Possibilities of bisoprolol in the treatment of cardiovascular diseases
In real clinical practice, beta-blockers (BABs) are one of the most widely used drugs in the treatment of cardiovascular diseases (CVD). The issues of choosing BAB still remain relevant.
As is known, beta-1-selective ABs are superior to non-selective ones: they significantly less increase peripheral vascular resistance, to a greater extent reduce the severity of the vasoconstrictor response to catecholamines and, therefore, are more effective in smokers, less likely to cause hypoglycemia in patients with diabetes mellitus (DM), less often cause withdrawal syndrome. Beta-1-selective ABs can be used in patients with obstructive pulmonary diseases; they change the lipid composition of the blood to a lesser extent.
One of the most highly cardioselective beta blockers is bisoprolol (Bidop). The affinity of bisoprolol for beta-1 adrenergic receptors is 75 times higher than for beta 2 adrenergic receptors. In a standard dose, the drug has almost no blocking effect on beta-2 adrenergic receptors and is therefore devoid of many undesirable effects. Bisoprolol in therapeutic dosages (2.5–10.0 mg/day) does not cause bronchospasm and does not impair respiratory function in people with chronic obstructive pulmonary disease (COPD). In addition, bisoprolol does not worsen renal function and intrarenal hemodynamics, does not affect carbohydrate metabolism and does not increase the content of cholesterol and lipoproteins in the blood plasma [1].
These properties determine the use of bisoprolol for various CVDs, primarily for arterial hypertension (AH) and coronary heart disease (CHD).
Benefits of bisoprolol for arterial hypertension
The main indications for the use of beta blockers in patients with hypertension are: coronary artery disease, a history of myocardial infarction, chronic heart failure (CHF), tachyarrhythmias, glaucoma [2].
In terms of antihypertensive activity, bisoprolol is not inferior to other beta blockers and is superior to them in a number of indicators. The double-blind randomized BISOMET trial showed that bisoprolol, like metoprolol, reduces blood pressure (BP) at rest, but is significantly superior to metoprolol in its effect on systolic blood pressure and heart rate (HR) during exercise [3]. The pronounced effectiveness of bisoprolol in patients leading an active lifestyle encourages the drug to be prescribed to younger patients with hypertension.
In this regard, we should recall the myths about the effect of beta-blockers on erectile function. Taking beta blockers is often associated with the possibility of sexual dysfunction. With regard to bisoprolol, the absence of a negative effect on sexual function in men has been convincingly proven. This property of bisoprolol increases adherence to treatment in young male patients who begin to suffer from hypertension in the active years of life. In a study by LM Prisant et al. demonstrated that the incidence of sexual dysfunction when taking bisoprolol did not differ from that when taking placebo [4].
When comparing bisoprolol with calcium antagonists (nifedipine) and angiotensin-converting enzyme inhibitors (ACEIs) (enalapril), it was found that it has no less antihypertensive activity. Moreover, in a comparative randomized study, bisoprolol (10–20 mg/day) led to a significant decrease in left ventricular myocardial mass index (LVMI) by 11%, which was identical to the effect of ACEI (enalapril, 20–40 mg/day) [5] .
Another study examined the effectiveness of bisoprolol in doses of 5–10 mg in patients with hypertension and left ventricular hypertrophy (LVH). After 6 months, the LVMM index significantly decreased by 14.6%, the myocardial thickness of the posterior wall of the left ventricle (LV) and interventricular septum by 8% and 9%, respectively, and the volume of cavities and LV ejection fraction did not change. At the same time, the regression of LV hypertrophy could not be explained by the hypotensive effect alone; in 5 patients who did not reach normal blood pressure values, a decrease in LVMM indices was also noted [6].
Assessment of organoprotective properties, including the effect of various antihypertensive drugs on arterial wall stiffness, is currently the subject of active study and debate. Taking into account the discovery of new markers of cardiovascular risk, we present data on the effect of bisoprolol on central pressure, pulse pressure and vascular wall stiffness. The stiffness of the vascular wall is one of the main factors determining pulse blood pressure. Both vascular wall stiffness and pulse pressure are highly correlated with endpoints such as cardiovascular mortality, myocardial infarction, and stroke. Central, or aortic, pulse pressure has an even closer relationship with cardiovascular risk [7].
Bisoprolol at a dose of 10 mg in patients with hypertension led to a significant decrease in pulse wave velocity, as well as an improvement in the elasticity of the brachial artery.
