3.1. Risk levels of VTEC
The classification of a patient into a low, moderate or high risk group is carried out using a number of systems for assessing the patient's status and taking into account the nature of the upcoming treatment.
One of the most convenient tools for determining the risk of VTEC in surgery is the Caprini scale (Table 13). Table 13. Clinical characteristics scoring scale (according to Caprini)
| 3 points | 5 points | ||
| 41-60 years | 61-74 years | >74 years old | Stroke ( |
| Minor operation | Arthroscopic surgery | History of VTE | Major joint replacement |
| BMI >25 kg/m2 | Major open surgery (>50min) | Family history of VTE | Fracture of the femur, pelvis, tibia |
| Edema of the lower extremities | Laparoscopic surgery (>45 min) | Leiden mutation | Spinal cord injury ( |
| Phlebeurysm | Oncology | Mutation in the prothrombin gene | — |
| Pregnancy or postpartum period | Bed rest (>3 days) | Lupus anticoagulant | — |
| History of miscarriage (2-3 trimester) | Gypsum bandage | Antibodies to cardiolipin | — |
| Taking estrogens/gestagens | Catheter in the central vein | Increased plasma homocysteine levels | — |
| Sepsis ( | — | Heparin-induced thrombocytopenia | — |
| Severe lung disease, including pneumonia ( | — | Other thrombophilias | — |
| Respiratory dysfunction | — | — | — |
| Acute myocardial infarction | — | — | — |
| Congestive heart failure ( | — | — | — |
| History of inflammatory bowel disease | — | — | — |
| Therapy patient on bed rest | — | — | — |
Depending on the amount of points obtained during the collection of anamnesis and examination of the patient, he is assigned to one or another risk group.
It is advisable to distribute patients into groups according to the principle proposed in the recommendations of the American College of Chest Physicians as amended in 2012. Patients are divided into groups of very low risk, low, moderate and high risk depending on the number of points, as well as from the surgical option. The probability of developing VTEC in the absence of prophylaxis in these groups is respectively less than 0.5, 1.5, 3 and 6%. (Table 14). Table 14. Risk levels depending on the number of points or type of surgical intervention (according to Caprini as modified by ACCP)
| Risk | General surgery, including gastrointestinal tract, urology, vascular, thoracic, endocrine (thyroid) | Plastic and reconstructive surgery | Operation |
| Very low | 0 | 0-2 | Most "one day surgery" patients |
| Short | 1-2 | 3-4 | Surgeries on the spinal column (not oncology) |
| Moderate | 3-4 | 5-6 | Gynecological surgeries (non-oncology), cardiac surgery, thoracic surgery (most interventions), spinal column surgeries (oncology) |
| High | 5 and > | 7-8 | Bariatric surgery, gynecological surgery (oncology), pneumonectomy, craniotomy, traumatic brain injury, spinal cord surgery, severe trauma |
Due to the absence of fundamental differences in the frequency of VTEC and the tactics of management and prevention of patients with low and very low risks in clinical practice, it is advisable to combine them into one group with a low probability of VTEC.
Along with the Caprini scale, the risk assessment system using the volume, duration of surgical treatment and the patient’s age as the main factors is of great practical importance (Table 15).
Table 15. Risk levels of VTE
| Risk level | Patient characteristics |
| Moderate | Major operations* in patients 40-60 years old without additional risk factors |
| Major gynecological operations* in patients under 40 years of age during estrogen therapy | |
| Minor surgeries* in patients over 60 years of age | |
| Minor surgeries* in patients aged 40–60 years with risk factors | |
| Isolated shin bone fractures | |
| Rupture of ligaments and tendons of the leg | |
| Hospitalization with chronic heart failure III-IV functional class according to NYHA | |
| Acute infectious or inflammatory diseases requiring bed rest | |
| Acute lung diseases with respiratory failure that do not require artificial ventilation | |
| Burns up to 20% of the body surface | |
| Thermal inhalation injury, stage II | |
| High | Sepsis |
| Presence of verified thrombophilia | |
| Major operations* in patients over 60 years of age | |
| Major operations* in patients 40-60 years old who have additional risk factors for VTEC (history of VTEC, cancer, thrombophilia, etc.) | |
| Endoprosthetics of the hip and knee joints, operations for hip fractures | |
| Severe and combined trauma, spinal cord damage | |
| Burns over 20% of the body surface | |
| Thermal inhalation injury, stage III | |
| Complications of burn disease | |
| Chemotherapy, x-ray or radiotherapy in patients with cancer | |
| Ischemic stroke with paralysis | |
| Acute lung disease with respiratory failure requiring mechanical ventilation |
Note.
