Shortness of breath at the very beginning of pregnancy is very common. It manifests itself in the fact that a woman begins to have breathing problems during various activities. The frequency of inhalations and their depth change; it often seems as if there is not enough oxygen in the air. This condition often occurs not only during walks or walks, but also when performing banal routine actions around the house.
Where does this condition come from? Do you need to urgently go to the doctors? What to do and what to do?
Why does shortness of breath appear in the early stages?
Often shortness of breath is due to the fact that a pregnant woman's hemoglobin level in the blood drops. If there are such suspicions, then it is best to immediately get your blood tested and improve your diet. There is little pleasure in anemia during pregnancy, and it is a very, very popular pathology.
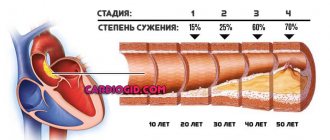
Also, one of the reasons for shortness of breath may be problems and problems with the heart. The body works for two people, and therefore respiratory activity is suppressed. Often, the expectant mother is bothered by a strong heartbeat during the early stages. You need to immediately consult a doctor and describe everything in detail to him. Particular attention should be paid to those girls who suffered from heart disease before pregnancy.
The doctor will perform a detailed diagnosis and establish the appropriate treatment, which will allow you to return your health to normal. Vitamins such as magnesium, iron, etc. are often added to the preparations.
Shortness of breath at the very beginning of pregnancy brings problems for the expectant mother. However, most often everything returns to normal on its own, without requiring any external intervention. For example, if a woman wears clothes that are too tight or too uncomfortable, then when she changes them to a looser wardrobe, the problem quickly disappears.
Other reasons that can cause shortness of breath:
- Wrong lifestyle and diet.
- Low pressure.
- Severe toxicosis.
- High physical activity.
- Interruptions with hormones.
- Increase in blood volume in the body.
- Overvoltage and stress.
- Lung diseases.
- Chronic diseases.
If shortness of breath during pregnancy does not disappear or subside, then it is better to undergo a detailed examination by doctors. Perhaps there are hidden foci of infection or other pathologies in the body.
Prevention and possible complications
Physiological attacks of lack of air are not harmful to mother and baby, but they are very unpleasant. You should not be afraid of their complications. If it is difficult to breathe during pregnancy due to endocrine, cardiac, or pulmonary diseases of the woman, it is important to take action. This can be dangerous for the health of the mother, threatening fetal hypoxia and premature birth.
Breathing disorders in pregnant women, the cause of which is not pathological changes in the body, are easy to prevent. To do this, it is important for the expectant mother to follow these recommendations:
- walk near bodies of water more often;
- in extreme heat, stay in a cool room;
- humidify the air in the house;
- monitor emotions;
- do fasting days;
- be sure to have breakfast;
- control weight, hemoglobin;
- leave places where people smoke (we recommend reading: if a nursing mother smokes, is it harmful for the baby?);
- take oxygen cocktails;
- go to the doctor in a timely manner in case of ARVI, tachycardia and other ailments.
Breathing problems in pregnant women are a reason to listen to your body. Many changes during this period are natural. However, it is dangerous if shortness of breath becomes more severe every day and bothers you during sleep. In this case, you need to urgently see a specialist and find out the cause.
How to deal with shortness of breath
To eliminate all the problems and consequences of shortness of breath, you must adhere to the following simple rules. The first thing you need to do is reconsider your lifestyle.
Need to:
- Stop smoking.
- Avoid stress and overload.
- Choose a suitable wardrobe that will not hinder your movement.
- In summer, try to take a sun umbrella.
- Reduce your vital activity.
You can also try to relieve other symptoms, such as extreme fatigue. This will lift your spirits even in such a difficult stage as pregnancy.
What moms can do:
- You need to monitor your diet, improve it and balance it.
- You should try to drink more fluid.
- It's worth improving your sleep. If the weather outside is suitable, you can even sleep with the window open.
- Before going to bed, try to drink soothing teas.
- Try to stick to breathing exercises.
- Buy special pillows for sleeping.
- Do not sit for a long time in front of a computer or TV. You should constantly get up and stretch.
- You must not give in to panic and always control your condition even during an attack of shortness of breath.
Many expectant mothers speak positively about various essential oils. If shortness of breath takes you by surprise during physical activity, then you can sit down or lie down and take a break. The increase in loads should be gradual.
What to do and how to treat?
Physiological causes of the anomaly do not require drug support and do not affect the course of pregnancy. They will help to eliminate:
- slow walks near bodies of water;
- ventilation of rooms;
- reduction of loads;
- a diet of easily digestible foods;
- calm atmosphere in the house;
- avoiding overeating;
- breathing exercises (you can master exercises to prepare for childbirth);
- rest on the side.