The ADLIB study examined the effects of different classes of antihypertensive drugs (amlodipine 5 mg, doxazosin 4 mg, lisinopril 10 mg, bisoprolol 5 mg and bendroflumethiazide 2.5 mg) on measures of vascular stiffness - central pressure, reflected wave and augmentation index. The most pronounced decrease in blood pressure in the brachial artery was caused by lisinopril and bisoprolol. Bisoprolol, along with lisinopril and amlodipine, reduced central blood pressure. At the same time, bisoprolol had the opposite effect on the augmentation index and reflected wave speed: the augmentation index was higher when using other drugs, and the reflected wave speed was maximum when treated with bisoprolol [8].
It is impossible not to dwell on aspects of the treatment of hypertension in obese patients. Hypertension is diagnosed in 88% of patients with abdominal obesity [9].
Despite the fact that beta blockers belong to the main class of drugs in the treatment of hypertension, obesity and metabolic syndrome are not the primary indication for their use, although the use of beta blockers in obese patients has a pathogenetic justification, given the key role of hyperactivity of the sympathetic nervous system in the development of hypertension in obesity.
The fear of prescribing beta blockers to a patient with metabolic syndrome is due to fears of worsening the course of diabetes. BAs have different prodiabetogenic potential. Thus, while taking bisoprolol and nebivolol in patients with hypertension and diabetes, there was no change in blood glucose levels, while treatment with atenolol led to a significant increase in its level. It was found that bisoprolol does not change blood glucose levels in patients with diabetes, and no dose adjustment of hypoglycemic agents is required, which indicates its metabolic neutrality [10].
Studies involving patients with diabetes, conducted with bisoprolol, have shown that, due to its high selectivity, the drug does not have a significant effect on carbohydrate and lipid metabolism and can be used in patients with diabetes.
A positive property of bisoprolol for use in obese patients with hypertension is its unique ability to dissolve in both fats and water (amphiphilicity). Due to its amphiphilic properties, bisoprolol undergoes 50% biotransformation in the liver, the rest is excreted unchanged by the kidneys. Considering the frequent presence of a “compromised” liver in patients with metabolic syndrome in the form of non-alcoholic fatty liver disease, the use of bisoprolol is justified for the treatment of hypertension in this category of patients. Amphiphilicity determines the balanced clearance of bisoprolol, which explains the low likelihood of its interaction with other drugs and greater safety when used in patients with moderate hepatic or renal insufficiency [11].
Polymorbidity and the presence of both COPD and CVD in one patient forces a careful approach to the choice of beta blockers. It has been established that the administration of beta blockers to patients with COPD who have suffered a myocardial infarction reduces the risk of mortality by 40% (compared to a similar group of patients without the use of beta blockers). According to S. Chatterjece, in patients with bronchial asthma, changes in bronchial patency when taking 10 and 20 mg of bisoprolol did not differ significantly from those after placebo [12].
The cardioselective beta blocker bisoprolol in patients with CVD and concomitant COPD does not have a negative effect on bronchial patency and improves the quality of life of patients, while the less selective atenolol and metoprolol worsened airway patency in this category of patients [13].
The use of bisoprolol in various forms of ischemic heart disease
Domestic recommendations for the diagnosis and treatment of coronary artery disease [14] consider beta blockers as first-line drugs for the treatment of various forms of coronary artery disease, including serving as a necessary component in the treatment of patients with a history of myocardial infarction and CHF. It is in these clinical situations that beta blockers can improve the prognosis of patients.
Antianginal properties make it possible to prescribe bisoprolol for the prevention of anginal attacks in patients with stable angina pectoris. The multicenter clinical trial TIBBS (Total Ischemic Burden Bisoprolol Study) demonstrated that bisoprolol effectively eliminates episodes of transient myocardial ischemia in patients with stable angina and increases heart rate variability [15]. This study also showed the effect of bisoprolol on improving the prognosis of coronary artery disease. It has been proven that the incidence of cardiovascular events during bisoprolol therapy is significantly lower than when taking nifedipine and placebo.
It was also found that the antianginal effectiveness of bisoprolol is comparable to atenolol, betaxolol, verapamil and amlodipine. Other studies have shown that bisoprolol is more effective in preventing the occurrence of anginal attacks and increases exercise tolerance to a greater extent than isosorbide dinitrate (used as monotherapy) and nifedipine. In patients with stable angina, bisoprolol can be used in combination with other antianginal agents (in particular, nitrates and calcium antagonists).
