How common is extrasystole?
It is believed that extrasystole is observed in every person at some periods of life. With a single ECG recording in a group of healthy individuals, it is detected in 1.5-5% of cases. Daily monitoring reveals supraventricular extrasystoles in 14-91% and ventricular extrasystoles in 46-89% of healthy individuals. Although most of them are represented by single extrasystoles, complex forms can also be detected.
How often do doctors encounter extrasystoles?
Doctors deal with this diagnosis every day. Extrasystoles are diagnosed in 50-70% of all patients with rhythm disturbances, coronary heart disease and heart failure.
Causes of VES
PVC is always a secondary heart rhythm disorder, which means there is some underlying cause. The doctor needs to find her and influence her.
The reasons can be different: from stress and the presence of bad habits - smoking, alcohol, overeating, to pathologies of the cardiovascular system - ischemic heart disease, angina pectoris, hypertension, cardiomyopathy, heart defects, myocarditis. The reason may also be pathologies of other internal organs - lungs, gastrointestinal tract, cancer.
How dangerous is ventricular extrasystole?
Typically, doctors never tell a patient that something is threatening his life until they have carried out a comprehensive diagnosis and identified the root cause of the disease. There are safe extrasystoles that you shouldn’t even begin to treat, and there are those that require immediate action!
What is the diagnosis of VES?
The main thing is to understand whether the extrasystole threatens the patient’s life, whether it can lead to the most serious complication - sudden cardiac death!
First, the doctor records the patient’s complaints, then refers him to functional tests of the heart. First of all, on a 12-lead ECG, then on 24-hour Holter monitoring and ultrasound of the heart. To exclude coronary pathology - stress tests. Depending on the results obtained, we may prescribe a CT scan, MRI, gastroscopy, blood tests, intracardiac electrophysiological study or genetic testing.
Are all patients eligible for treatment?
Not every PVC requires correction. Sometimes, on the contrary, you should not touch it, as therapy can cause even greater harm to health.
The choice of treatment tactics depends on whether the patient has organic heart damage or whether it is structurally normal.
In treatment, it is necessary to achieve three goals: reducing symptoms, eliminating hemodynamic disturbances, and improving prognosis.
But the key goal is to prevent sudden cardiac death. It must be emphasized that the main thing is to determine whether the patient has a risk of sudden cardiac death due to extrasystole.
Treatment approaches and techniques
PVC is of a secondary nature, so at the beginning of treatment it is important to identify the primary disease and act on it.
Next, this is the prescription of medications, including antiarrhythmics, sedatives, potassium and magnesium preparations.
If drug therapy is ineffective, radiofrequency ablation or implantation of a cardioverter-defibrillator is prescribed if the arrhythmia is prognostically dangerous.
If there is no heart damage, patients are advised to change their lifestyle. Elimination of overeating, heavy food, alcohol, smoking. Sometimes extrasystole can go away even after rest or a vacation trip.
Ventricular extrasystole - symptoms and treatment
Once ventricular extrasystoles are detected in a patient, treatment should be selected taking into account the symptoms and the presence of dangerous types of extrasystoles.
The tactics for managing patients with ventricular extrasystole are as follows:
- observation without prescribing medications for patients with benign PVC, which is subjectively well tolerated (it is recommended to change lifestyle, eat a balanced diet, eliminate factors that provoke arrhythmia, adjust physical activity, etc.);
- in case of functional ventricular extrasystole (extrasystole caused by non-cardiac diseases) and extrasystole associated with heart pathologies, drug therapy is prescribed aimed at treating the underlying disease;
- treatment with antiarrhythmic drugs;
- the use of surgical treatment (radiofrequency ablation of the arrhythmogenic area of the myocardium, heart transplantation).
There are several main areas of treatment depending on the course, form and severity of PVCs.
1. If a person has no complaints, and the study reveals rare single monomorphic premature ventricular complexes that do not cause hemodynamic disturbances, no special therapy is required. In this case, the patient should give up caffeine-containing and alcoholic drinks, eliminate smoking, establish a daily routine, and ensure adequate sleep and rest. If there are any dysfunctions of the body associated with insufficient mobility, you need to increase physical activity in accordance with the body's capabilities. At the same time, it is necessary to exclude excessive physical activity (weight lifting, weightlifting). Your diet should include foods rich in potassium and magnesium: they have a beneficial effect on the cardiovascular system.
| Products containing potassium | Products containing magnesium |
| ⠀•⠀dried apricots; ⠀•⠀cocoa powder; ⠀•⠀wheat bran; ⠀•⠀raisins; ⠀•⠀sunflower seeds; ⠀•⠀nuts (pine nuts, almonds, peanuts, walnuts); ⠀•⠀legumes (peas, lentils, beans); ⠀•⠀jacket potatoes; ⠀•⠀avocado; ⠀•⠀ceps; ⠀•⠀bananas; ⠀•⠀citrus fruits; ⠀•⠀Brussels sprouts and kohlrabi; ⠀•⠀milk and fermented milk products; ⠀•⠀cereals (oatmeal, buckwheat, pearl barley, rice); ⠀•⠀fruits (peaches, pears, watermelon, apples, prunes, apricots, melon); ⠀•⠀chicory; ⠀•⠀vegetables (carrots, spinach, green onions, eggplant, cucumbers); ⠀•⠀chicken eggs; ⠀•⠀fish and meat; ⠀•⠀apple juice. | ⠀•⠀oil (sesame, flaxseed, peanut); ⠀•⠀cheese (Dutch, Poshekhonsky, goat, with mold); ⠀•⠀cottage cheese (low-fat and low-fat, curd cheese); ⠀•⠀bitter chocolate; ⠀•⠀almost all types of meat; ⠀•⠀fish (halibut, sturgeon, perch, haddock, cod, saury); ⠀•⠀duck eggs; ⠀•⠀cereals (rolled oats, chickpeas, peas, buckwheat, brown rice, lentils); ⠀•⠀fruits and berries (cherries, kiwi, pineapple, feijoa, raspberries, pears, peach, persimmon); ⠀•⠀many varieties of tea (for example, “Ivan-tea”) and juices; ⠀•⠀ginger; ⠀•⠀mustard; ⠀•⠀vanilla. |
2. When attacks of extrasystole are detected, which are accompanied by clinical symptoms, but do not disturb hemodynamics and have a benign course, beta-blockers (Bisoprolol, Metoprolol) are first prescribed. Sometimes, especially with functional ventricular arrhythmia against the background of vegetative-vascular dystonia and stressful conditions, drugs with sedative (Valemidin, Valerian) and anti-anxiety effects (Stresam, Adaptol), magnesium preparations (Magnerot) help in complex treatment , "Magne B6 forte"). It must be emphasized that the number of PVCs is taken into account when determining the degree of its malignancy. Frequent (up to 1000 or more per day) ventricular extrasystole in itself, even in the absence of obvious heart disease, is an indication for antiarrhythmic therapy.
