What is the cause of hypercholesterolemia?
The most common cause of increased cholesterol levels is excess nutrition and a sedentary lifestyle. Modern man spends too few calories with a “full” diet. Hereditary predisposition plays a certain role.
In addition, hypercholesterolemia can be secondary and provoked by diseases such as:
- diabetes;
- decreased thyroid function (hypothyroidism);
- kidney damage in the form of nephrotic syndrome;
- liver dysfunction;
- genetic diseases (familial hypercholesterolemia).
Hypercholesterolemia can also occur while taking certain groups of pharmacological drugs.
These include:
- progestins;
- anabolic steroid;
- different types of immunosuppressants.
Risk factors for the development of hypercholesterolemia are:
- hereditary predisposition;
- excess body weight;
- low physical activity;
- chronic or acute stress.
Researchers have found a link between high cholesterol levels and increased infection of cells by the SARS-CoV-2 virus. This may provide an answer to why people with metabolic disorders such as diabetes and cardiovascular disease, who often have high cholesterol levels (hypercholesterolemia), are at higher risk of severe illness from COVID-19.
According to the STEPS study conducted in 2021, the prevalence of hypercholesterolemia in Belarus is 38.2% (>5mmol/l). The proportion of women (42.6%) with elevated total cholesterol levels is slightly higher than men (33.4%).
What is hypercholesterolemia and who is at risk
The bulk of cholesterol (about 80%) is produced by the body itself, the remaining approximately 20% comes from food. Hypercholesterolemia is a disorder of lipid metabolism in the human body, which is accompanied by an increase in cholesterol levels in the blood.
Viktor Snezhitsky, Doctor of Medical Sciences, Professor of the Grodno Regional Clinical Cardiology Center, Corresponding Member of the National Academy of Sciences. Viktor Snezhitsky:
The risk group includes people whose diet is rich in animal fats (red meat, sausages, sausages, pastries, baked goods) or have genetic characteristics/anomalies. In addition, some diseases (for example, diabetes mellitus, hypothyroidism, glomerulonephritis) are accompanied by an increase in the concentration of cholesterol in the blood. Taking a number of medications (glucocorticoids, hormonal contraceptives, beta-blockers) can also lead to hypercholesterolemia.
Smoking is a serious provoking factor. In addition, obese people, as well as patients with concomitant diseases (diabetes mellitus, liver and kidney diseases, arterial hypertension, decreased thyroid function), are susceptible to the development of hypercholesterolemia.
There are no pronounced symptoms of hypercholesterolemia, and this is its insidiousness. At the same time, elevated cholesterol levels increase the risk of developing cardiovascular accidents (strokes and heart attacks, atherosclerosis, chronic coronary heart disease, peripheral artery occlusion), sometimes at a young age. There are several clinical manifestations that may indicate high blood cholesterol levels:
- xanthomas (dense yellow formations) on the eyelids;
- xanthomas on the tendons (in the form of growths);
- the so-called lipoid arc of the cornea of the eyes - a rim of cholesterol (white or grayish-white).
The importance of a patient's lipid profile
The key to diagnosing disorders of lipid metabolism and cholesterol metabolism, as a special case of dyslipidemia, is a comprehensive assessment of changes in biochemical blood parameters that characterize lipid metabolism (lipidogram). Moreover, it is important to determine not only total cholesterol, but also a number of lipid fractions. Four indicators are most often assessed:
- total cholesterol;
- low-density lipoprotein cholesterol;
- high density lipoprotein cholesterol;
- triglycerides.
Victor Snezhitsky:
The term “total cholesterol” refers to its total concentration, while all cholesterol contained in the blood is distributed into different fractions - low- and high-density lipoproteins and some others.
Lipidogram. Norm
For an ordinary healthy person under the age of 40 without chronic diseases, the normal level of cholesterol in the blood should not exceed 5 mmol/l.
Biochemical blood test (normal):
- Total cholesterol – no more than 5 mmol/l.
- Low-density lipoprotein cholesterol (LDL) – 1.71-3.5 mmol/l
- High-density lipoprotein (HDL) cholesterol – less than 1 mmol/l
- Triglycerides – less than 1.8 mmol/l.
Is there a risk of a more severe course of Covid-19 in a patient with hypercholesterolemia?
