Monocytes are synthesized in the bone marrow, from where they enter the systemic circulation, where they live for up to 3 days. Next, they will face either apoptosis (cell death programmed by nature), or improvement to the level of macrophages due to the growth of their internal structures - lysosomes and mitochondria. This improvement allows monocyte macrophages to more effectively perform their direct function - eliminating pathogenic microorganisms.
In addition to phagocytosis, monocytes perform several other useful functions:
- participate in allergic reactions, identifying foreign proteins;
- prevent the formation of malignant tumors;
- regulate the processes of hematopoiesis and coagulation (blood clotting);
- dissolve blood clots;
- help the body develop specific immunity to certain types of bacteria and viruses.
Blood test for monocytes
Figure 1. Leukocyte blood count.
Image: mikrostoker / Depositphotos A complete blood count is used to determine the level of monocytes. Typically, this study requires capillary blood (taken from a finger), but sometimes venous blood can also be used. In analysis forms, monocytes are also referred to as MON and MONO. Their normal content in the blood is 3-11%, and in absolute value - 0.04-0.08 * 109 / liter.
The normal level of monocytes in the blood does not depend on the gender of the patient. Pregnant women may experience a physiological increase in the number of monocytes, but this does not go beyond the normal range.
Indications for analysis
A general blood test to determine the leukocyte formula and monocyte level is prescribed to almost all patients who visit the clinic. The most common indications:
- viral or bacterial infections;
- oncological neoplasms;
- autoimmune diseases (Crohn's disease, rheumatoid arthritis, etc.);
- diseases of the circulatory system;
- helminthic infestations;
- inflammatory diseases of the kidneys, liver and any other organs;
- injuries, burns, frostbite.
Reasons for promotion and demotion
Monocytes (the norm for women by age, a table of clinical indicators is compiled based on the results of a diagnostic examination of the body) are blood cells that are part of the body’s immune system, and an increase in their concentration indicates the possible presence of the following diseases:
- infection of the digestive system by helminths;
- invasion of bacterial, viral and fungal microorganisms;
- tuberculosis of the lymphatic system or lung tissue;
- typhoid fever;
- all types of sexually transmitted diseases (the most dramatic surge in monocyte activity is observed in the case of infection with syphilis);
- brucellosis;
- lymphomas of malignant etiology;
- monocytic leukemia of a specific type;
- blood damage by the malaria pathogen;
- all types of malignant neoplasms that are localized in any part of the body;
- herpesvirus infection, which was in a chronic form, and then moved to the acute stage;
- endocarditis and rheumatoid tissue destruction;
- skin damage associated with the parasitic activity of infectious microorganisms, acute allergic reaction or mechanical trauma.
During menstruation, most women allow a slight increase in the level of monocytes, which returns to normal 2-3 days after the end of menstruation. Such a reaction of the body is not a pathology.
A decrease in the concentration of phagocytes can be caused by the following reasons:
- internal bleeding;
- postoperative period of tissue restoration;
- severe traumatic brain injury;
- malignant neoplasms in the bone marrow;
- long-term therapy with Prednisolone, cytotoxic drugs, as well as immunosuppressants;
- state of shock;
- prolonged stay in conditions of psycho-emotional overstrain and stress;
- postpartum period;
- presence of aplastic anemia.
A decrease in the level of phagocytes is no less an alarming signal than an increase in their number. The reasons that caused the change in the cellular composition of the blood must be established in a biochemical laboratory.
Preparing for analysis
When preparing for a general blood test, you should follow just a few simple rules:
- take the test in the morning on an empty stomach;
- the day before the test, avoid heavy physical activity;
- Avoid alcohol, fatty and spicy foods for 2 days;
- On the day of the study, do not smoke and avoid nervous stress.
Refusal of physical activity is especially important on the day of the study, so it is advisable to avoid even fast walking and climbing stairs on the way to the clinic.
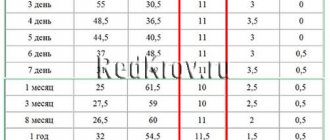
The normal level of monocytes in the blood
The level of monocytes in the blood depends on the patient's age. If we consider absolute values, that is, the content per liter of blood, then the norms look like this:
- Children under 12 years old: from 0.05 to 1.1 * 109 / liter.