Frequent PVCs and the appearance of paired, polytopic extrasystoles disrupt the movement of blood through the vessels, therefore, to reduce the risk of ventricular fibrillation and cardiac arrest, antiarrhythmic drugs are prescribed. It is preferable to use class I antiarrhythmics, and only if they are ineffective - Amiodarone or Sotalol. In parallel, drugs must be used to treat the underlying disease that caused the extrasystole[10]. To assess the results of treatment, as a rule, daily ECG monitoring is performed. A decrease in the number of PVCs by 75-80% indicates the effectiveness of therapy.
3. For PVCs of a malignant nature, it is necessary to prescribe highly effective drugs, such as Amiodarone and Sotalol. Sometimes they are combined with maintenance doses of beta-blockers. Treatment is usually carried out in a hospital setting, under ECG monitoring. In the hospital there are more opportunities to adjust hemodynamics and significantly reduce the risk of death in patients with cardiac arrhythmias.
Class I antiarrhythmics should not be taken if the patient has the following pathologies:
- severe signs of heart failure (low ejection fraction according to echocardiography);
- acute forms of coronary heart disease (acute infarction, progressive angina);
- previous myocardial infarction (especially if it was less than 6-12 months old);
- angina pectoris of functional classes III and IV (especially with proven coronary atherosclerosis);
- severe hypertrophy of the left ventricle with a thickness of more than 14 mm and/or the right ventricle (according to echocardiography);
- chronic heart failure class III-IV according to NYHA (New York Heart Association) and/or left ventricular ejection fraction less than 35%;
- pronounced dilatation (expansion of the chamber) of the left ventricle, cardiomegaly;
- active myocarditis;
- bundle branch block;
- severe bradycardia, etc.
If the patient does not have these contraindications and has moderately severe heart pathology, then the use of class I drugs can be considered [10]. It should be noted that antiarrhythmic drugs can have a proarrhythmic effect, i.e. cause a more dangerous arrhythmia, so only a doctor can prescribe them and only with appropriate indications.
Work has appeared that has shown the possibility of a beneficial effect of Omacor on ventricular arrhythmia, in particular in patients with coronary heart disease and chronic heart failure [6]. The addition of this drug to antiarrhythmics increases the effectiveness of treatment of ventricular arrhythmias. If the problem is associated with an electrolyte imbalance, then the patient is prescribed Magnesium sulfate or Potassium chloride.
The question of the duration of antiarrhythmic therapy is practically important. In patients with malignant ventricular arrhythmias, antiarrhythmic therapy should be continued indefinitely, in most cases for life. For less malignant rhythm disturbances, treatment should continue for up to several months with the possibility of gradual (due to the danger of rebound syndrome) its withdrawal. After stopping continuous therapy, the patient is advised to always carry a successfully used antiarrhythmic with him and take it in case of resumption of cardiac dysfunction.
4. For ventricular extrasystole, surgical treatment is possible. Indications for surgical intervention are:
- frequent (from several thousand to 20-30 thousand per day) ventricular extrasystole with an identified arrhythmogenic focus;
- ineffectiveness or impossibility of long-term use of antiarrhythmics in combination with poor tolerability or poor prognosis.
The high activity of the lesion makes it possible to detect it when drawing up a map of the electrical activity of the heart and perform radiofrequency ablation (RFA) of this myocardial zone[11]. The essence of the RFA technique is that a catheter is inserted into the patient through a large-caliber vessel, which is guided under the control of equipment to the very heart. First, using a special technique, the focus of pathological impulses is diagnosed, and then the site of ectopic excitation is exposed to a radiofrequency pulse, which leads to its destruction.
It is also possible to install an electrical pacemaker (ECS). The pacemaker is a device with electrodes that are attached to the ventricle and atrium during surgery. The electrodes create electronic impulses that cause the myocardium to contract. A pacemaker essentially replaces the sinus node, which is responsible for rhythm. It relieves a person from extrasystole and allows him to return to a full life.
In acute and chronic coronary heart disease, the development of ventricular arrhythmia is directly related to myocardial ischemia. In this regard, surgical myocardial revascularization (stenting, coronary artery bypass grafting) can improve electrical stability and reduce the likelihood of developing ventricular arrhythmias.
In patients with a high risk of sudden death and congestive heart failure, heart transplantation remains the main treatment option.
Archives
O. Y. Zharinov, V. O. Kuts National Medical Academy of Postgraduate Education. P. L. Shupika Ministry of Health of Ukraine
Extrasystole (ES) is the most widespread disturbance of the heart rhythm, which can significantly influence the life quality of patients, being a marker of structural and functional changes in the myocardium and indicate the unsafety of life unsafe You have heart arrhythmia. A more refined strategy for the management of ill patients is directly linked to the development of the concept of “stratification of risk”, so that patients are divided into groups according to the level of risk of death from all causes and, among other things, cancers. about cardiac death (CCD). In addition, day-to-day instrumental methods for diagnosing cardiac arrhythmias are being actively promoted, including ambulatory ECG monitoring. In clinical practice, there is an obvious need for the creation of favorable recommendations for the management of cervical diseases, specific diagnostic and therapeutic approaches.
ETIOLOGY
When SHE appears, they can call out any structural illness of the heart. They are especially common in patients with acute myocardial infarction (MI) and chronic ICH. However, extrasystoles can also occur with other myocardial stresses, including subclinical ones. In many patients with extrasystole, no available instrumental methods of investigation can be used to detect any signs of a weakened heart.