In all cases, the risk of VTEC increases with the presence of additional risk factors. * - see Appendix 2. Non-surgical patients. An approach to assessing the risk of VTEC in non-surgical patients is presented in Appendix 3.
Prevention of venous thrombosis and pulmonary embolism
Prevention of venous thrombosis and pulmonary embolism (PE) is based on determining the degree of risk of their occurrence for each individual patient and assigning it to one of three risk categories: low, moderate or high.
The category of risk of venous thrombosis is determined depending on the presence of risk factors for the development of venous thrombosis in each patient, which include: malignant neoplasms, heart failure, myocardial infarction, sepsis, dilated cardiomyopathy, atrial fibrillation, stroke, broncho-obstructive diseases, erythremia, inflammatory bowel diseases, obesity, nephrotic syndrome, surgery, trauma, age over 40 years, estrogen intake, prolonged immobility, pregnancy, varicose veins of the lower extremities, history of venous thrombosis, bed rest for more than 4 days, thrombophilia.
During surgical interventions, the degree of risk of venous thromboembolism is determined by an assessment of the severity of the surgical operation and the patient’s condition. The basis for the prevention of venous thrombosis in this category of patients is their early activation, elastic compression of the lower extremities and heparin therapy.
Elastic compression of the lower extremities affects blood stasis and the hemodynamic factor of thrombosis, being a method of nonspecific prevention and includes the following methods.
Elastic compression socks and stockings
unlike bandages, they create the compression necessary to normalize venous outflow and provide physiologically distributed pressure along the entire length of the limb.
To prevent deep vein thrombosis and thromboembolic complications, a special type of medical compression hosiery is used, called “anti-embolic” or “hospital” hosiery. In our practice, we use hospital knitwear from Tyco Healthcare/Kendall. In this case, the maximum pressure is created at the level of the ankles and measured in mm Hg, appropriate for each compression class, followed by a gradual decrease in the proximal direction, which eliminates the threat (as in the case of elastic bandages) of iatrogenic venous stagnation.
These products retain their compression properties for a long time, are processed, and are easy to put on and take off, which saves the time of medical personnel. The use of anti-embolic knitwear increases the effectiveness of specific anticoagulant prevention of pulmonary embolism by 3-4 times. “Lastoshir” compression garments have 3 compression classes and a wide range of modern colors (flesh, bronze, blue, gray, black, brown).
Contraindications for the use of compression hosiery include the following cases:
- Progressive atherosclerosis of the vessels of the lower extremities (degree of ischemia above grade IIA);
- Ankle circumference more than 35 cm;
- After surgery for autodermoplasty, plastic surgery with a rotational flap or on a free pedicle to close varicose ulcers;
- Severe leg deformity.
The size of compression hosiery is selected strictly individually, taking into account the morphometric data of the patient. When using compression socks, four parameters are measured - foot length, ankle circumference, maximum calf circumference, calf length (Fig. 1).
When choosing a stocking size, six measurements should be taken: foot length, ankle circumference, maximum calf circumference, maximum thigh circumference, thigh length.
It should be noted that this type of medical product practically does not cause a contact reaction of the skin, which is very important for most patients, since it does not contain latex.
A new generation of hospital knitwear - anti-embolic stockings T.E.D. — have a more reliable fit on the leg due to the presence of a flexible silicone elastomer along the edge of the product. The silicone coating is comfortable on the skin and holds the stockings in place perfectly. For a long time, anti-embolic products maintain constant graduated compression on the leg.