The following method will help relieve an unexpected attack of shortness of breath. You need to sit comfortably on a chair (sofa, chair with a back) and relax your upper body. Place one of the palms on the stomach, the other on the chest area. Breathe according to the pattern - inhale for three counts, exhale for the fourth. Another method, if holding your breath takes you by surprise at home, is to get on all fours and relax as much as possible. You can lean on the fitball and hug it with your arms.
The tactics for getting rid of shortness of breath when identifying chronic pathologies are individual:
- in case of cardiovascular abnormalities, the doctor prescribes medications to normalize the functioning of the heart muscle;
- in case of inflammatory lung pathology, mucolytics and antibacterial drugs cannot be avoided;
- during neuroses, consultations with specialists are necessary to help restore high spirits and relieve stress;
- for obesity, a diet is indicated when light foods that are beneficial for the mother and fetus are prescribed.
What medications can be prescribed if there is not enough air during pregnancy? The list is given in the table:
| Type of drug | When shown | Famous medicines |
| Sedatives | Stress, nervous disorders, vegetative-vascular dystonia, insomnia | Glycine, Persen, Corvalol (see also: can pregnant women take Glycine sublingual tablets in the first trimester?) |
| Diuretics | Arterial hypertension, VSD | Furosemide |
| Nootropic | Dystonia (VSD) | Piracetam |
| Antihistamines | Allergies: skin itching, obstruction | Cetrin Fenistil |
| Vasodilators | Ischemia, angina | Apressin |
| Mucolytics | Inflammatory pathologies of the lungs | Lazolvan, Ambroxol |
| Antibiotics | Pneumonia | Amoxiclav |
What symptoms indicate that you need to see a doctor?
Shortness of breath is not always well tolerated by women. Often, such an ailment leads to the fact that a woman experiences severe discomfort, cannot lead her usual lifestyle, and feels severe pain. You should consult a doctor if you have the following symptoms:
- Pain while inhaling.
- Breathing too quickly.
- Blue lips.
- Cold hands or feet.
- Fainting.
- Increased weakness, unable to get out of bed.
- Increase in body temperature.
- Coughing up blood.
- Increased asthma.
Any breathing pathologies will certainly affect the baby. A lack of oxygen can lead to the child developing various developmental problems. There is no need to ignore such problems and diseases. It is worth taking decisive action immediately.
In the early stages of pregnancy, shortness of breath is not as dangerous for the baby as in later stages. It often goes away on its own. As soon as the hormonal levels settle down and hemoglobin returns to normal, shortness of breath will disappear. Try not to panic, walk outside more, lead a healthy lifestyle and actively relax. Try breathing exercises that will help you during childbirth.
When is shortness of breath dangerous for the health of the woman and the fetus?
Shortness of breath in pregnant women is often normal. However, if it occurs repeatedly, you should pay close attention to your health and consult a doctor. Urgent medical assistance will be required in a number of situations that can be dangerous:
- blue lips, painful pale skin;
- severe pain in the sternum when inhaling;
- pulse 110 beats per minute or higher;
- fainting state;
- panic attack;
- persistent cough, fever;
- allergic reaction in the form of bronchospasm.
The above symptoms are signs of the development of respiratory and heart failure, exacerbation of asthma, and pulmonary embolism. They are dangerous for the expectant mother and fetus and require hospitalization and professional support.
Recommendations for the second trimester of pregnancy
Most recommendations are universal for all trimesters, for example, giving up bad habits, sleeping for 8-9 hours and eating well. But there are some important tips that apply specifically to the second trimester.
- You should only sleep on your side and use a special pillow for pregnant women.
- From the 24th week, it is advisable to start wearing a bandage, this will help reduce the load on the spinal column.
- Avoid contact with people who are sick or have a cold. If the second trimester falls during the “cold season,” try to spend less time in crowded places.
- Take vitamin and mineral supplements, even if you haven't done so before. Right now, the need for vitamins and minerals is increasing somewhat, especially iron, as well as omega-3 PUFAs, which are needed for the formation and proper development of the child’s brain, nervous and immune systems.
- Switch to proper nutrition. The second trimester is a time of active fetal growth; diets and fasting are inappropriate now. But it is important not to get carried away with fast food, to make sure that the menu has enough proteins and seasonal vegetables and fruits.
Can pregnant women get vaccinated?
Vaccination for pregnant women is only partially approved in Russia. But there is growing evidence that vaccination is safe for mother and child.
Several thousand women around the world are now known to have been vaccinated during pregnancy. The registry of the American Center for Disease Control contains observational data on 827 patients. The frequency of pregnancy complications in them did not differ from the frequency of complications in unvaccinated people. Therefore, some major foreign national associations have recommended vaccination for pregnant women who are at high risk of developing severe COVID-19.