Wider causes and factors associated with SE:
- Ailments of the myocardium, endocardium and cerebrovascular arteries: ICH, myocarditis, myocardiofibrosis, cardiomyopathy, blood vessels, arterial hypertension or hypotension, heart failure (HF);
- Electrolyte imbalance (hypokalemia, hyperkalemia, hypomagnesemia, hypocalcemia), impaired acid-salinity;
- Hypoxia: sick leg, pulmonary hypoventilation (for example, during surgery);
- Traumatic injuries: chest injury, heart surgery, empty heart catheterization, brain and spinal cord injuries;
- Impaired autonomic regulation: neurocirculatory dystonia, neuroses, diencephalitis, sympathetic ganglionitis and truncitis, psychoemotional stress;
- Pathological reflexes, diseases of the organs and poisoning (virazkova disease, gum disease, pancreatitis, diaphragmatic clubina, colitis and enterocolitis, especially if they are accompanied by flatulence, constipation or electrolyte disturbances balance); dystrophic changes in the cervical and thoracic lobes of the ridge (osteochondrosis, spondyloarthrosis); bronchial diseases and illnesses, especially those accompanied by a persistent cough; prostate adenoma;
- Diagnostic procedures: endoscopy (bronchoscopy, gastroscopy, laparoscopy, cystoscopy, colposcopy, rectoscopy), puncture, carotid sinus massage, pressure on the apple of the eye, breathing while holding a deep breath;
- Allergies: food, medicinal, microbial, occupational, household;
- Pharmacodynamic and toxic effects of medications such as cardiac glycosides, quinidine, novocainamide, anesthetic agents, morphine, glucocorticoids, potassium, calcium preparations, tricyclic antidepressants, related phenotiases in other words, adrenomimetics.
The main electrophysiological mechanisms of extrasystole are re-entry (return input of awakening) and post-depolarization. The basis for extrasystoles may also be the mechanisms of asynchronous renewal of myocardial alertness and pathological automatism.
COLLABORATION OF THE SICK
Treatment of patients with cervical heart disease includes methods to ensure the diagnosis of cardiac rhythm disturbances, determination of the clinical and prognostic significance of arrhythmia, choice of treatment and assessment of its effectiveness.
Anamnesis.
When examining a patient, provide the following information: subjective manifestations of arrhythmias (heart palpitations, interruptions in the functioning of the heart, problems or a “frozen” heart, discomfort in the chest, due to insufficient wind, shortness of breath, confusion, syn digging camps), ancient history of destruction of the rhythm; factors that provoke arrhythmia (physical stress, psycho-emotional stress, late hour of prey, body position, food intake, alcohol, chicken); endured the remaining hours of illness; background cardiac pathology; advance use of antiarrhythmic drugs (AAP).
Clinically quilted.
Identification of arrhythmias during auscultation of the heart or during palpation of peripheral arteries; presence of clinical signs of HF.
Laboratory methods of investigation.
Valued instead of potassium, sodium, creatinine in blood serum, thyroid-stimulating hormone activity.
EKG.
Main ECG signs of extrasystoles (ES):
- It is preceded by the appearance of a widened and deformed intrabasic rhythm of the QRS complex without the P wave transmitted to it, after late extrasystoles, before which the P wave is registered, which does not impair the electrophysiological connection with the neck;
- Most often, a new compensatory pause is evident.
The shape of SH is not only due to the localization of the extrasystole, but also due to the fluidity and direction of the expansion of the impulse in the shanks. Therefore, the ECG makes it possible to determine the location of the ectopic cavity behind the morphology of the extrasystolic complex. It appears that there is a blockade of the right leg and the left anterior bundle of His, and it should be located in the system of the left posterior bundle of His, or in the posterior wall of the left bundle; It appears that there is a blockade of the right leg and the posterior inferior ganglion of the His bundle, which is located in the left anterior ganglion of the His bundle; If there appears to be a complete blockade of the left branch of the His bundle, then there is a blockage in the right branch of the His bundle. The QRS complex of the left ventral extrasystole in the right thoracic abductions has a mono- or biphasic form: R, qR, RR', RS, Rs and in the left ones - rS or QS. The QRS complex of the right ventricular extrasystole in the right thoracic adducts takes the form rS or QS, and in the left - R (Table 1). This is due to the dilation of the interstitial septum, as, of course, its length and shape slightly vary in relation to the QRS complex of the main rhythm. The QRS shape of the rSR' type in V1 is typical for extrasystoles from the left half of the interseptal septum, and the R or qR type in V6 is typical for extrasystoles from the right half of the septum. The directness of the QRS complex of the extrasystolic complex in all thoracic abductors allows localization of the cerebral muscle in the basal lobes of the heart, and the directness of the QRS complex in the lower abdomen allows for localization of the thoracic abductor in the basal lobes of the heart. In cases that are difficult for topical diagnostics, it is more precise that extrasystoles are not indicated, surrounded by a warning about the presence of E.
Table 1. Characteristic forms of NEC complexes in thoracic ECG leads with basal, perineal and superior localization
| Localization of extrasystoles | Forms of NHE complexes in ECG extensions | ||||||
| V1 | V2 | V3 | V4 | V5 | V6 | ||
| Right lunochkovi | Basal | Rs, Rs | R.S. | R | R | R | R |
| Crotch | rS, QS | rS | rS | rS, RS | R | R | |
| Livoshlunochkovi | Verkhivkov | rS, QS | rS, QS | rS | rS | rS, RS | Rs, Rs |
| Basal | R | R | R | R | Rs | RS, Rs | |
| Crotch | R, qR, RR', RS, Rs | R, Rs | R.S. | RS, RS | rS | rS, QS | |
| Verkhivkov | RS, Rs | rS, RS | rS | rS | rS | rS | |
| Basal | R | R | R | R | R | R | |
| Verkhivkov | rS | rS | rS | rS | rS | rS | |
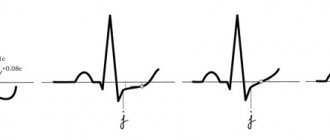
The intervals of aggregation of monotopic HE are, however, regardless of the fact that their form may be different (in this type the stench is polymorphic). The intervals for the accumulation of monotopic extrasystoles should not exceed 0.06–0.10 s. Floods may vary over the course of the consolidation interval and, as a rule, have different shapes of QRS complexes. Two extrasystoles are called guy (Fig. 1), and three to five are called group, “volley” (Fig. 2), or runs of ventral tachycardia - PC. You can also see early and even early SH („R to T”) (Fig. 3). Extrasystoles may be irregular (monotopic or polytopic), and their appearance with regularity is designated as an arrhythmia (bigeminia, trigeminia, quadrigeminia, etc.). Interpolations are registered between two normal QRS complexes, especially against the background of bradycardia.