It was found that bisoprolol significantly reduces the risk of myocardial infarction and mortality from CVD in patients who underwent surgery on the great arteries. As a means of secondary prevention of myocardial infarction, the use of bisoprolol in stable patients who have suffered a myocardial infarction (starting from 5–7 days of the disease) is justified [16].
Choosing bisoprolol
Considering the wide range of medicines on the Russian market and the need for an adequate choice, the problem of interchangeability of original drugs with generics for economic reasons is very relevant. The main limitation in the widespread use of original medicines is their high cost. On the other hand, the fact that the original drug is highly effective is well known. When choosing a generic, it is necessary to have data on therapeutic bioequivalence to the original drug. To prove therapeutic equivalence, a clinical study of a generic drug is required, with comparative clinical studies performed with the original drug to study its effectiveness and safety.
Let us dwell in more detail on the data from clinical studies involving Russian patients with hypertension and coronary artery disease to evaluate the effectiveness of the drug Bidop (bisoprolol).
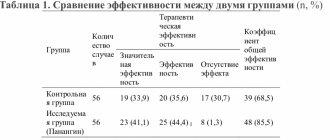
In 2012, K.V. Protasov et al. A comparison was made of the clinical effectiveness and safety of the original and generic bisoprolol preparations for patients with hypertension and patients with exertional angina. 30 patients with grade 1–2 hypertension (average age 47 years) were examined. Patients were randomized into the original bisoprolol and Bidop groups, which were prescribed at a starting dose of 5 mg/day. After 6 weeks of treatment and a 2-week washout period, the drug was replaced with an alternative one, after which therapy was continued for up to 6 weeks. The study diagram is presented in Fig.
At baseline, on the 2nd and 6th weeks of therapy, blood pressure, heart rate, and unwanted side effects were recorded, and the results of self-monitoring of blood pressure (SBP) were analyzed. At baseline and at week 6, 24-hour blood pressure monitoring (ABPM) was performed. By the 6th week of treatment, office blood pressure significantly decreased in the original bisoprolol group by 23.0/10.5 mmHg. Art., in the generic group - by 21.2/10.0 mm Hg. Art., intergroup differences are not significant. The target blood pressure level (<140/90 mmHg) was achieved in the first group in 71.4%, in the second - in 64.3% of patients (p = 0.57). The degree of heart rate decrease also did not differ and amounted to 11.8 and 10.1 beats/min.
According to self-control and 24-hour blood pressure monitoring, unidirectional and comparable in severity shifts in mean blood pressure and heart rate were identified. Another fragment of the study, which included 18 patients with stable angina, showed that both bisoprolol drugs had similar antianginal effects, reducing signs of ischemia. It is important to note that the doses of the original and generic drugs when achieving a similar antianginal effect in the same patients did not differ, which indicates the identity of their antianginal properties.
Both drugs were well tolerated. Clinically insignificant bradycardia was recorded in only two patients treated with the original bisoprolol. This indicates that Bidop is quite well tolerated and safe [17].
According to T.K. Chernyavskaya (2012), the drug Bidop turned out to be completely therapeutically equivalent to the original bisoprolol. Thus, in the group of patients with grade 1–2 hypertension, the target blood pressure level was <140/90 mmHg. Art. reached 72% of those receiving original bisoprolol and 72.5% of those receiving Bidop. At the same time, the doses of bisoprolol required to normalize blood pressure were 9.5 mg for the original drug and 9.3 mg for Bidop. Transfer to combination treatment was required in 34% of those receiving original bisoprolol and in 33% of those receiving Bidop. No side effects occurred during 16 weeks of observation in any group of patients. With the same therapeutic efficacy, the cost of Bidop therapy was lower [18].
It can be concluded that the original bisoprolol and the drug Bidop are clinically equivalent in terms of safety, antianginal and antihypertensive effects. This allows doctors and patients to reduce the cost of treatment without reducing the effect.
Conclusion
Bisoprolol is a leader among beta blockers due to its high cardioselectivity, unique amphiphilic properties, metabolic neutrality, high efficiency and the absence of a negative effect on the course of other diseases. It is important for Russian patients to confirm the therapeutic equivalence of the original drug bisoprolol and its generic (Bidop). The antihypertensive and antianginal effectiveness of bisoprolol, reducing the cost of treatment through the use of high-quality generic drugs can significantly increase the adherence of patients with CVD to treatment.