Rice. 1. Differential pressure distribution in TED compression garments (Tyco Healthcare / Kendall)
This allows you to increase blood flow by 138%. The mosaic circular knitting, directed to one side, correctly distributes pressure along the leg, and the absence of pressure in the popliteal vein allows blood to flow freely through this critical area. Ergonomics are also created by the interrupting bandage and the two-layer V-shaped insert in the fixing elastic band of the stocking, which prevents the effect of a tourniquet on the femoral vein. 3 types of T.E.D. compression hosiery are available: knee socks, stockings, stockings with a belt, and 27 possible sizes allow you to choose the knitwear for most patients. High-precision manufacturing techniques and strict quality control ensure correct pressure distribution and no defects.
The advantages of hospital knitwear over “classic leg bandaging” are obvious. Almost all clinics are aware that it is impossible to create dosed vertical (foot-shin-thigh) and horizontal (front surface of the leg - back surface of the leg, popliteal fossa) using elastic bandages. However, knowledge has not universally developed into beliefs, and especially into clinical practice, which was the reason for writing this section in sufficient detail.
Intermittent pneumatic compression
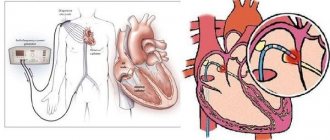
is carried out using a special compressor and cuffs divided into several chambers. Consecutive inflation of the chambers creates a “traveling wave” effect, which is especially useful in the absence of your own active muscle contractions. As a result, even in immobilized patients, the speed of venous blood flow increases significantly, i.e. one of the key factors of thrombogenesis is eliminated. Intermittent pneumocompression is most effective when using devices with microprocessor control and electronic timing (for example, the fifth generation pneumocompression device SCD, Fig. 2), which allows you to individually set the cuff filling time and maintain different levels of pressure on individual venous segments.
Rice. 2. SCD Response adjustable pneumatic compression device (Tyco Healthcare / Kendall)
With a digital display and special devices for fixing the device to the bed, intermittent pneumocompression becomes a relatively simple, safe and highly effective way to prevent venous thrombosis, which can be used during surgery, in the postoperative period, as well as in the intensive care unit for patients in hospital. critical condition. In cases where, due to a high risk of bleeding or for other reasons, the use of direct anticoagulants (surgeries on the brain and spinal cord, organs of vision and hearing, acute hemorrhagic stroke, etc.) is contraindicated, intermittent pneumatic compression in the modern version of its implementation is a method choice.
Specific prevention includes the perioperative use of pharmacological drugs of various groups.
Low molecular weight heparins (LMWHs) (ardeparin, dalteparin, nadroparin, parnaparin, reviparin, sandoparin, tinzaparin, certoparin, enoxaparin, etc.) are increasingly used for thromboprophylaxis in surgical patients, of which nadroparin calcium salt (fraxilarin) is currently the most widely used. , enoxaparin sodium salt (Clexane, Lovenox) and dalteparin sodium salt (Fragmin). Compared with UFH, these drugs have high bioavailability (more than 90%), a longer half-life (40 - 90 minutes for UFH and 1 90 - 270 minutes for LMWH) and antithrombotic effect (8 - 12 hours and 17 - 24 h), are less likely to bind to acute phase proteins, i.e. retain their effect against the background of endogenous intoxication, have a more predictable dose-dependent anticoagulant effect, do not stimulate, but weaken platelet aggregation, less often (less than 0.5%) cause thrombocytopenia and do not require laboratory monitoring.
These properties of LMWH are due to the chemical composition of the drugs. Heparin molecules, consisting of 25 - 50% of less than 18 saccharides (with a molecular weight of less than 5400 Da), are not able to bind ATIII and thrombin simultaneously, therefore they cannot accelerate the inactivation of the latter, but retain the ability to catalyze the process of factor Xa inhibition. As a result, the ratio of anti-Xa and anti-IIa activity in commercial LMWHs is not 1:1-2, as in UFH, α3-4:1; they have less anticoagulant activity than UFH, but have more pronounced antithrombotic properties. Since the composition of each of the commercial LMWHs is different, they differ, as we previously noted, from each other in physicochemical, biological and pharmacokinetic properties, are not interchangeable and have different clinical efficacy and safety.