Picture 1.
Alone and paired polytopic extrasystole.
Figure 2.
Group polytopic shlunochkova extrasystole.
Figure 3.
Early shlunochkova extrasystole “R to T”.
Scholochkovy extrasystole against the background of anterior fibrillation must be differentiated from aberant sluchkovy complexes. The shortening of the cardiocycle during atrial fibrillation, which ends with an aberrant scapular complex, is not accompanied by a compensatory pause, and is transferred to an extended RR interval. Aberrant QRS complexes, as a rule, take the form of blockade of the right leg of the His bundle of varying degrees of severity in the output V1 (rSR', rSr'), and left ventricular extrasystoles - the form R, RS, Rs, qR, RR' or Rr' (Table 2 ).
Table 2. Differential diagnosis of supraventricular extrasystoles with aberation of the internal sac conductivity and sac extrasystoles
| Signs | Supraventricular extrasystole with aberration | Shlunochkova extrasystole |
| QRS morphology in advanced V1: | ||
| rSR', rsR' | Characteristic | Not typical |
| qR, R, rR' with splitting on the output column | Very rarely | Not typical |
| qR, R, RS, Rsr', RR' with splitting on the downstream column | Not typical | Characteristic |
| rS, QS | Not typical | Characteristic |
| QRS morphology in advanced V6: | ||
| qRS | Characteristic | Not typical |
| rS, QS | Not typical | Characteristic |
| Importance of positive and negative teeth of the QRS complex in all chest muscles | Not typical | Characteristic |
OTHER METHODS OF INSTRUMENTAL DIAGNOSTICS
Holter monitoring (HM) of the ECG allows recording of the ECG without compromising the patient's roach mode for 24 years or more with the subsequent automated analysis of the recording. The number of extrasystoles per hour of exercise is assessed, their distribution of activity, connections with physical or emotional stress, heart rate, body intake, changes in body position, transitional episodes, etc. ii myocardium.
HM ECG is a “standard” method for diagnosing apparently infrequent extrasystoles, as well as assessing the severity of ECG detected during ECG registration. CM ECG allows more precise, shorter-term ECG recording to provide a clear and comprehensive assessment of the disturbance of heart rhythm due to a significantly larger number of assessed ectopic complexes. Alone, it is common to find ECG with CM in apparently healthy individuals.
The equalization of circadian changes in the number of extrasystoles and the frequency of heart rate (HR) allows for the increase in fluid intensity of such and bradyseal forms of extrasystoles. One of the broadest types of extrasystoles is the “vagal” (vagal, or “low”), when the frontal complexes are registered 1.5 times less often in the passive period of dob, against the background of sleep Synchronous with sinus rhythm. Vagozalezhnaya is more often diagnosed in young people without signs of heart pathology, it often has an episodic sign and is not considered sick. This form of extrasystole importantly does not require antiarrhythmic therapy. With the “adrenergic” (sympathostatic or “day” type), the average number of extrasystoles per year is 1.5 times greater during the active period of stimulation, and extrasystoles are often associated with accelerated sinus rhythm. The “adrenergic” type is more typical for summer people, especially those with IHD, hypertensive illness, heart disease, dilated and hypertrophic cardiomyopathies, myocardial fibrosis. In contrast to the “vagal” type, such extrasystole is not benign and often requires the use of AAP, beta-blockers and amiodarone. Even often, the daily connection between the number of extrasystoles and the period of increase and heart rate. You can also watch out for the “hectic” type of subdivision of extrasystoles with significant fluctuations from year to year. Such high ectopic activity over a short period of time may be associated with recurrent myocardial ischemia. The use of the HM ECG has significantly increased the possibility of detecting extrasystole and parasystole, establishing the variability of their forms and options.
The HM ECG method allows you to evaluate changes in heart rate variability per day. Zocrema, a decrease in the standard indicator of heart rate variability - standard variation of RR intervals by stretching (SDNN) - below 50 ms indicate an imbalance in the autonomic regulation of heart rate and one of the predictors of guilt RSS in patients with post-infarction cardiosclerosis, left systolic dysfunction (LS) and heart failure and save sinus rhythm. The strongest predictor of the risk of life-threatening arrhythmia was the result of low heart rate variability due to decreased heart rate fraction (EF) and impaired baroreflex sensitivity (follow-up). ATRAMI, 1998). It is clear that measurements are often used to assess hourly and spectral indicators of heart rate variability.
With CM ECG, attention is also paid to the variability and variability of the consolidation interval, as well as the variability of the QT interval. It is important to evaluate the additional fluctuations of the adjusted QT interval, and even with this significant increase, the severity of the “discharge” period of the cardiac cycle and the delay before the onset of paroxysms may increase „pirates-tachycardia”.
Repeated HM ECG against the background of treatment makes it possible to assess the effectiveness of the prescribed therapy. Based on the changes in the spontaneous fluctuations in the frequency of culprit arrhythmias of the heart, the following criteria for the effectiveness of antiarrhythmic therapy in patients with cerebral hypertension have been developed: a) a change in the number of cervical arrhythmias for an additional 50– 75%; b) a change in the number of young and early children by 90% or more; c) externally suspended episodes of ST; d) with polymorphic cerebral neck - a change in the number of morphological types of extrasystoles to 1–2. Assessing the adequacy of treatment with an antiarrhythmic drug, in addition to exceeding the criteria, also requires taking into account the specificity of its effect on sinus rhythm, conductivity, and the frequency of ischemic episodes.