Literature
- The Task Force on Beta-Blockers of the European Society of Cardiology. Expert consensus document on b-adrenergic receptor blockers // Eur Heart J. 2004; 25: 1341–1362.
- Russian Medical Society for Arterial Hypertension (RMAS), All-Russian Scientific Society of Cardiologists (VNOK). Diagnosis and treatment of arterial hypertension. Russian recommendations (fourth revision), 2010.
- Haasis R., Bethge H. Exercise blood pressure and heart rate reduction 24 and 3 hours after drug intake in hypertensive patients following 4 weeks of trearment with bisoprolol and metoprolol: a randomized multicentre double-blind study (BISOMET)//Eur Heart Jour. 1987; 8; 103–113.
- Prisant LM, Weir MR, Frishman WH, Neutel JM, Davidov ME, Lewin AJ Self-Reported Sexual Dysfunction in Men and Women Treated With Bisoprolol, Hydrochlorothiazide, Enalapril, Amlodipine, Placebo, or Bisoprolol/Hydrochlorothiazide // J Clin Hypertens (Greenwich). 1999, July; 1 (1): 22–26.
- Podzolkov V.I., Osadchiy K.K. Rational choice of beta-blocker for the treatment of arterial hypertension: focus on Bisogamma // Breast Cancer. 2008, vol. 16, no. 16, p. 4–8.
- Teresa E., Gonzdlez M., Camacho-Vazquez C., Tabuenca M. Effect of bisoprolol on left ventricular hypertrophy in essential hypertension // Cardiovasc. Drugs ther. 1994, 8, 837–843.
- Asmar R. Effect of antihypertensive agents on arterial stiffness as evaluated by pulse wave velocity: clinical implications // Am. J. Cardiovasc. Drugs; 2001, 1(5): 387–397.
- Leonova M.V. Beta blockers and organ protection for arterial hypertension // Clinical pharmacology and therapy. 2012, 21 (3), p. 26–30.
- Drapkina O. M., Korneeva O. N., Ivashkin V. T. Activation of the sympathetic nervous system in obesity. How to influence energy homeostasis? // Arterial hypertension. 2011, vol. 17, no. 2, p. 102–107.
- Kukes V. G., Ostroumova O. D., Baturina A. M., Zykova A. A. Beta-blockers in the treatment of arterial hypertension in patients with diabetes mellitus: contraindication or drugs of choice? // Rus. honey. magazine 2002; 10: 446–449.
- Semenov A.V., Kukes V.G. Clinical and pharmacological aspects of the use of bisoprolol // RMJ. 2007, vol. 15, no. 15, p. 38–43.
- Ostroumova O. D., Maksimov M. L. Possibilities of using highly selective beta-blockers in patients with concomitant diseases // Consilium Medicum. 2012; (4), No. 1: 721–725.
- Korneeva O. N. The place of beta-blockers in the treatment of obese patients with hypertension // Doctor. 2011, no. 11, p. 38–40.
- Diagnosis and treatment of stable angina. On Sat. "National Clinical Guidelines". MEDI Expo, 2009, p. 35–74.
- Weber F., Schneider H., von Arnim T. et al. Heart rate variability and ischaemia in patients with coronary heart disease and stable angina pectoris; influence of drug therapy and prognostic value. TIBBS Investigators Group. Total Ischemic Burden Bisoprolol Study // Eur Heart J. 1999; 20 (1): 38–50.
- Syrkin A.L., Dobrovolsky A.V. // Russian Medical Journal. 2010. No. 22. pp. 1352–1355.
- Protasov K.V., Dzizinsky A.A., Shevchenko O.P. et al. Antianginal and antihypertensive effectiveness of bisoprolol: comparison of generic Bidop with the original drug // Pharmateka. 2012, no. 17, p. 57–63.
- Chernyavskaya T.K. Fundamentals of optimal choice among interchangeable drugs in the treatment of cardiovascular diseases // Systemic hypertension. 2012, No. 1, p. 29–32.