- Dyslipidemia itself is a factor in the more severe course of coronavirus infection. In addition, there are a number of diseases (arterial hypertension, coronary heart disease, diabetes mellitus and others) in which dyslipidemia and, in particular, hypercholesterolemia, increases this risk even more, the expert notes.
- Risk factors for severe and complicated course of SARS-CoV-2 in adults include:
- Age over 60 years (risk increases with age);
- Concomitant diseases of the circulatory system (arterial hypertension, coronary heart disease, chronic heart failure);
- Cerebrovascular diseases;
- Concomitant chronic pathologies of the respiratory system (chronic obstructive pulmonary disease, bronchial asthma, fibrotic changes in the lungs);
- Endocrinopathies (diabetes mellitus, metabolic syndrome, obesity);
- Immunodeficiency conditions (oncological, hematological diseases, HIV infection);
- Other severe chronic diseases (chronic kidney disease);
- Smoking.
The course of Covid-19 infection may be complicated by vascular microthrombosis. This is the main problem. At the same time, it is currently difficult to say whether patients with coronavirus infection will develop hypercholesterolemia during the course of the disease or after it, the specialist believes. It is now known that a 12-year follow-up of patients who had suffered severe acute respiratory syndrome (SARS) caused by SARS-Cov showed that their risk of developing dyslipidemia was increased. There is no such information yet regarding people who have had SARS-Cov-2, due to the short observation period.
Should I take cholesterol-lowering medications?
A lot of publications have been made on this topic. Specifically, in critically ill patients treated in Lombardy, Italy, the incidence of hypercholesterolemia was 18%. In a series of other publications in patients with coronavirus, concomitant ischemic heart disease was recorded in 35.5%, and the mortality rate in this category was very high - 50%. Similar data were obtained in New York. 26% of hospitalized patients with COVID-19 had concomitant hyperlipidemia, and 10% had coronary artery disease. In those receiving outpatient treatment, hyperlipidemia was observed in 11% and 2%, respectively.
Victor Snezhitsky:
Early publications have shown that patients taking statins have a 35% lower risk of developing COVID-19. In addition, taking these medications is associated with a significant improvement in prognosis: patients with IHD and COVID-19 had a milder course of the disease, faster recovery, and lower mortality. One meta-analysis shows results indicating a 30% reduction in mortality in people with coronavirus infection when statins are used in the treatment of comorbid coronary artery disease.
In addition, the pleiotropic (multiple) effects of statins have been proven. Namely:
- anti-inflammatory and immunomodulatory effects;
- reducing the ability of SARS-CoV-2 to infect due to direct inhibition (suppression) of one of the viral proteases directly involved in this process;
- an increase in the expression of ACE2 with normalization of the renin-angiotensin-aldosterone system (regulates blood pressure) and a decrease in the degree of lung damage.
Victor Snezhitsky:
These effects indicate the advisability of continuing statins in patients with COVID-19 or prescribing them to those with appropriate indications. However, more recent publications, including large meta-analyses, indicate that taking statins during COVID-19 illness does not affect outcomes, including mortality. However, the recommendation to continue taking statins, if there are indications and no contraindications, remains in force.
In addition, according to studies regarding the experience with the use and effectiveness of drugs from the group of PCSK-9 inhibitors in the treatment of patients with COVID-19 and coronary artery disease, it is recommended to continue taking them as monotherapy or in combination with statins, depending on the initial conditions. The use of PCSK-9 inhibitors may further reduce LDL levels and the risk of cardiovascular disease.
At the same time, it is important to be careful when prescribing lipid-lowering therapy in patients with COVID-19, since the likelihood of drug-drug interactions is high, the professor emphasized.
Victor Snezhitsky:
In such patients, the risk of thrombosis and the likelihood of destabilization of existing atherosclerotic plaques increases. There is an increase in the incidence of heart attacks and strokes. Approaches to the diagnosis and treatment of dyslipidemia during the disease COVID-19 are formulated in the relevant protocols and recommendations (for example, Shlyakhto E.V., Arutyunov G.P., Belenkov Yu.N. .... V.A. Snezhitsky. - “The use of statins, anticoagulants, antiplatelet agents and antiarrhythmic drugs in patients with COVID-19." Cardiology. 2020; 60(6); E. V. Shlyakhto, et al. - "Guide to the diagnosis and treatment of circulatory system diseases in the context of the COVID-19 pandemic." — Russian Journal of Cardiology 2020; 25 (3).