Interpretation of HM ECG data to assess the effectiveness of antiarrhythmic therapy in case of high blood pressure. When the AAP is assigned to the 1st class under classification V. Williams, the effectiveness of the specified clinical criteria does not allow for an improvement in the prognosis of survival of patients with treatment. Moreover, the use of certain drugs (flecainide, encainide) in controlled studies was associated with significant increases in the prevalence of PCC. It is important that the treatment of patients with severe structural disorders of the myocardium (dysfunction of the myocardium after myocardial infarction or dilated cardiomyopathy, with/without heart failure) begins with the therapy of etiopathogenetic Direction: correct ischemia and hemodynamic disturbances. For evidence of LS dysfunction and partial symptomatic ES, amiodarone or sotalol should be added before basic preventive therapy (angiotensin-converting enzyme (ACE) inhibitors, β-blockers, aspirin, statins) - methods with proven effectiveness This is for the prevention of malignant sac arrhythmias. It is significant that beta-blockers and amiodarone can be used empirically, based on the established availability of these drugs, to predict the survival of patients and, regardless of changes in heart rhythm disturbances. In these situations, the HM ECG is completely dynamic to assess the interruption of heart rhythm disturbances against the background of antiarrhythmic therapy. And in situations where the stagnation of AAP is determined by the clinical manifestations of the rhythm disturbance, and not by their prognostic values, the initial criterion for the effectiveness of the drug is a change in symptoms causing arrhythmia. It is also agreed that the most effective way to prevent RSS in patients with high risk criteria is implantation of an internal cardioverter-defibrillator.
Trying out physical skills
(Master's test, step test, veloergometry, treadmill test) can provoke the appearance of WHILE under the hour of desire and in the early adolescence period due to increased activity of the sympathoadrenal system, an increase in catecholamines , development of tissue hypoxia, acidosis. In patients with chronic ICH, bicycle ergometry under one hour reveals HI in 60% of patients, and its frequency often correlates with displacements of the ST segment (Fig. 4). Under the infusion of physical exercise, the number and gradation of extrasystoles may change: an increase in the number of extrasystoles during the hour of exercise at high heart rate or in the first half after the end of the exercise Consider this possible connection with IHS; “Good” extrasystoles usually appear at the hour of exercise and renew 3–5 hours after its completion. It is necessary to call for diagnostic tests due to the following reasons: in some patients it is not possible to provoke an extrasystole that was previously diagnosed; in 11–40% of patients with a healthy heart, during physical exercise there is a single extrasystole, and in 5% - a pardy; In some patients, with physical stimulation, group and early extrasystoles may occur.
Figure 4.
Right-sided extrasystole against the background of horizontal depression of the ST segment.
Orthoclinostatic test
allows you to clarify the nature of extrasystolic arrhythmia: stable extrasystole occurs at rest during functional tests; Labile extrasystole of voltage appears or becomes stronger during an orthostatic test and a standard applied pressure of 50 W; Labile extrasystole calmly appears during an orthostatic test and physical exertion with a pressure of 50 W and appears after the transition to a horizontal position. It is important that labile extrasystole of stress and stable extrasystole are more likely to be associated with the presence of heart disease and/or a stable substrate of arrhythmia, and labile extrasystole of calm, as a rule, є functional (vagal).
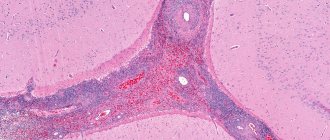
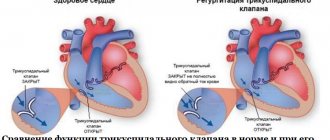
Echocardiography
It is necessary to clarify the infusion of both SE and AAP on the hemodynamic stage. The method allows you to estimate the size of the empty heart in systole and diastole, the vascular fraction, the thickness of the heart walls, the mass of the myocardium of the heart, the relationship between the end-diastolic volume and the mass of the myocardium of the heart, and zones of hypo- and akinesia, local hypertrophy, valvular valves, the phenomenon of “post-systolic “strengthening”, myocardial dysplasia of the right shank. A change in LVEF of less than 40% in patients with IHS is associated with an increased risk of RSS. Cardiac dysfunction can be more accurately determined using radioisotope ventriculography or coronary ventriculography.
Inner-Heart EED
It is a routine method for diagnosing disturbances in cardiac rhythm and conductivity, an important indication for cardiac pacing, radiofrequency catheter ablation and implantation of a cardioverter-defibrillator. The investigation is carried out in specially equipped laboratories. There are no absolute indications for performing intracardiac EPD in patients with SHE. This investigation may be even more useful if it is necessary to establish a connection between the heart rhythm and syncope and presyncope. If you are ill with asymptomatic excess of extrasystole, EPD is not indicated.
CLINICAL AND PROGNOSTIC VALUE
The clinical significance of IE is mainly determined by its type and gradation, the severity of symptoms, the nature of the underlying illness, the stage of heart disease and the functional state of the myocardium.
Schlunoch's extrasystoles, especially without a structural disturbance of the heart, are not dangerous for life. They are detected during ECG HM in most practically healthy individuals of all age groups, and in 10% the stench is polytopic and rarely group. Zagalom SH does not necessarily indicate a concomitant cardiac pathology, and in the absence of cardiac disease is not a predictor of progression of illness and mortality. On the other hand, in patients with severe structural disorders of the heart and myocardial dysfunction, especially against the backdrop of post-infarction cardiosclerosis or heart failure, frequent heart failure is detected and is an additional prognostic factor.
Ectopic activity of the scutulae is detected in 75–90% of patients with acute myocardial infarction in the first 72 years of illness and results in a high frequency of RSS at this time, but does not correlate with mortality over time. u. The presence of illness at a later stage indicates an unfavorable prognosis. Thus, the frequency of IE less than 1 per year is observed in 50% of patients upon discharge from the hospital and indicates a mortality rate of approximately 5%. In most cases (1–10 per year), which occurs in 20% of patients, the mortality rate reaches 20%. Short paroxysms of ST occur in 12% of patients, and mortality from all causes falls to 30% during the first period after suffering MI. The emergence of serious cardiac arrhythmias after MI is associated with the presence of recurrent ischemia with metabolic and electrolyte disorders. Important factors that contribute to arrhythmogenesis are HF and stenosing coronary atherosclerosis.