O. N. Korneeva, Candidate of Medical Sciences
GBOU VPO First Moscow State Medical University named after. I. M. Sechenova Ministry of Health of the Russian Federation, Moscow
Contact information about the author for correspondence
Bisoprolol
The effectiveness and tolerability of bisoprolol may be affected by concomitant use of other medications. This interaction can also occur when two drugs are taken within a short period of time. The doctor must be informed about taking other medications, even if taken without a doctor's prescription (i.e., over-the-counter drugs).
Combinations not recommended
Treatment of CHF
Class I antiarrhythmic drugs (for example, quinidine, disopyramide, lidocaine, phenytoin; flecainide, propafenone), when used simultaneously with bisoprolol, can reduce AV conduction and myocardial contractility.
All indications for use of the drug Bisoprolol
Blockers of “slow” calcium channels (SCBC) such as verapamil and, to a lesser extent, diltiazem, when used simultaneously with bisoprolol, can lead to a decrease in myocardial contractility and impaired AV conduction. In particular, intravenous administration of verapamil to patients taking beta-blockers can lead to severe arterial hypotension and impaired AV conduction.
Centrally acting antihypertensives (such as clonidine, methyldopa, moxonidine, rilmenidine) can lead to a decrease in heart rate and cardiac output, as well as vasodilation due to a decrease in central sympathetic tone. Abrupt withdrawal, especially before discontinuation of beta-blockers, may increase the risk of developing “rebound” arterial hypertension.
Combinations requiring special caution
Treatment of arterial hypertension and angina pectoris
Class I antiarrhythmic drugs (for example, quinidine, disopyramide, lidocaine, phenytoin; flecainide, propafenone), when used simultaneously with bisoprolol, can reduce AV conduction and myocardial contractility.
All indications for use of the drug Bisoprolol
BMCC dihydropyridine derivatives (for example, nifedipine, felodipine, amlodipine) when used simultaneously with bisoprolol may increase the risk of arterial hypotension. In patients with CHF, the risk of subsequent deterioration in cardiac contractility cannot be excluded. Class III antiarrhythmic drugs (eg, amiodarone) may worsen AV conduction disturbances.
The effect of beta-blockers for topical use (for example, eye drops for the treatment of glaucoma) may enhance the systemic effects of bisoprolol (lowering blood pressure, lowering heart rate).
Parasympathomimetics, when used simultaneously with bisoprolol, may enhance AV conduction disturbances and increase the risk of developing bradycardia.
The hypoglycemic effect of insulin or oral hypoglycemic agents may be enhanced. Signs of hypoglycemia - in particular tachycardia - may be masked or suppressed. Such interactions are more likely when using non-selective beta-blockers.
Agents for general anesthesia may increase the risk of cardiodepressive effects, leading to arterial hypotension (see section "Special Instructions").
Cardiac glycosides, when used simultaneously with bisoprolol, can lead to an increase in impulse conduction time, and thus to the development of bradycardia.
Nonsteroidal anti-inflammatory drugs (NSAIDs) may reduce the antihypertensive effect of bisoprolol.
The simultaneous use of Bisoprolol with beta-agonists (for example, isoprenaline, dobutamine) may lead to a decrease in the effect of both drugs.
The combination of bisoprolol with adrenergic agonists that affect beta and alpha adrenergic receptors (for example, norepinephrine, epinephrine) may enhance the vasoconstrictor effects of these drugs that occur with the participation of alpha adrenergic receptors, leading to an increase in blood pressure. Such interactions are more likely when using non-selective beta-blockers.
Antihypertensive drugs, as well as other drugs with a possible antihypertensive effect (for example, tricyclic antidepressants, barbiturates, phenothiazines) may enhance the antihypertensive effect of bisoprolol.
Mefloquine, when used simultaneously with bisoprolol, may increase the risk of bradycardia.
MAO inhibitors (except MAO B inhibitors) may enhance the antihypertensive effect of beta-blockers. Concomitant use may also lead to the development of a hypertensive crisis.
Allergens used for immunotherapy or allergen extracts used in skin testing increase the risk of anaphylactic reactions.
The clearance of lidocaine and xanthines (except theophylline) may be reduced due to a possible increase in their concentration in the blood plasma, especially in patients with an initially increased clearance of theophylline under the influence of smoking.
The effect of non-depolarizing muscle relaxants and the anticoagulant effect of coumarins may be prolonged during treatment with bisoprolol.