- Children over 12 years old: from 0.04 to 0.08 * 109 / liter.
For convenience, fluctuations in percentages depending on age are given in the table.
Table 1. Normal monocyte levels in adults and children
| Age | Normal monocyte percentage |
| Newborns | 5 – 15% |
| Children from 2 weeks to one year | 4 – 10% |
| 1 – 2 years | 3 – 10% |
| 2 – 15 years | 3 – 9% |
| 16 years and older | 3 – 11% |
Decoding the general blood test of adults: norm and pathology
Like most diagnostic tests, a complete blood count is performed in the morning and on an empty stomach. The result - a summary table of indicators - can be available either the same or the next day. What does a general blood test include?
Here are the most common general blood test indicators examined in a clinical laboratory:
- hemoglobin;
- red blood cell count;
- color index;
- reticulocyte count;
- platelet count;
- ESR;
- leukocyte formula;
- hematocrit;
and so on.
Let us consider these indicators and their norms in the blood of a healthy person in more detail. Let's start with hemoglobin (Hb) - one of the most important components of red blood cells [3]. If hemoglobin is reduced, this may indicate a lack of iron [4] (it is used in the process of hemoglobin synthesis) or vitamin B12 in the body, and be the first sign of developing anemia. A significant (several times) increase in hemoglobin may indicate that the patient has pulmonary or heart failure. Increased hemoglobin can also be observed in cases of oncological diseases and kidney pathology, but not a single highly qualified doctor, as mentioned above, will make a final diagnosis based on a general blood test alone, therefore, even if hemoglobin in the blood is greatly increased, There is no need to panic in advance. The norms for this indicator for adults approximately look like this: 131–173 g/l for men 18–64 years old and 117–160 g/l for women of the same age.
Red blood cells (RBCs) are transport cells. They deliver oxygen to all tissues and organs and take away carbon dioxide.
The average normal erythrocyte count for adult men 18–64 years old is considered to be 4.2–5.7 × 1012/L, and for women – 3.8–5.3 × 1012/L. A reduced number of red blood cells may indicate anemia as a result of a deficiency in the body of iron, vitamin B12 or blood loss - for example, with heavy menstruation in women, hidden bleeding. An increased number of red blood cells occurs in people who have been high in the mountains for some time, where the air is thin. Such a change is adaptive in nature and is the norm. Also, increased concentrations of red blood cells may indicate to the doctor that the patient has problems with the hematopoietic, respiratory or cardiovascular system. That is why it is very important, after receiving test results, not to self-medicate under any circumstances. You need to contact a specialist.
Reticulocytes (RTC) are young cells that perform the function of a “blank” for older cells[5]. By the speed with which they appear in the bloodstream, the doctor can judge the functioning of the bone marrow, kidneys, as well as the patient’s blood itself. Normally, in adult men the rate is 0.2–1.92%, in women – 0.2–2.07%. Elevated reticulocytes can be either normal or a deviation from it. So, for example, if a patient has recently lost a lot of blood and reticulocytes are elevated, this is normal. If there was no blood loss, an increased percentage of reticulocytes may indicate the presence of diseases such as hemolytic anemia or malaria [6]. In patients with cancer, an increase in reticulocytes may indicate metastases to the bone marrow. A decrease in level is a signal that the kidneys or bone marrow are affected, or that these organs are depleted due to prolonged erythropoiesis. This may also indicate metastases in the bone marrow: unfortunately, it is impossible to predict which part of the bone marrow the tumor will metastasize to and how this will affect reticulocytes - in the direction of reducing or, conversely, increasing cell growth.
ESR (ESR) is the erythrocyte sedimentation rate . In women under 50 years of age, the rate should not exceed 20 mm/hour, in older women - 30 mm/hour. For men under 50 years of age, the norm is 15 mm/hour, and after 50—20 mm/hour. If the ESR is elevated, this may indicate the presence of an inflammatory process in the body, poisoning, anemia, or large blood loss.