Nadroparin calcium (Fraxiparin) is an official solution in pre-filled syringes with a volume of 0.3 - 0.6 -0.8 - 1.0 ml containing 2850 - 5700 - 7600 - 9500 MEanti-Xa activity, respectively. After a single subcutaneous administration of anti-Xa factor activity reaches a maximum after approximately 4 - 6 hours. Activity against Pa changes slightly and is maximum 3 hours after administration of the drug.
The main indications for use are: prevention of thromboembolic complications in general surgery, orthopedics, gynecology, as well as in other surgical and non-surgical patients who have a high risk of venous thrombosis due to acute respiratory or heart failure; patients being treated in the intensive care unit; patients with surgical infection. The drug is also used in the treatment of patients with acute coronary syndrome, the treatment of thromboembolic complications and for the prevention of blood clotting during hemodialysis.
The prophylactic use of nadroparin involves daily administration of the drug in a dose of 0.3 ml 1 time/day. before and after surgery in the form of a course lasting at least 7 days or until the patient’s motor activity is completely restored. During planned operations, the first dose is administered 2–4 hours before surgery; in emergency surgery, administration begins 1–2 hours after the end of surgery.
Enoxaparin sodium (Clexane)
- low molecular weight heparin, consisting of short mucopolysaccharide chains with an average molecular weight of 4500 daltons, produced in the form of an aqueous solution for injection containing 100 mg/ml in ready-made syringes of 0.2-0.4-0.6-0.8- 1.0 ml. 1 mg of enoxaparin corresponds to 100 MG of anti-Xa activity. The peak of anti-Xa factor activity reaches a maximum approximately 3 - 5 hours after subcutaneous administration and persists for 24 hours.
To prevent venous thrombosis and thromboembolism, surgical patients begin to administer enoxaparich before surgery: at a moderate risk, 20 mg (0.2 ml) 2 hours before surgery, at a high risk, 40 mg (0.4 ml) 1 2 hours before surgery and continue in the postoperative period for 7-10 days, one injection per day in the same doses. The use of higher doses of enoxaparin for the prevention of thrombosis in surgical patients is inappropriate, since increasing the dose is accompanied by a statistically significant increase in both anti-Xa activity and anti-lla, which significantly increases the incidence of hemorrhage. Therefore, higher doses of enoxaparin are used only in the treatment of deep vein thrombosis, as well as for the prevention of thrombosis during extracorporeal hemocorrection and hemodialysis operations. In the treatment of thromboembolic complications, the best safety/activity ratio of enoxaparin is achieved at a dose of 1 mg/kg, which is administered subcutaneously twice a day after 1-2 hours. For hemodialysis, enoxaparin is administered initially at a dose of 1 mg/kg for a 4-hour procedure. For patients with a high risk of bleeding, the dose is reduced to 0.5 - 0.75 mg/kg. If there are signs of fibrin deposition and a threat of thrombosis of the system, during a longer procedure, an additional 0.5 - 1 mg/kg can be administered.
At doses used for the prevention of venous thrombosis, enoxaparin has virtually no effect on bleeding time, blood clotting time, aPTT, and has no effect on platelet aggregation. In the first days of treatment with enoxaparin, moderate transient asymptomatic thrombocytopenia may appear. An asymptomatic and reversible increase in the number of platelets and an increase in the level of liver transaminases are possible. If the platelet count decreases by 30–50% of the initial value, treatment with enoxaparin should be discontinued.
Enoxaparin should be prescribed with caution to patients with a potential risk of bleeding, hypocoagulation, and patients with severe liver disease.
3.2. Methods for preventing VTE
Antiplatelet agents (acetylsalicylic acid). According to some data, acetylsalicylic acid helps prevent VTEC. However, evidence of its preventive effectiveness is limited and not as convincing as that of anticoagulants. In addition, there is reason to believe that acetylsalicylic acid has no safety advantage over anticoagulants. Therefore, although the use of acetylsalicylic acid for the prevention of VTEC can be discussed in individual patients, in most cases anticoagulants should be preferred.