When used simultaneously with rifampicin, a slight decrease in the half-life of bisoprolol is possible due to the induction of hepatic isoenzymes of cytochrome P450 by rifampicin. Usually no dose adjustment is required.
Non-hydrogenated ergot alkaloids and ergotamine increase the risk of developing peripheral circulatory disorders.
Sulfasalazine increases the concentration of bisoprolol in the blood plasma.
BISOPROLOL-PRANA (tablets)
and with all this, the pressure drops sharply - to 90/40, and the pulse at the same time - 163 beats per minute, Oy!
And it has happened that after a minor load, for example playing volleyball, something similar happens. At first this happened once every six months and I did not pay attention to it, but after this phenomenon began to repeat almost every month, I was forced to see a doctor. The cardiologist wrote out a prescription and at the same time a referral for examination and treatment to the hospital, and that’s how I ended up in the cardiology department of the hospital. And after discharge, I discovered in the epicrisis, signed by the head of the department, that I needed to take Bisoprolol tablets for a year, half a tablet of 5 mg dosage once a day every day. The diagnosis is tachycardia, the pills seem to be suitable, but the annotation says that in addition to lowering the heart rate, they also reduce blood pressure, and my blood pressure has always been slightly below normal -110/70. Therefore, I was very surprised when I discovered this drug at home, in the discharge summary, and just in case, I went to the clinic, also to a cardiologist, for a consultation. The doctor firmly assured and confirmed that this medicine would suit me and there was no reason to worry. Although I laughed that Bisoprolol is somewhat outdated today and now there are more modern analogues, and indeed on the Internet I found information that Bisoprolol was discovered back in the sixties of the last century. But there are few side effects, “relatively” of course, and what worried me most was the situation with blood pressure. Probably in my eyes, after all, the doctor read the doubts and immediately offered to get this drug for free at the departmental pharmacy and wrote out a prescription for it. I had to agree, there is only one life. This box contained 3 plates of ten tablets each. I cut the tablets in half every morning with a knife along the line marked on them. In principle, it’s convenient, and I put the remaining half of the tablet back into the blister for storage. Well, I washed them down with water from this cooler. The package lasted me exactly two months. Our medicine’s manufacturer is the pharmaceutical company Pranafarm LLC, Samara. I can’t describe the taste of the tablets, since I swallowed them without chewing. This is what the doctor prescribed, and I had no desire to chew them. Probably bitter, like all pills. And now about health. The pills helped. My heart calmed down, my blood pressure did not drop two months after I started taking Bisoprolol, and my health improved. True, I just can’t forget the words of the head of the cardiology department upon discharge from the hospital: “We will meet again.” Now I decided to take a short break from taking Bisoprolol, let my tummy rest a little from the chemicals. The bottom line is clear to me: the medicine is good, but I will not recommend it, do not self-medicate, go to the doctor if you find similar symptoms as mine, although it helped me. Don't get sick, take care of yourself, have a good mood.
How to take Bisoprolol
Bisoprolol should be taken exactly as prescribed by your doctor.
If you have any doubts about taking the drug, you should consult your doctor or pharmacist before use.
Treatment with Bisoprolol requires regular medical supervision. This is especially important at the beginning of treatment, during dose increases and when stopping treatment.
Bisoprolol tablets should be taken with a small amount of water in the morning, with or without food. Do not crush or chew the tablets.
Treatment with Bisoprolol is usually long-term.
Adults including the elderly:
Treatment with Bisoprolol should start with a low dose and increase gradually.
Your doctor will decide how to increase your dose and this is usually done as follows:
- 1.25 mg bisoprolol once a day for one week, then
- 2.5 mg bisoprolol once a day for one week, then
- 3.75 mg bisoprolol once a day for one week, then
- 5 mg bisoprolol once a day for four weeks, then
- 7.5 mg bisoprolol once a day for four weeks, then
- 10 mg bisoprolol once daily for maintenance therapy
The maximum recommended daily dose is 10 mg of bisoprolol.
Depending on how well you tolerate the drug, your doctor may also decide to lengthen the interval between dose increases. If your condition worsens or you can no longer tolerate the effects of this drug, you may need to reduce your dose or stop treatment. In some patients, a maintenance dose of less than 10 mg of bisoprolol may be sufficient.
Usually the doctor's prescription is correct in this situation.
If you must stop treatment completely, your doctor will, as usual, advise you to gradually reduce your dose as otherwise your condition may worsen.