The color index (average erythrocyte hemoglobin concentration) (MCHC) of blood indicates how saturated the red blood cells are with hemoglobin. Normally it will look like this: from 300 to 380 g/l. A decrease indicates possible thalassemia or iron deficiency; an increased rate may indicate a deficiency of vitamin B12 and folic acid in the body.
The main function of platelets (PLT) is to stop bleeding by forming a blood clot[7]. The normal platelet level is 180–320 × 109/L. An increase in the platelet count may indicate to the doctor the presence of injury, possibly a malignant tumor, an infectious process, or some other diseases. Thrombocytosis may be temporary and disappear when the condition returns to normal - for example, if a person has recently undergone surgery. Low platelets often indicate poisoning of the body with chemicals, the presence of an infectious disease, an autoimmune process, deficiency of vitamin B12 and folic acid, leukemia in acute or chronic form. The result of platelet levels in the blood is also affected by the use of certain medications, so it is very important to tell the doctor what medications the patient is currently taking to enable the specialist to formulate the correct diagnostic picture.
White blood cells (WBCs) in the body are responsible for immunity, and their numbers can indicate to the doctor that the body is in a state of fight against viruses, foreign bodies, pathogens or toxins. The normal white blood cell count may vary slightly depending on a person's age (see table below), but generally ranges from 4.5 to 11.3 x 109/L. A decrease in the indicator can be observed, for example, with blood diseases, viral infections, enlarged spleen and during chemotherapy. A high level may indicate the presence of a bacterial, fungal, viral infection in the body, acute bleeding, and so on.
Lymphocytes (LYM) are the main “building blocks” of the immune system. The normal level in the blood of an adult is 1.2–3.0 × 109/l. If the concentration is increased, wide-spectrum infectious diseases are usually diagnosed[8]. Low levels often indicate renal or immune failure, chronic diseases, and are also observed with long-term use of corticosteroids.
The leukocyte formula helps determine the presence of infectious diseases and oncological processes by the ratio of certain types of leukocytes to each other.
If neutrophils are higher than normal, which is 47–72% of the total number of particles of this class, this may indicate infectious diseases (sinusitis, sore throat, bronchitis, pneumonia, etc.), an inflammatory process (arthritis, pancreatitis, etc.), chronic metabolic disorders substances, heart attack or allows one to suspect the presence of a malignant neoplasm. With neutropenia - a low level of neutrophils - infectious diseases such as typhoid fever, influenza, brucellosis, measles, rubella and others may be present. This may also indicate recent treatment with radiotherapy or chemotherapy, or the use of antiviral drugs.
Eosinophils (EOS) are normally present in the blood in a ratio of 1–5% of the total number. If the indicator is higher, this can tell the doctor about the patient’s allergies, parasitic infestations, infectious diseases (scarlet fever, tuberculosis and others), malignant tumors, leukemia and other diseases of the hematopoietic system[9]. Eosinophils in the blood decrease with heavy metal poisoning, sepsis or the onset of an inflammatory process.
Basophils (BAS) are normally practically undetectable in the blood of a healthy person, as they make up up to 1% of the total number of cells. An increase in the formula may indicate the development of diseases such as nephrosis, hemolytic anemia, chicken pox, hypothyroidism, chronic myeloid leukemia, Hodgkin's disease, drug or food allergies, taking hormonal drugs, ulcerative colitis, or observed after removal of the spleen.
Monocytes (MON) are responsible for engulfing dead cells and bacteria. An increased level of monocytes indicates diseases such as rheumatoid arthritis, syphilis, mononucleosis, tuberculosis and other infectious diseases. A decrease is observed when taking corticosteroids or after major operations.
This is interesting
All parts of the human body are supplied with oxygen through the blood. The only exception is the cornea of the eye - it does not have blood vessels[10]. The cornea must be perfectly transparent, so oxygen dissolved in tears enters its cells directly from the air.