Children and polytopes are affected in 70–90% of patients with HF, and short episodes of HF – in 40–80%. In this type of heart failure, heart rhythm disturbance is an unfavorable prognostic factor, and 33–47% of all deaths in patients with HF occur in RSS. Arrhythmogenic factors in HF include dysfunction of the left ventricle (EF < 45%), myocardial ischemia, hypoxia, electrolyte disorders, as well as arrhythmogenic effects of congested therapeutic drugs, especially cardiac glycosides, etc. Iuretics and peripheral vasodilators.
The frequency of SE in patients with dilated cardiomyopathy is very high. Thus, frequent and polytopic SH are observed in 80–90% of patients, short episodes of SH are observed in 20–60%. The frequency of RCC is 10% per year and accounts for half of all deaths. In approximately 50% of patients, anterior extrasystoles are detected. The formation of arrhythmias is associated with the presence of severe dysfunction of LS and HF.
Scholastic extrasystoles are recorded in 50–65% of patients with hypertrophic cardiomyopathy with obstruction of the outflow tract of the left cord, including in 32% of patients, and in 14–25% of paroxysms of pharyngitis. The frequency of RCC in these patients is 2.5–9% per river. The atrial extrasystole occurs earlier, lower than the cardiac rhythm. Causes and factors that contribute to arrhythmogenesis: cellular disorganization in different sections of the myocardium, hypoxia, hypokalemia, obstruction of the outflow tract of the left ventricle, diastolic dysfunction of the left ventricle, heart failure, arrhythmogen no infusion of drugs, intense physical exercise.
The risk of RSS due to sulcus rhythm disturbances especially increases in patients with arrhythmogenic dysplasia of the right sac, congenital or inborn QT syndrome, valvular heart disease (including mitral valve prolapse), arterial hypertension єyu.
The level of concern associated with the ECG can be seen in the following specific features of the ECG. As a matter of fact, there are no dangerous extrasystoles with the configuration of the blockade of the left leg of the His bundle and the vertical position of the electrical axis transmitted to the QRS complex (Rosenbaum type) or if the QRS complex of extrasystoles in all thoracic abductions is superior and predicts the graphic for Wolff-Parkinson-White syndrome type A (type Wolf). The QRS complex of such extrasystoles does not have additional splitting, its amplitude becomes 20 mm or more, duration can be up to 0.12 s, and the ST segment and asymmetrical T wave are straightened discordantly to the main tooth of the socket complex. Septal cords with narrow QRS complexes are more often seen in young people due to structural heart disease and are rarely symptomatic. Potziyno groomed, the marshmallow vinike on the fountains of the structural Uzhennnya Cherzi, the form of the block of law of the bunch of Gis, the amplitudu is not the amplitud complex of the QRS (often up to 10 mm) Сdodatki rodsheshchelni, and the triviality of the yogo is more than 0.12–0.14 s. Anomalies of repolarization may be observed: horizontal depression of the ST segment and concordant straightening of the symmetrical, constricted T wave.
CLASSIFICATIONS OF SLUNOCHKOV'S EXTRASYSTOLES
According to the recommendations of the Association of Cardiologists of Ukraine, created on the basis of the International Classification of Diseases X review, the following types of extrasystoles are seen: atrial, atrioventricular, scapular (one by one - up to 30 per year, often - 30 or more per year, arrhythmia, polymorphic, paired, early - type “R to T”).
In Ukraine, when interpreting HM ECG data in patients with sutular rhythm disorders, the classification of B. Lown and M. Wolf (1971) is traditionally used. Based on this classification, there are 5 classes of extrasystoles: 1) monomorphic, < 30 per year; 2) monomorphic, > 30 per year; 3) polymorphic; 4) pairing (4a) and running of ventral tachycardia (4b); 5) early (“R to T”). This classification was developed to systematize heart rhythm disturbances in patients with acute myocardial infarction, but does not meet the needs of stratification of risk and choice of tactics for differential treatment in post-infarction patients ientiv. The reported variants of sulcular disturbances in the cardiac rhythm of the image according to the classification of R. Myerburg (1984), which can be easily recognized when interpreting the results of the ECG HM (Table 3). It is clear that when stratifying the risk in post-infarction patients, it is already about 10 per year. Before arrhythmias of “high gradations”, protect against paroxysms of any kind. Moreover, persistent CT, regardless of the clinical symptoms and the nature of structural heart disease, is seen as a malignant disruption of the rhythm, so the prognostic value of unstable CT lies heavily behind the underlying disease of the heart and function central state of the myocardium. The morphological type of CT also signifies the essential features of the mechanisms of guilt and tactics for managing the sick, sedation, stagnation of AAP and catheter methods of debridement.
Table 3. Systematization of heart rate disturbances according to R. Myerburg (1984)
| Number of extrasystoles | Forms of shunt arrhythmias | Morphology of shunt tachycardias | ||
| Level of severity | Quantity | Level of severity | Characteristics | |
| 0 | No | 0 | No | •Monomorphic •Polymorphic • “Feasting” • From the outflow tract of the right sac •Double-straightened |
| 1 | Rarely (<1 per year.) | 1 | Alone, monomorphic | |
| 2 | Infrequently (2–9 per year.) | 2 | Alone, polymorphic | |
| 3 | Promizhna (10–29 per year.) | 3 | Guys, jogging (2 or 3–5 complexes) | |
| 4 | Often (30–59 per year.) | 4 | Unstable schular tachycardia (6 complexes up to 29 s) | |
| 5 | Very often (≥ 60 per year.) | 5 | Stable tachycardia (≥ 30 s) | |
A well-known prognostic classification of sac arrhythmias was established by JT Bigger (1993), which divides sac arrhythmias into harmless (benign) and unsafe for life (malignant, lethal) and potentially unsafe (potentially lethal).
- Harmless (benign) arrhythmias - be it any kind (rare, frequent, polytopic, young), as well as short episodes of ST for the presence of cardiac pathology, which do not cause hemodynamic impairment . The prognosis for cirrhosis is the same as for a healthy population. There is no indication for antiarrhythmic therapy.