If you have used more Bisoprolol than recommended
If you take more Bisoprolol tablets than recommended, immediately tell your doctor. Your doctor will decide what measures are needed.
Symptoms of overdose may include palpitations, difficulty breathing, dizziness, or trembling (due to low blood sugar).
If you forget to take Bisoprolol
Do not take a double dose to make up for a missed dose. Take your scheduled dose the next morning.
If you stop taking Bisoprolol a
You should not stop taking bisoprolol unless your doctor advises you to. Otherwise, your condition may become much worse.
If you have any additional questions about the use of the drug, you should contact your doctor or pharmacist.
Possible side effects
Like other medicines, bisoprolol can cause side effects, although not everyone gets them.
To prevent serious side effects from developing, talk to your doctor right away if side effects are severe, develop suddenly, or get worse quickly.
The most serious side effects related to cardiac function are:
- slow heart rate or bradycardia (may affect more than 1 in 10 people),
- worsening heart failure (may affect 1 in 10 people),
- slow or irregular heartbeat (may affect 1 in 100 people).
If you experience dizziness, or weakness, or difficulty breathing, please tell your doctor as soon as possible.
Additional side effects are listed by frequency of occurrence.
Common (may occur in 1 in 10 people);
- fatigue, weakness, dizziness, headache,
- feeling of coldness or numbness in the arms or legs,
- low blood pressure,
- gastrointestinal problems such as nausea, vomiting, diarrhea or constipation.
Uncommon (may affect 1 in 100 people):
- sleep disorders,
- depression,
- dizziness when standing up
- respiratory problems in patients with bronchial asthma or chronic lung diseases,
- muscle weakness, muscle cramps.
Rare (may affect 1 in 1,000 people):
- hearing problems,
- allergic rhinitis,
- reduction of lacrimation,
- inflammation of the liver, which can lead to yellowing of the skin or whites of the eyes,
- disturbances in the levels of various lipids and liver markers in the blood,
- allergic reactions such as itching, swelling, rash,
- erectile dysfunction,
- nightmares, hallucinations,
- fainting.
Very rare (may affect 1 in 10,000 people):
- irritation and redness of the eyes (conjunctivitis),
- hair loss,
- development and worsening of psoriasis.
Side Effect Reporting:
If you notice any side effects, tell your doctor, pharmacist or pharmacist, including any side effects not listed in this leaflet. You can also report side effects by going to the website www.arpimed.com and filling out the appropriate form “Report a side effect or ineffectiveness of a drug” and to the Scientific Center for Expertise of Medicines and Medical Technologies named after. Academician E. Gabrielyan by going to the website www.pharm.am to the “Report a side effect of a drug” section and fill out the form “Card of reporting a side effect of a drug.” Scientific center hotline phone number: +37410237665; +37498773368.
How to store Bisoprolol
- Store out of reach of children, protected from moisture and light at a temperature of 15-25º C.
- Shelf life – 3 years. Do not take Bisoprolol after the expiration date indicated on the drug packaging. When indicating the expiration date, we mean the last day of the specified month.
Medicines should not be disposed of in wastewater or sewer systems. Ask your pharmacist how to dispose of any medicine you no longer need. These measures are aimed at protecting the environment.
Package contents and additional information
What Bisoprolol contains
Active substance: bisoprolol fumarate – 5 mg
Other components: core - microcrystalline cellulose, povidone, sodium starch glycolate, magnesium stearate, corn starch, Aerosil 200; shell - purified talc, propylene glycol, titanium dioxide, hypromellose, yellow dye E-110, red dye E-129.
What Bisoprolol looks like and contents of the package :
Yellow-orange heart-shaped tablets.
Description of packaging
10 film-coated tablets in blister packs (PVC/aluminium). 3 blister packs (30 tablets) together with an insert leaflet are placed in a cardboard package.
Vacation conditions
Available with prescription
Bisoprolol, 30 pcs., 5 mg, film-coated tablets
The effectiveness and tolerability of bisoprolol may be affected by the simultaneous use of other drugs. This interaction can also occur when two drugs are taken within a short period of time.
The doctor must be informed about the use of other medications, even if they are used without a doctor’s prescription (that is, over-the-counter drugs).
Combinations not recommended
Class I antiarrhythmic drugs (for example, quinidine, disopyramide, lidocaine, phenytoin, flecainide, propafenone), when used simultaneously with bisoprolol, can reduce AV conduction and myocardial contractility.