Anticoagulants have well-proven preventive efficacy in various clinical situations; they reduce the risk of venous thrombosis and pulmonary thromboembolism by approximately half and should be used in all patients with an increased risk of venous thrombosis who do not have contraindications.
Subcutaneous prophylactic doses of UFH, LMWH, fondaparinux sodium, or VKA should be used. In addition, in traumatology and orthopedics, oral administration of NOACs (apixaban, dabigatran, etexilate or rivaroxaban) is possible. It is advisable to use mechanical methods of preventing DVT in patients of any risk level.
Mechanical methods are of particular importance when the use of anticoagulants is impossible due to the high risk of bleeding. In patients at high risk of DVT, it is reasonable to combine them with anticoagulants. Elastic stockings should be used to ensure optimal distribution of compression on the lower extremities (compression hosiery - see Appendix 3), or instrumental methods of prevention (alternating pneumatic compression of the lower extremities, and in some cases a venous pump for the foot, electromuscular stimulation, systems that provide flexion- extension movements in the ankle joints).
Early cessation of bed rest is one of the conditions for successful prevention of venous thrombosis and should be practiced in all cases where possible. However, in patients with an increased risk of venous thrombosis, this approach should not be the only method of prevention, since it does not provide sufficient protection.
Overdose of anticoagulants
In case of bleeding, doctors administer a 1% solution of protamine sulfate intravenously. Heparin is used as follows: to neutralize 100 units of heparin, 0.1 ml of a 1% solution of protamine sulfate is administered. The use of low molecular weight heparins for these purposes is relevant: 0.6 ml of a 1% solution of protamine sulfate neutralizes 0.1 ml of low molecular weight heparin.
Selected anticoagulants
Heparin
Heparin sodium is prescribed at a dose of 15,000 IU for 24 hours, and if the patient’s body weight is less than 50 kg, the daily dose of heparin is reduced to 10,000 IU. In elective surgery, the first injection is carried out 2 hours before surgery, the interval between injections is 8 hours
Low molecular weight heparins
There are two approaches to prescribing drugs: based on calculations and on the results of clinical studies. Dose calculation: from 4000 to 6000 units of anti-Xa per day. Injections are given 1 or 2 times a day. In emergency surgery, it is possible to start heparin prophylaxis after surgery, but no later than 12 hours after its completion.
Dalteparin (Fragmin) daily dose 5000 IU, for body weight above 120 kg daily dose 7500 IU. In clinical studies, a daily dose of 5000 IU has been studied.
Nadroparin calcium (Fraxiparin) daily dose 5750 IU (0.6 ml), for body weight above 120 kg daily dose 7550 IU (0.8 ml). Clinical studies have shown higher efficacy of the 0.3 dose (2875 units) than unfractionated heparin at a dose of 15,000 units per day; in one study, 0.6 ml of nadroparin calcium (5750 units) was used in patients weighing over 70 kg.
Enoxyparine (Clexane) daily dose 4000 IU (40 mg), for body weight above 120 kg daily dose 6000 IU (60 mg). Studies have generally shown the effectiveness of 30-40 mg of enoxaparin, and there are reports that a dose of 20 mg is not statistically different in effectiveness from 15,000 units of unfractionated heparin per day.
Factor Xa inhibitors
Rivaroxaban (Xarelto) is a direct factor Xa inhibitor (available in tablets), prescribed 10 mg once a day. Contraindicated in pregnancy and severe renal failure (creatinine clearance ≤15 ml/min).
Fondaparinux (Arixtra), a synthetic factor Xa inhibitor. The drug is administered no earlier than 6 hours after completion of the operation, 2.5 mg 1 time per day subcutaneously. In patients whose age is more than 75 years, and/or body weight is less than 50 kilograms, and/or who have moderately impaired renal function (creatinine clearance ≤ 3050 ml/min), it is better to refrain from administering the drug.