- Unsafe for life (malignant) sculular arrhythmias are episodes of ST that lead to disruption of hemodynamics or fibrillation of the sacs (FS). These arrhythmias, as a rule, are avoided in patients with manifestations of structural disorders of the heart (ICS, persistent HF, cardiomyopathies, heart failure) and impaired speed of heart rate. In these patients, SHE is only part of the spectrum of shlunochkovyh disturbances to the rhythm. They often also show instability and stability.
- Potentially unsafe (potentially malignant) ventricular arrhythmias - frequent, polytopic, partial, short episodes of cardiac arrest in patients with structural heart disorders (ICS, HF, cardiomyopathies, di heart), so as not to disrupt the rhythm until changes in hemodynamics occur. A marker of greater prevalence of life-threatening cardiac arrhythmias in these patients is systolic dysfunction of the heart valve (LV EF <45%).
PRINCIPLES OF ILLNESS MANAGEMENT
Tactics for treating sick people who are suffering from: a) structural heart disease; b) the frequency of extrasystoles, the presence of group extrasystoles or concomitant paroxysms of tachyarrhythmia; c) clinical symptoms associated with arrhythmia. Indications for the use of β-blockers and/or other AAPs are the following clinical situations: 1) progressive progression of heart disease with a significant increase in blood count; 2). 3) arrhythmia (bi-, tri-, quadrigeminia), short runs of ST, which are accompanied by signs of CH; 4) against the background of illness, which is accompanied by an increased risk of life-threatening arrhythmias (mitral valve prolapse, low QT syndrome, etc.); 5) guilt or increase in the frequency of attacks of angina or acute myocardial infarction; 6) saving the SH after an attack of ST and FS; 7) extrasystoles against the background of abnormal conduction patterns (Wolf-Parkinson-White and Clerk-Levy-Kristesko syndromes).
Patients with good health will not require special antiarrhythmic therapy, but dynamic caution is necessary, because in some of them, according to the Framingham investigation, they may be the onset of cardiac disease. In case of extrasystole in a young age without a structural stress of the heart, especially one that appears at the hour of physical exertion, AAP is absolutely not prescribed. In case of subjective intolerance to extrasystole, rational psychotherapy, sedatives, tranquilizers or antidepressants are indicated. The effectiveness of treatment depends on medical indications and varies over three days up to 2–3 months. When a persistent sedative and antiarrhythmic effect is achieved, the dose of the drug over a skin period of 6–7 days is changed by one third to the full dose. As extrasystole occurs against the background of autonomic dysfunction with signs of sympathoadrenal activation, indications of β-blockers, and with dominant vascular-insular symptoms - M-cholinergic drugs (atropine, beladonium preparations, etrop ). Sicknesses with diseases of the internal organs and extrasystole will first require adequate treatment of the underlying disease. In all types of colds, it is aimed at identifying and reducing potential provoking factors of extrasystoles (such as caffeine intake, life situations), as well as accompanying disorders (arterial hypertension).
In case of single monofocal cerebral palsy in patients with cardiac-vascular diseases without impairment of hemodynamics and coronary blood flow, there is no need to prescribe AAP. The approach to the recognition of AAP is that the risk of side effects with drug treatment of “benign” arrhythmias is greater, and the results of treatment are less positive. The management of such patients requires treatment for the underlying illness, as well as the use of sedatives and psychotherapy methods for subjective intolerance to arrhythmia.
Potentially malignant splanchnic arrhythmias often occur against the background of structural heart disease, for example, ICHS or after a history of myocardial infarction. In such patients, in different gradations, there is a danger of further paroxysms of pharyngitis, tremors or fibrillation of the sac. However, patients with potentially malignant splanchnic arrhythmias will require adequate treatment of the underlying illness. This involves the correction of standard risk factors for ICHS (arterial hypertension, chicken, hypercholesterolemia, celiac diabetes). irin, β-blockers, statins) and for heart failure (ACE inhibitors, β-blockers , aldosterone antagonists). In case of established cardiac pathology, often in high grades, obtain adequate antiarrhythmic therapy. The drugs of choice are most often β-blockers, especially for the presence of additional indications: IHS, arterial hypertension, sinus tachycardia. The high effectiveness of these drugs is associated with their antianginal, antiarrhythmic and bradycardic action. If necessary, beta-blockers can be used with class I AAPs (propafenone, ethmozin, etacizin, disopyramide) to ensure their effectiveness.
The hypothesis about the preventive effectiveness of class I AAP in ES in preventing rapto-related death was revised after the results of the CAST study (1989) were published. The use of flecainide and encainide in post-infarction patients with asymptomatic high grades was associated with a significant increase in the risk of raptic death compared with placebo. The phenomenon is believed to be associated with the arrhythmogenic and negative inotropic action of class I AAP. At the same time, the negative evidence from the CAST study and other studies on the effectiveness of the AAP class I do not exclude the possibility of their effective non-invasive treatment for the treatment of ICH in patients with ICD, as well as for other causes of stenosis. arrhythmia.
If β-blockers and class I AAPs are insufficiently effective, amiodarone is prescribed - the most potent antiarrhythmic agent with the lowest level of arrhythmogenic effects. Amiodarone stagnates in case of resistance to other AAPs; In addition, it is the drug of choice in patients with life-threatening and clinically manifested arrhythmias against the background of severe structural heart disease. Encouraging results were obtained with amiodarone in patients with frequent cervical cancer after suffering from myocardial infarction in a meta-analysis of ATMA (1997). In groups of patients who were treated with amiodarone, the prevalence of RCC did not change significantly, but there was no significant change in overall mortality. Amiodarone is the drug of choice for the treatment of ventricular arrhythmias and their use in patients with systolic myocardial dysfunction and HF. Vicristan amiodarone in small doses (200 mg per dose) allows you to minimize the number of non-cardiac side effects. An alternative way to treat patients with splanchnic arrhythmias against the background of IHS is sotalol, a class III AAP with β-blocking agents.
The high effectiveness of amiodarone and sotalol in the treatment of patients with malignant splanchnic arrhythmias does not indicate the existence of safety problems for these patients. Class III AAP will correct the QT interval, and it is safe to set the interval to 440–460 ms. If indicators of the Q-T interval exceed the indicated limits, prolonged QT interval syndrome is diagnosed. A characteristic and specific manifestation of this is the polymorphic CT (pyrating tachycardia), which can be transformed in FS. The risk of developing arrhythmogenic effects with sotalol is greatest in the first three days of taking the drug. The arrhythmogenic effects of sotalol are avoided more often than with amiodarone.
BAGS
Slunochkova extrasystole is the most widespread in clinical practice of heart rhythm disturbances. You may suffer from a large number of cardiac and extracardial illnesses, which can be a common finding in otherwise healthy individuals. A set of current instrumental and laboratory methods for treating patients with directives to identify the causes and mechanisms, quantity and gradation, clinical and prognostic significance, and stratification. this riziku. A comprehensive strategy for the management of sick patients from the neck, sedation, and the effectiveness of arrhythmias with additional anti-arrhythmias are indicated in advance as a result of the development of the potential cortex, treatment for the reduction of arrhythmias, an improvement in the prognosis. annuity and the risk of arrhythmogenic and other side effects of therapy.
RECOMMENDED LITERATURE
- Outpatient ECG monitoring. Current technologies, diagnostic capabilities, indications: Method. Pos_bnik / Bobrov V. O., Zharinov O. Y., Kuts V. O. and spivat. - Lviv: Medicine of the World, 2004. - 68 p.
- Bobrov V. O., Zharinov O. I. Schlunchar arrhythmias (mechanisms of development, influx of myocardial dysfunction, prognostic assessment, differential therapy). - Lviv, 1995. - 122 p.
- Dabrowski A., Dabrowski B., Piotrovich R. Daily ECG monitoring. - M.: Medpraktika, 2000. - 208 p.
- Investigation of heart rate variability in cardiological practice: Method. rec. / Bobrov V. O., Chubuchny V. M., Zharinov O. Y. and spivat. - K: Ukrmedpatentinform, 1999. - 25 p.
- Kushakovsky M. S. Cardiac arrhythmias. - St. Petersburg: IKF “Foliant”, 1998. - 640 p.
- Orlov V.N. Guide to electrocardiography. - M.: Medical Information Agency, 2003. - 526 p.
- Risk stratification and prevention of cardiac death: Method. rec. / Bobrov V. O., Zharinov O. Y., Sichov O. S. and spivat. - K: Ukrmedpatentinform, 2002. — 39 p.
- Functional diagnostics in cardiology / Ed. L. A. Bockeria, E. Z. Golukhova, A. V. Ivanitsky. - M.: Publishing house NTsSSKh im. A. N. Bakuleva RAMS, 2002. - T. 1 - 427 p., t. 2 - 296 p.
Symptoms of arrhythmic syndrome
The clinical picture of extrasystole mainly consists of subjective sensations and is characterized by such symptoms as:
- a feeling of interruptions in the work of the heart, its fading;
- feeling of heart hitting chest;
- anxiety, lack of air;
- weakness, decreased performance;
- pallor, sweating, feeling hot.
The main danger of extrasystoles lies in their ability to develop into more serious rhythm disturbances, such as paroxysmal tachycardia and atrial fibrillation.
The use of gradations for the treatment of extrasystole
Indicating the degree of arrhythmia in the formulation of the diagnosis is very important. The treatment tactics chosen by the doctor will depend on this.
Thus, the presence of extrasystoles of the first gradation in a patient indicates the functional nature of the resulting abnormal contractions. About 60-70% of people experience a similar phenomenon, and this is considered the absolute norm. The only thing required is to periodically check the ECG. However, if you have any symptoms of cardiovascular pathologies, you should undergo additional examination, as this may be one of the first signs of the disease.
If the second gradation is detected without hemodynamic disturbances, non-drug treatment is indicated: auto-training, psychotherapy, avoidance of risk factors. If there are accompanying symptoms or the appearance of polymorphic foci is noticed (third gradation), an appropriate course of antiarrhythmic drugs is required.
Finally, the fourth, fifth, as well as third degree refractory to conservative therapy, especially with hemodynamic disorders, require surgical treatment. In this case, surgical interventions such as catheter radiofrequency ablation or pacemaker implantation may be indicated.
This classification is also used to make a forecast. Ventricular extrasystole of grade 3-5 according to Lown is considered threatening. These are the so-called malignant arrhythmias. They are characterized by a high risk of sudden death. In this case, the patient should be transferred to the intensive care unit.
The location of the lesions also matters. The prognosis is less favorable in the presence of left ventricular arrhythmias.
Types of extrasystole
Extrasystole is classified according to the location of the abnormal focus of activity:
- ventricular;
- ventricular-atrial;
- atrial.
Due to the occurrence:
- extrasystole of functional origin - as a result of the use of nicotine, alcohol, nervous overstrain;
- extrasystole of organic origin - myocardial infarction, cardiomyopathy, heart defects, coronary heart disease;
- extrasystole of toxic origin - as a result of the use of certain medications, during a prolonged febrile state.
Also distinguished:
- bigeminy - characterized by the occurrence of extrasystole immediately after a normal contraction;
- trigeminy - one normal contraction is followed by two extrasystoles, or two normal cardiac complexes are followed by one extrasystole;
- quadrigeminy - three normal contractions occur, followed by an extraordinary contraction.
Principle of classification
There are many factors that characterize a particular disease. As for extrasystoles, the following signs are distinguished:
- number of ectopic areas (mono-, polytopic);
- form of arrhythmia (mono-, polymorphic);
- frequency of occurrence (rare, moderately frequent, frequent);
- localization (right, left ventricular);
- pattern of abbreviations (ordered, unordered);
- frequency (spontaneous, regular).
In accordance with these parameters, many options were proposed: according to Bigger, Mayerburg. However, the Laun-Wolff classification turned out to be the most practical and popular. Ventricular extrasystole according to Laun is determined using so-called gradations, each of which is assigned one number :
- 0 — no arrhythmias over the last 24 hours of observation;
- I - no more than 30 arrhythmias are recorded during an hour of monitoring, monotopic and monomorphic;
- II - more than 30 per hour of the same type;
- III - polymorphic extrasystoles appear;
- IVa - paired monomorphic;
- IVb - paired polymorphic;
- V - characterized by the presence of ventricular tachycardia (extrasystoles that occur more than 3 times in a row).