Blockers of “slow” calcium channels (SCBC) such as verapamil and, to a lesser extent, diltiazem, when used simultaneously with bisoprolol, can lead to a decrease in myocardial contractility and impaired AV conduction. In particular, intravenous administration of verapamil to patients taking beta-blockers can lead to severe arterial hypotension and impaired AV conduction.
Centrally acting antihypertensives (such as clonidine, methyldopa, moxonidine, rilmenidine) can lead to a decrease in heart rate and cardiac output, as well as symptoms of vasodilation due to a decrease in central sympathetic tone. Abrupt withdrawal, especially before discontinuation of beta-blockers, may increase the risk of developing “rebound” arterial hypertension.
Combinations requiring special caution
BMCC dihydropyridine derivatives (for example, nifedipine, felodipine, amlodipine) when used simultaneously with bisoprolol may increase the risk of arterial hypotension. In patients with CHF, the risk of subsequent deterioration in cardiac contractility cannot be excluded.
Class III antiarrhythmic drugs (for example, amiodarone), when used simultaneously with bisoprolol, may increase AV conduction disturbances.
The effect of beta-blockers for topical use (for example, eye drops for the treatment of glaucoma) may enhance the systemic effects of bisoprolol (lowering blood pressure, lowering heart rate).
Parasympathomimetics, when used simultaneously with bisoprolol, may enhance AV conduction disturbances and increase the risk of developing bradycardia.
The hypoglycemic effect of insulin or oral hypoglycemic agents may be enhanced. Signs of hypoglycemia, in particular tachycardia, may be masked or suppressed. Such an interaction is more likely when using non-selective beta-blockers.
General anesthesia products
Can increase the risk of cardiodepressive effects, leading to arterial hypotension (see section "Special Instructions").
Cardiac glycosides
When used simultaneously with bisoprolol, they can lead to an increase in impulse conduction time, and thus to the development of bradycardia.
Nonsteroidal anti-inflammatory drugs (NSAIDs)
May reduce the antihypertensive effect of bisoprolol.
The simultaneous use of Bisoprolol with beta-agonists (for example, isoprenaline, dobutamine) may lead to a decrease in the effect of both drugs.
The combination of bisoprolol with adrenergic agonists that affect alpha and beta adrenergic receptors (for example, norepinephrine, epinephrine) may enhance the vasoconstrictor effects of these drugs that occur with the participation of alpha adrenergic receptors, leading to an increase in blood pressure. Such interactions are more likely when using non-selective beta-blockers.
When bisoprolol is combined with norepinephrine and epinephrine, aggravation of intermittent claudication may occur.
Antihypertensive drugs, as well as other drugs with a possible antihypertensive effect (for example, tricyclic antidepressants, barbiturates, phenothiazines) may enhance the antihypertensive effect of bisoprolol.
Allergens used for immunotherapy or allergen extracts used in skin testing increase the risk of anaphylactic reactions.
The clearance of lidocaine and xanthines (except theophylline) may be reduced due to a possible increase in their concentration in the blood plasma, especially in patients with an initially increased clearance of theophylline under the influence of smoking.
Tricyclic and tetracyclic antidepressants, antipsychotics (neuroleptics), ethanol, sedatives and hypnotics increase depression of the central nervous system.
Diuretics, sympatholytics, hydralazine and other antihypertensive drugs can lead to an excessive decrease in blood pressure.
The effect of non-depolarizing muscle relaxants and the anticoagulant effect of coumarins may be prolonged during treatment with bisoprolol.
Mefloquine
When used simultaneously with bisoprolol, it can increase the risk of developing bradycardia.
MAO inhibitors (except MAO B inhibitors)
May enhance the antihypertensive effect of beta-blockers. Concomitant use may also lead to the development of a hypertensive crisis. The break between taking MAO inhibitors and bisoprolol should be at least 14 days.
Rifampicin
There may be a slight decrease in the half-life of bisoprolol due to the induction of hepatic isoenzymes of cytochrome P450 by rifampicin. Usually no dose adjustment is required.
Ergotamine derivatives
Non-hydrogenated ergot alkaloids increase the risk of developing peripheral circulatory disorders. Ergotamine increases the risk of developing peripheral circulatory disorders.
Sulfasalazine increases the concentration of bisoprolol in the blood plasma.