A patient with hypercholesterolemia should be managed in accordance with protocols approved by the Ministry of Health of Belarus. Observe the patient over time, monitor laboratory parameters (primarily the level of troponin, D-dimers, C-reactive protein), record an ECG.
Currently, there is insufficient data regarding the long-term prognosis of the consequences of COVID-19 infection in patients who had dyslipidemia before the disease. But over time, of course, this will be possible. Without accurate, time-tested scientific data, any assumptions and statements are speculation.
This information is intended for medical and pharmaceutical professionals only. To be distributed at the venues of medical or pharmaceutical exhibitions, seminars, conferences and other similar events or directly transferred to medical and pharmaceutical workers. Dissemination of information by any other means that opens access to it to an indefinite number of persons is prohibited. The images used are not of actual patients. The article was created with the support of Novartis Pharma Services AG (Switzerland), representative office in the Republic of Belarus. BY/NEUR/11.2020/pdf/102662
What can hypercholesterolemia lead to?
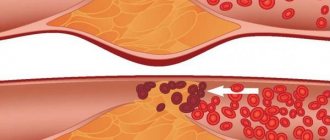
First of all, high cholesterol is the main factor in the development of atherosclerosis. Its deposits on the walls of blood vessels with the formation of atherosclerotic plaques pose a direct threat to all organs and systems of the patient.
Firstly, the lumen of the vessel itself narrows, which means that it begins to let in less and less blood, causing ischemia (oxygen starvation) of the organs that it supplies. The heart, kidneys and brain are primarily affected. The diameter of the vessels supplying these organs narrows due to the presence of atherosclerotic plaques, causing ischemia. With severe damage to the arteries of the legs, chronic insufficiency of blood supply develops, which can lead to the appearance of foci of necrosis and tissue ulceration.
Hypercholesterolemia leads to the formation of plaques in the wall of the largest vessel in our body - the aorta, leading to a loss of its elasticity and thickness. As a result, the wall is stretched under blood pressure and an aortic aneurysm occurs. And this, in turn, can lead to delamination or rupture, which is an extremely dangerous condition for the patient’s life.
Types of dyslipidemias
What is it and how to treat it? Dyslipidemia (hyperlipidemia) is an increase in lipid and lipoprotein levels relative to optimal values and/or a possible decrease in high-density lipoprotein or alpha-lipoprotein levels. In the dyslipidemia group, the focus is on hypercholesterolemia, since elevated levels of cholesterol (low-density lipoprotein) are directly associated with an increased risk of coronary artery disease.
In plasma, the two main lipid fractions are cholesterol and triglycerides. Cholesterol (CH) is an essential component of cell membranes; it forms the “framework” of steroid hormones (cortisol, aldosterone, estrogens and androgens) and bile acids. Cholesterol synthesized in the liver enters organs and tissues and is utilized by the liver itself. Most of the cholesterol in the composition of bile acids ends up in the small intestine, from the distal parts of which approximately 97% of the acids are absorbed and subsequently returned to the liver (the so-called enterohepatic circulation of cholesterol). Triglycerides (TG) play an important role in the process of transporting nutrient energy into cells. CS and TG are transported in plasma only as part of protein-lipid complexes - lipoproteins (the complexes include a simple protein - protein).
Currently, there are several classifications of dyslipidemia. One of them divides dyslipidemia into types according to the factors of occurrence: primary and secondary.
Primary dyslipidemias are disorders of lipid metabolism, most often associated with genetic abnormalities. These include: common (polygenic) and familial (monogenic) dyslipidemia, familial hypercholesterolemia, familial endogenous hypertriglyceridemia, familial chylomicronemia, familial combined dyslipidemia.