The updated instructions for the Russian Sputnik V vaccine recently included a new instruction: it should be used during pregnancy “only in cases where the expected benefit to the mother outweighs the potential risk to the fetus.” Evidence that the vaccine is safe during pregnancy comes only from animal studies.
Vaccination is not recommended for nursing mothers due to the fact that “the risk to newborns/infants who are breastfed cannot be excluded,” the instructions say.
PHYSICAL ACTIVITY DURING PREGNANCY
Severe pain during pregnancy in the second trimester is a reason to refuse physical activity and a reason to urgently consult a doctor.
But if a pregnant woman feels great, moderate physical activity in the form of walking, swimming, yoga or gymnastics will only be beneficial for pregnant women.
Women endure the second trimester of pregnancy much easier than the first. Monitor your condition, visit your doctor regularly, get more positive emotions, and pregnancy will bring you extremely joyful moments.
Share on social media networks
Differences from colds
There are certain signs that even allow you to independently understand whether a runny nose has a cold or an allergic cause. The main distinguishing feature is that snot in case of an allergic disorder is liquid, transparent, more like water. If the disease is a cold, then the discharge becomes thick, green or yellow-green. They may also have a strong, unpleasant odor. In addition, with a cold, the temperature rises, but with allergies, there is no rise.
Signs of the first and second pregnancy
Are the early signs of the first and second pregnancy different? We answer: everything is purely individual. There are many cases where the same woman’s first pregnancy occurred against the background of severe toxicosis, while bearing a second child did not cause any problems.
In general, gynecologists identify the same early signs of pregnancy, regardless of whether it is the first, second or third. However, pathologies such as hemorrhoids and varicose veins during the second and subsequent pregnancies become aggravated already in the first weeks of gestation.
Prices for osteopathic services
| SERVICE | ADULTS | FOR CHILDREN |
| Osteopath consultation | 2 500 | 2 500 |
| Osteopathic treatment session | 7 500 5 000 (4,500 with prepayment for a course of 7 procedures) | 7 500 5 000 (4,500 with prepayment for a course of 5 procedures) |
| Consultation with osteopath, head of the clinic, Lazareva N.G. | — | 3 000 |
| Osteopathic treatment session with the head of the clinic Lazareva N.G. | — | 7 000 (discount for prepayment of a course of 5 procedures) |
VISIT DOCTOR
How often to visit doctors.
It is recommended to visit your leading obstetrician-gynecologist once every two weeks. Frequent visits are needed to constantly monitor the dynamics of fetal development and the condition of the expectant mother. Other specialists should be visited as needed or as directed by your doctor.
Ultrasound screening at 18-24 weeks is especially important, as it helps to identify genetic diseases.
What tests to take.
The Ministry of Health recommends taking tests for the following studies: antibodies G, M, OAC, carbohydrate metabolism, OAM.
Changes in the 1st week of pregnancy
Pregnancy is definitely a magical time for every woman. The awareness that a little person is developing inside inspires and endows with new, sometimes completely unexpected qualities. Feeling concern for the well-being of the baby, taking care of him from the first moments of his life, giving your love even at the moment when the baby is still inside the mother’s body - these are natural impulses. But in the first seven days after conception, a woman is unlikely to feel these emotions.
Unusual, but almost imperceptible biological processes take place in her body. An egg fertilized by a sperm is just beginning its journey of transformation. It first moves down the fallopian tube to reach the uterine cavity. This takes time - three to four days. During the movement, it does not stop changing: the number of cells in it increases. And approximately on the seventh or eighth day after conception, the microscopic embryo is “embedded” in the wall of the uterus.
The uterus itself is preparing to receive the embryo. Its structure has not yet changed, so it is impossible to notice external signs of pregnancy in the 1st week, much less an enlarged abdomen. Changes occur only in the mucous membrane of the uterus - the endometrium. It increases in volume and becomes loose to allow the fertilized egg to sink deeply into it and attach to the wall of the uterus. From this moment and over the next nine months, the endometrium will not be rejected, which means that the next menstruation will not occur. The body moves to a new stage - pregnancy.
pixabay.com/
What kind of complications are we talking about?
In severe cases, problems can affect any aspect of pregnancy.
- Patients expecting a child are admitted to intensive care at least one and a half times more often than women of the same age who are not pregnant. And expectant mothers have to be connected to a ventilator even more often.
- Pregnant women are 50% more likely to experience premature birth and preeclampsia (high blood pressure and swelling).
- More than half of pregnant women with coronavirus give birth by caesarean section. Doctors often observe postpartum bleeding.
The highest risk of complications is observed in the following groups of women:
- with chronic lung diseases, including moderate and severe bronchial asthma;
- with diseases of the cardiovascular system and hypertension;
- with diabetes mellitus;
- with cancer;
- obese (body mass index > 30 kg/m2);
- with chronic kidney and liver diseases.