Table of normative (reference) indicators of clinical blood analysis of adult men and women
It is better, as mentioned above, to entrust the interpretation of the analysis indicators to a doctor, since the results may vary depending on the patient’s age, gender and other factors[11]. These reference values (normal limits) may also vary depending on the laboratory.
| Indicator name | Designation | Norm |
| Red blood cell count | R.B.C. | for men: 18–44 years old - 4.3–5.7 × 1012/l; 45–64 years old - 4.2–5.6 × 1012/l; from 65 years old - 3.8–5.8 × 1012/l |
| for women: 18–44 years old - 3.8–5.1 × 1012/l; 45–64 years old - 3.8–5.3 × 1012/l; from 65 years old - 3.8–5.2 × 1012/l | ||
| Hemoglobin | HGB, Hb | for men: 18–44 years old – 132–173 g/l; 45–64 years old – 131–172 g/l; from 65 years old - 126–174 g/l |
| for women: 18–44 years old - 117–155 g/l; 45–64 years old – 117–160 g/l; from 65 years old - 117–161 g/l | ||
| Hematocrit | HCT | for men: 18–44 years old – 39–49%; 45–64 years old – 39–50%; from 65 years old - 37–51% |
| for women: 18–44 years old - 35–45%; after 45 years - 35–47% | ||
| Platelet count | RLT | 180–320 × 109/l |
| White blood cell count | WBC | 4.5–11.3 × 109/l |
| Granulocyte count | GRA, GRAN | up to 0.09 × 109/l; or up to 0.6% |
| Monocyte count | MON | 0.09–0.60 × 109/l; or 3–11% |
| Lymphocyte content | LYM, LY% | 1.2–3.0 × 109/l; or 19–37% |
| Red blood cell distribution width | RDWc | 11,6–48,8 % |
| Average red blood cell volume | MCV | 80–100 fl |
| Average hemoglobin concentration in erythrocyte | MCHC | 300–380 g/l |
| Average hemoglobin content in an erythrocyte | MCH | 27–35 pg |
| ESR (erythrocyte sedimentation rate) | ESR | for men: 18–49 years old - up to 15 mm/h; after 50 years - up to 20 mm/h |
| for women: 18–49 years old - up to 20 mm/h; after 50 years - up to 30 mm/h |
Changes in each individual or several indicators of a general blood test may be characteristic of various diseases. In order to correctly “read” the results form, the doctor needs to know as much as possible about the patient: from symptoms and time of onset of illness to dietary supplements that he has recently consumed. You should definitely share this information with your doctor.
Causes of high levels of monocytes in the blood
An increase in the level of monocytes in the blood is called monocytosis. It is noted in the following cases:
- infectious diseases;
- acute and chronic inflammatory processes;
- helminthic infestations;
- recovery period after injury or surgery;
- oncological neoplasms;
- poisoning with toxic substances (including alcohol);
- autoimmune systemic diseases;
- diabetes.
Monocytosis can also be of a purely physiological nature. For example, monocyte levels increase within a few hours after eating. In women during menstruation, monocytosis is observed in response to the rejection of endometrial cells.
Figure 2. Monocytosis. Image: Leukemia Research Reports / ResearchGate (CC BY-NC-ND)
Monocytosis in children
Separately, I want to talk about monocytosis in children. This has recently become a fairly common condition, and parents and, unfortunately, not even medical workers always know what to think about with monocytosis and what pathological causes can cause an increase in the number of monocytes in children.
- Firstly, these are diseases caused by bacteria, fungi and viruses. In principle, any of these “friends” can cause an increase in monocytes in the child’s blood.
- Infection with worms. This reason can even be put in first place in children's practice.
- Inflammatory processes in the gastrointestinal tract. And that condition of the gastrointestinal tract, which we call: intestinal dysbiosis, which is also not a diagnosis, but it is the microbiota that can determine the concentration of monocytes and cause monocytosis.
- Food poisoning. And any other poisoning can cause monocytosis in a child’s body.
- Allergic reactions in a child. If we talk about young children, then this is predominantly a genetically determined food allergy. If we talk about older children, then these may be allergic reactions associated with the same parasitosis, helminthic infestations, protozoan infections, or the consumption of food products containing a lot of preservatives, allergens, all kinds of stabilizers, etc., that is, not Completely suitable food for a child.
- Oncological diseases of the blood. Of course, they can also cause monocytosis, and, first of all, these are leukemia and lymphoma.
- Autoimmune pathology of children.
- Rheumatoid arthritis or juvenile rheumatoid arthritis.
- Systemic lupus erythematosus.
- Crohn's disease.