Lipoproteins differ in size, density, amount of cholesterol and TG and the composition of apoproteins (proteins localized on the surface of lipoproteins - ligand of lipoprotein receptors, enzyme cofactors):
- chylomicrons (CM) - saturated with TG and poor in cholesterol, are formed in the wall of the small intestine from alimentary fats;
- very low density lipoproteins (VLDL) - synthesized in the liver from endogenous sources and contain a lot of TG and little cholesterol. Increased VLDL levels are associated with an increased risk of atherogenesis;
- Low-density lipoproteins (LDL) are a cholesterol-containing class. They are synthesized in the liver, transferring cholesterol to its “consumers” - the adrenal glands, liver, etc. Today, LDL is considered the main atherogenic fraction of lipoproteins and the main “target” for lipid-lowering drugs;
- High-density lipoproteins (HDL) are an antiatherogenic class of lipoproteins that ensure the elimination of excess cholesterol from the walls of arteries and tissues. HDL has a positive effect on the condition of the endothelium and prevents the oxidation of LDL.
The classification of primary lipid disorders was developed back in 1965 by American researcher Donald Fredrickson.
It has been adopted by WHO as the international standard nomenclature for dyslipidemia/hyperlipidemia and remains the most common classification (see Table 1). Table 1. Classification of primary dyslipidemia according to Fredrickson
| TTip | Name | Etiology | Detectable violation | Occurrence in the general population, % |
| Type I | Primary hyperlipoproteinemia, hereditary hyperchylomicronemia | Reduced lipoprotein lipase (LPL) or disorder of the LPL activator - apoC2 | Increased HP level | 0,1 |
| Type IIa | Polygenic hypercholesterolemia, hereditary hypercholesterolemia | LDL receptor deficiency | Elevated LDL (TG is normal) | 0,2 |
| Type IIb | Combined hyperlipidemia | Decreased LDL receptor and increased apoB | Elevated LDL, VLDL and TG | 10 |
| Type III | Hereditary dys-beta lipoproteinemia | ApoE defect (apoE 2/2 homozygotes) | Increased DILI, increased CM levels | 0,02 |
| Type IV | Endogenous hyperlipidemia | Increased formation of VLDL and their delayed breakdown | Elevated VLDL | 1 |
| Type V | Hereditary hypertriglyceridemia | Increased formation of VLDL and decreased lipoprotein lipase | Elevated VLDL and CM | 1 |
Secondary dyslipidemias are lipid metabolism disorders that develop against the background of the following diseases:
- obesity (increased TG levels, decreased HDL cholesterol);
- sedentary lifestyle (decrease in HDL-C levels);
- diabetes mellitus (increased levels of TG, total cholesterol);
- alcohol consumption (increased levels of TG, HDL cholesterol);
- hypothyroidism (increased levels of total cholesterol);
- hyperthyroidism (decrease in the level of total cholesterol);
- nephrotic syndrome (increased levels of total cholesterol);
- chronic renal failure (increased levels of total cholesterol, TG, decreased HDL);
- liver cirrhosis (decrease in the level of total cholesterol);
- obstructive liver diseases (increased levels of total cholesterol);
- malignant neoplasms (decrease in the level of total cholesterol);
- Cushing's syndrome (increased levels of total cholesterol);
- Iatrogenic lesions while taking: oral contraceptives (increased levels of TG, total cholesterol), thiazide diuretics (increased levels of total cholesterol, TG), beta-blockers (increased levels of total cholesterol, decreased HDL), corticosteroids (increased levels of TG, increased total cholesterol ). For cholesterol levels, see Table 2.
Table 2. Cholesterol values for adults (men and women) of all ages
| Total cholesterol, mmol/l | LDL-C, mmol/l | |
| Normal level | below 5.2 (200 mg/dl) | below 3.0 (115 mg/dl) |
| Borderline (mild) hypercholesterolemia | 5.2–6.2 (200–250 mg/dL) | 3,4–4,0 (130–159) |
| Hypercholesterolemia | above 6.2 (250 mg/dl) | 4,1–4,8 (160–189) |
| Target level for patients with coronary artery disease with clinical manifestations of CVD and patients with diabetes mellitus | less than 4.5 (175 mg/dl) | less than 2.5 (100 mg/dl) |
How to treat hypercholesterolemia?
The patient must be prescribed a diet low in fat and carbohydrates. As drug therapy, doctors at the CELT clinic use a wide range of lipid-lowering (lowering fat-lipid levels) agents. Their purpose, as well as the regimen of use, is selected individually and depends on the results of the examination of each individual patient.
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions