At high risk (if the patient does not yet have atherosclerotic cardiovascular diseases, but he has several risk factors, for example, a smoking hypertensive man of 50 years with a cholesterol level of 6 mmol/l will have a high cardiovascular risk) the optimal value for " bad cholesterol will be less than 2.6 mmol/l.
- For everyone else who is not at high or very high cardiovascular risk, the optimal low-density lipoprotein cholesterol ("bad" cholesterol) value is less than 3.0 mmol/L.
If there is a genetic “damage” behind hypercholesterolemia, then lifestyle changes (diet, physical activity, smoking cessation) can only improve the biochemical composition of the blood to a limited extent, so additional drug therapy must almost always be resorted to.
What lifestyle changes can lower cholesterol and reduce the risk of heart disease?
First of all, this:
- reducing consumption of foods such as fatty meats, fatty dairy products, confectionery and sweets;
- complete cessation of smoking;
- reduction in body weight by at least 10% from the original, if there is overweight and obesity;
- increasing physical activity - fairly intense physical activity at least 4-5 times a week for 30-40 minutes, which requires effort (for example, running, cycling, outdoor sports games, swimming, etc.), including housework in this regard is not considered suitable physical activity.
All of these measures not only change the lipid composition of the blood for the better, but can also significantly reduce the risk of cardiovascular diseases associated with atherosclerosis (myocardial infarction, stroke, angina pectoris and others).
Drug therapy
The main drugs used to reduce cholesterol levels and its associated cardiovascular risks are statins. The first statins were obtained, like the first antibiotics, from mold cultures. The next generations of statins appeared thanks to chemical synthesis.
Statins are perhaps the most well-studied drugs in the history of medicine and also some of the safest.[9] This group of drugs inhibits the synthesis of cholesterol in the liver (yes, most of the cholesterol is formed inside us and does not come from outside). The liver, needing cholesterol primarily for the synthesis of bile acids, begins to more actively extract cholesterol from the blood as part of low-density lipoproteins, as a result of which gradually, over the course of a month or two, the concentration of cholesterol in the blood decreases and can decrease by 50% from the previous level with a sufficient dose of statin. The results of numerous clinical studies involving many thousands of patients provide convincing evidence of the ability of this group of drugs not only to reduce blood cholesterol levels, but also, more importantly, to seriously reduce the risk of myocardial infarction and stroke, and most importantly, to increase the life expectancy of patients with cardiovascular diseases (primarily those who have had myocardial infarction, as well as people with other forms of coronary heart disease).
Using intravascular ultrasound, the ability of statins, when taken regularly for at least two years, has been proven to stop the development of atherosclerosis and even reduce the size of atherosclerotic plaques.
It is important that, if there are indications for their use, treatment with statins is carried out in sufficient doses and for a long time - for a number of years. The usual doses in modern cardiology are 40-80 mg of atorvastatin and 20-40 mg of rosuvastatin. These are the two most effective modern drugs of this class.
The “gold standard” are the original drugs of the development companies - Crestor (rosuvastatin from AstraZeneca) and Liprimar (atorvastatin from Pfizer). The remaining statin drugs containing rosuvastatin or atorvastatin are generic copies and must demonstrate their equivalence to the original drugs in clinical trials. Many generic drugs do not have such confirmation of their effectiveness and safety, and their use can sometimes be disappointing. The advantage of generics is their lower cost.
Another drug that lowers the level of “bad” cholesterol in the blood is ezetimibe. It blocks the absorption of cholesterol in the intestinal lumen and is usually prescribed in addition to statins if they do not allow one to achieve optimal cholesterol levels in monotherapy. Ezetimibe itself allows you to reduce the level of “bad” cholesterol by 15-20% of the original level, i.e. inferior in this regard to statins.
A new class of drugs that has surpassed statins in their ability to lower bad cholesterol is the so-called cumabs, which are antibodies to a regulatory protein responsible for regulating the rate at which cholesterol is absorbed from the blood.[11] True, these drugs are very expensive (treatment costs 30-40 thousand rubles per month). But there are situations when this is literally necessary to save a life, when otherwise the patient may not survive the next five years due to myocardial infarction or stroke. In addition, this new class of drugs is used to treat patients with familial hypercholesterolemia in cases where the maximum dose of statin therapy in combination with ezetimibe is still very far from achieving optimal cholesterol levels.
What can hypercholesterolemia lead to?
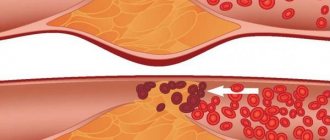
First of all, high cholesterol is the main factor in the development of atherosclerosis. Its deposits on the walls of blood vessels with the formation of atherosclerotic plaques pose a direct threat to all organs and systems of the patient.
Firstly, the lumen of the vessel itself narrows, which means that it begins to let in less and less blood, causing ischemia (oxygen starvation) of the organs that it supplies. The heart, kidneys and brain are primarily affected. The diameter of the vessels supplying these organs narrows due to the presence of atherosclerotic plaques, causing ischemia. With severe damage to the arteries of the legs, chronic insufficiency of blood supply develops, which can lead to the appearance of foci of necrosis and tissue ulceration.
Hypercholesterolemia leads to the formation of plaques in the wall of the largest vessel in our body - the aorta, leading to a loss of its elasticity and thickness. As a result, the wall is stretched under blood pressure and an aortic aneurysm occurs. And this, in turn, can lead to delamination or rupture, which is an extremely dangerous condition for the patient’s life.
Diagnostics
Laboratory hypercholesterolemia is detected by examining venous blood. In addition to the concentration of total cholesterol, the determination of its fractions and triglycerides is of great information. For differential diagnosis, the patient’s age and other anamnestic data are important - taking medications, the presence of close relatives with a confirmed familial form of hypercholesterolemia. To clarify the etiological factor, the following examination is carried out:
- Routine laboratory tests.
The content of liver transaminases (ALT, AST), markers of cholestasis (alkaline phosphatase, gamma-glutamyl transpeptidase), and glucose are measured. If nephrotic syndrome is suspected, a general urinalysis, analysis for microalbuminuria, and daily proteinuria are performed. - Hormonal studies.
The concentration of TSH and thyroid hormones (free T4 and T3) is determined. To confirm hypercortisolism, the level of cortisol in the blood is checked after performing small and large dexamethasone tests. - Immunological tests.
Tests are performed for markers of viral hepatitis (HBsAg, HCV), antimitochondrial (AMA), antineutrophil (ANCA) antibodies. - Ultrasound.
An ultrasound of the abdominal organs may reveal gall bladder stones, wall thickening, and signs of fatty infiltration in the liver. - Genetic research.
If hereditary hypercholesterolemia is suspected, mutations in the LDLR, PSCK-9, and ApoB-100 receptor genes are detected using the polymerase chain reaction.
For drug correction of hypercholesterolemia, different groups of drugs are prescribed
How to treat hypercholesterolemia?
The patient must be prescribed a diet low in fat and carbohydrates. As drug therapy, doctors at the CELT clinic use a wide range of lipid-lowering (lowering fat-lipid levels) agents. Their purpose, as well as the regimen of use, is selected individually and depends on the results of the examination of each individual patient.
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
Patient with homozygous familial hypercholesterolemia: difficult to treat. Case report
Andrey V. Susekov1, Tatyana V. Balakhonova2,3, Vladislav M. Soloviev4, Yuliia S. Isaeva4, Irina M. Miklashevich4, Irina V. Leontieva4 1Russian Medical Academy of Continuous Professional Education, Moscow, Russia;
2National Medical Research Center for Cardiology, Moscow, Russia; 3Sechenov First Moscow State Medical University (Sechenov University), Moscow, Russia; 4Pirogov Russian National Research Medical University, Moscow, Russia Abstract
Homozygous familial hypercholesterolemia is a severe genetic disorder characterized by extremely high levels of total cholesterol and low-density lipoprotein cholesterol (LDL-C), as well as by rapid atherosclerosis progression in various vascular territories.
Objective examination of the affected patients often reveals multiple Achilles tendon xanthomas, xanthomas on the extensor surface of arms, knee joints, etc. The prevalence of such severe inherited hyperlipidemia in many populations is about 1 : 1,000,000, however, the family heterozygous type frequency increase leads to the decrease of this value and to the increase in the affected people number. The paper introduces case report for the patient VI aged 16 who was diagnosed with homozygous familial hypercholesterolemia at the age of 12. DNA testing revealed pathogenic mutations in the LDL receptor gene which confirmed the diagnosis. The paper reports the results of the discussed patient treatment using triple-drug combination lipid-lowering therapy with rosuvastatin (40 mg/day), ezetimibe (10 mg/day) and evolocumab (420 mg/day) in the last two years. The total cholesterol level decreased from 20.8 mmol/L (baseline) to 7.3–12.00 mmol/L, and the LDL-C level decreased from 19.9 mmol/L to 4.6–9.9 mmol/L due to therapy, the treatment was well tolerated. During the observation period, a rapid regression of xanthomas on the buttocks, knee and elbow joints, and Achilles tendon was achieved. A series of baseline instrumental tests (2013) revealed severe atherosclerosis of carotid arteries (maximum stenosis up to 50%), and first symptoms of aortic valve stenosis. Another examination in the hospital (2019) revealed slowing the progression of atherosclerosis in the carotid arteries and aorta, however, the arterial hypertension onset required additional prescription of a low dose of enalapril. Exercise testing and Holter ECG monitoring has yet identified no myocardial ischemia. Thus, the timely diagnosis together with long-term triple-drug intensive lipid-lowering therapy make it possible to slow down the atherosclerosis progression in the discussed rare and severe category of patients. Key words
: homozygous hypercholesterolemia, familial hypercholesterolemia, low-density lipoprotein cholesterol, rosuvastatin, ezetimibe, evolocumab, combination therapy, slowing the atherosclerosis progression.
For citation
: Susekov AV, Balakhonova TV, Soloviev VM et al. Patient with homozygous familial hypercholesterolemia: difficult to treat. Clinical review for general practice. 2020; 1:35–41. DOI: 10.47407/kr2020.1.1.00006
Initial instrumented test data (2013)
Duplex scanning of the extracranial section of the brachiocephalic arteries from 01/25/2013 (Professor T.V. Balakhonova): multiple stenoses of the common external and internal carotid arteries (ICA) on the right and left with maximum stenosis up to 45–50% in the bifurcation of the right common carotid artery (CCA) and the proximal third of the right ICA up to 45%. Stenosis of 35% at the mouth of the right vertebral artery. According to the results of echocardiography (EchoCG) dated January 25, 2013 (the study was carried out by Professor M.A. Saidova): thickening of the aortic walls, aortic valve leaflets with the formation of initial signs of stenosis of the aortic mouth and regurgitation of the aortic valve of I–II degrees. The cavities of the heart are not expanded, the walls are not thickened. The contractile function of the left ventricle is satisfactory. The valve apparatus is intact. There are no signs of pulmonary hypertension. There is no data confirming congenital heart disease. Treadmill test (May 2013): no ischemic changes were registered against the background of the submaximal load performed. The test is negative. Exercise tolerance is average (7.7 METS).