- Infectious processes after surgical interventions can also cause monocytosis, and this will be one of the body’s protective reactions.
If we talk about monocytosis in pediatric practice, then, of course, first of all it will be associated with acute respiratory viral infections, diseases of an infectious nature, and bacterial diseases of the gastrointestinal tract. Therefore, on the one hand, there is no need to be afraid of monocytosis, but on the other hand, this is a blood indicator that can indicate some serious, still hidden problems that are not clearly manifested clinically. And this is a reason to conduct more in-depth research on a specific person.
That’s basically all I wanted to tell you about monocytes. If you have any questions, you can write to us or ask them in the comments. And if everything is clear to you, I was glad to give you this information. Come see us if the need arises and stay healthy.
Causes of low levels of monocytes in the blood
A decrease in the level of monocytes in the blood below the age-appropriate norm is called monocytopenia.
Possible causes of low monocyte count:
- Aplastic anemia. This is a life-threatening condition that is caused by failure of the maturation of blood cells in the bone marrow.
- Oncohematological diseases. Late stages of leukemia are characterized by suppression of hematopoiesis, therefore, among other things, the number of monocytes in the blood decreases.
- Purulent bacterial infections. Such diseases include bacterial pneumonia, boils, cellulitis, and sepsis.
- Taking medications. Cytostatics and corticosteroids have the greatest effect in this regard.
Differences between macrophages and monocytes
Until the 70s of the 20th century, scientists were convinced that all monocytes eventually transform into macrophages. Any additional sources of the appearance of “cleaners” have not been identified. And only in 2008, after a series of studies, it was established that macrophages have different origins. Some of them are transformed from monocytes, the rest develop from precursor cells of various types during intrauterine development of the fetus.
The transformation of one cell into another goes through certain stages. After monocytes enter the internal tissues from the blood, their active growth begins. At the same time, the development of mitochondria and lysosomes occurs. Thanks to these internal rearrangements, monocyte macrophages acquire specific properties.
Consequences of deviation of monocytes from the norm
First of all, the reason for the deviation of monocytes from the age norm should be considered. If it is short-term stress, a heavy meal, pregnancy or menstruation, then there is no reason to worry. If the cause is infectious-inflammatory processes or other pathological conditions, then the lack of timely treatment can, at best, cause the disease to enter the chronic stage, and at worst, lead to death. In addition, an excess of monocytes in the blood itself can increase atherosclerosis, disrupt systemic blood flow and impair blood flow to the heart.
What are monocytes?
A monocyte is a representative of white blood cells. If translated from ancient Greek, then μονος is one, and κύτος is a cell. This is a fairly large cell, which has a large nucleus, slightly eccentrically displaced, and in our body it performs very important functions. To perform its tasks, the so-called janitors or orderlies, it is equipped with special devices.
This cell can have amoeboid movement, it can move independently, like an amoeba, in the liquid part of the blood, and it can have transnasal movement. those. leave its stay in the bloodstream through the thin wall of the blood vessel and, accordingly, rush into certain tissues. Performing its function as an orderly, it has such a powerful property as chemotaxis (the motor reaction of microorganisms to a chemical irritant) and can rush precisely to the sites of inflammation. There, where there are many destroyed cells, where there may be dead bacteria, viruses, dead cells of the body.
Let’s say there is a flu-like condition, and during this period there is a lot of destruction of the epithelial cells of the nasopharynx or oropharynx. And monocytes, during the flu period, will rush there and try to utilize dead cells. By enveloping fairly large pieces of destroyed bacterial cells and digesting them, they will prepare the tissue for reparative processes (recovery processes). They must clean out the field, and in this field, after eliminating the source of inflammation, young, healthy cells will then grow.
How to reduce monocyte levels
The Mediterranean diet reduces the level of monocytes in the blood.
Photo: e_mikh / Depositphotos First, you should consult with your doctor, since the reasons for the increase in monocyte levels may be different, which means the treatment strategy will be different. Therefore, it is advisable to use all the tips below only with the approval of a specialist.
1. Physical activity. You can vary the degree of load depending on your exercise experience and health status. The most important thing is to practice regularly. Reducing triglyceride levels, normalizing body weight and increasing insulin sensitivity help lower the level of monocytes in the blood.
2. Consuming omega-3 fatty acids. They can be taken in the form of supplements, or can be obtained by eating foods high in omega-3 fatty acids (fish, caviar, flax seeds).
3. Fasting. Intermittent fasting reduces monocyte levels and improves metabolism, alleviating chronic diseases.
4. Mediterranean diet. It is recommended to consume lean meats and fish in moderation. The basis of the diet is yogurt, cheeses, vegetables, fruits, beans and whole grain bread. Moderate consumption of alcohol is allowed.
Symptoms of increase and decrease
An increase in the level of phagocytes is almost always associated with a pre-existing disease of the internal organs or soft tissues.
In this case, the woman experiences the following symptoms:
- increased body temperature, which can range from 37 to 40 degrees Celsius;
- severe headache, chills, fever;
- epigastric pain, possible nausea and vomiting;
- shortness of breath, feeling of lack of air and rapid heartbeat;
- frequent urge to urinate;
- complete or partial loss of appetite;
- possible intestinal dysfunction, which is expressed in attacks of liquid diarrhea (this symptom manifests itself if there has been an infectious invasion of the gastrointestinal tract);
- red rash, hives, swelling that appears on various parts of the body, and is also accompanied by severe itching;
- inflammation of the oral mucosa, swelling of the tonsils, gingivitis.
Signs of increased monocyte levels may be expressed in other pathological conditions of the body. It all depends on what disease provoked a sharp surge in the phagocytic activity of the immune system.
A decrease in monocyte concentration is most often manifested by the following symptoms:
- the body’s tendency to frequent colds, infectious, viral and fungal diseases;
- feeling of constant fatigue;
- decreased ability to work;
- drowsiness;
- ulcerative lesions of the skin surface and the development of various types of dermatitis;
- changes in the biochemical composition of blood;
- dyspnea;
- tachycardia, as well as other signs of disturbances in the rhythmic activity of the heart.
As in the case of an increase in the level of monocytes, a decrease in their concentration also indicates the presence of an acute or chronic disease of the body, or is a consequence of heavy blood loss.
How to increase monocyte levels
A decrease in monocyte levels usually indicates a weakened immune system. Therefore, the main task in this case is to increase the body’s defenses. To do this, it is necessary to minimize bad habits, maintain a high level of physical activity, and also avoid lack of sleep and nervous stress.
It is also recommended to consume vitamins B12, C, D. They can be obtained with vitamin complexes or with food (meat, fish, eggs, milk, plums, cherries, rose hips, currants, garlic).
To increase the level of monocytes, you should significantly limit your alcohol consumption, or even better, give it up completely. Drinking alcohol provokes the so-called leaky gut effect: lipopolysaccharides from intestinal bacteria pass into the systemic bloodstream, as a result of which inflammatory processes develop in the body.
Quitting alcohol will help increase monocyte levels. Photo: AndreyPopov / Depositphotos
Biological role in the body
The biological role of monocytes is very diverse. The largest phagocytes are necessary for many functions:
- Phagocytosis.
During this process, monocytes and macrophages identify proteins, bacteria, and viruses that are dangerous to the body, capture them and absorb them (phagocytose).
- Participation in the development of specific immunity.
Monocytes produce special cytotoxins, interferon, to counteract pathogenic viruses, bacteria and fungi.
- Assistance in the formation of allergic reactions.
Thanks to monocytes, specific elements of the compliment system are produced. Due to these processes, foreign proteins - allergens - are identified.
- Protection against tumors.
It is carried out through the production of tumor necrosis factor.
- Regulation of hematopoiesis and blood clotting processes
- carried out through the synthesis of specific elements.
Monocytes have special characteristics that distinguish them from neutrophils and other phagocytes:
- After absorbing a foreign element, monocytes do not die, but continue to function actively. In rare cases, the pathogen can defeat them.
- The life cycle of monocytes is longer than that of neutrophils.
- Monocytes have a pronounced antiviral effect, neutrophils have an antibacterial effect.
- When many monocytes are activated against a foreign agent, pus does not form.
- Chronic inflammatory process is a favorite place for concentration of macrophages and monocytes