About the disease
The cause of this disease is atherosclerosis - a chronic process in the vascular wall of medium- and large-caliber arterioles, which is based on the accumulation of cholesterol, the growth of scar tissue and the narrowing of the lumen of the vessel.
In the international classification of diseases (ICD 10), cardiosclerosis is coded in the group of coronary heart disease (CHD):
- I25 - chronic ischemic heart disease:
- 0 - atherosclerotic cardiovascular disease.
At the appointment, I diagnose this condition in patients with a long course of coronary heart disease and its consequences (angina pectoris, myocardial infarction, rhythm disturbances, circulatory failure).
Definition
Post-infarction cardiosclerosis is the presence of areas of the heart that died as a result of a myocardial infarction and were replaced by connective tissue.
The transformation of the heart muscle begins 3-4 days after the vascular accident and is completed by the end of 2-4 months. It is impossible to make a diagnosis at an earlier time. Mortality from the pathology, according to personal observations, is about 20% in the first few hours after an attack and about 30-40% in the long-term period (1-5 years). The volume and density of scarring directly depends on the area of myocardial damage and is a determining factor in the prognosis of the disease.
Causes
Today it has been established that atherosclerotic cardiosclerosis is a disease caused by a combination of many factors. Some of them can be influenced by one or another therapeutic measures. A favorable basis for cholesterol deposition is the presence of damage to the internal lining of the vessel (intima).
Risks of developing atherosclerotic cardiosclerosis:
- Unmodifiable (unchangeable):
- genetic predisposition (hereditary dyslipidemia);
- age (men over 40, women over 50);
- male (estrogens produced during the menstrual cycle protect blood vessels from becoming saturated with cholesterol).
- Modifiable (changeable):
- dyslipidemia caused by poor nutrition;
- arterial hypertension;
- smoking, alcohol;
- overweight, metabolic syndrome;
- carbohydrate metabolism disorders (hyperglycemia, diabetes mellitus);
- tachycardia;
- sedentary lifestyle;
- chronic stress;
- hyperhomocysteinemia (an excess of this amino acid causes damage to the intima of the vessel, to which it is easier for cholesterol to attach).
The basis for the development of atherosclerotic cardiosclerosis is:
- Combined disorder of protein and fat metabolism. Previously, the main role was given to hyperdipidemia - an increased concentration of fats in the patient's serum due to their excess consumption. To date, it has been proven that an imbalance between “good” (high density - HDL) and “bad” (low and very low density - LDL, VLDL) lipoproteins plays a significant role in the deposition of cholesterol plaques.
- Hormonal imbalance. Insulin resistance, diabetes mellitus, and hypothyroidism contribute to the accumulation of cholesterol in the inner layer of cells (endothelium) of arterioles.
- Hemodynamic load. Constant high blood resistance in hypertension contributes to the rapid development of pathological processes in the vascular bed.
- Nervous factor. Constant stress, conflicts, lack of sleep, and unfavorable psycho-emotional background lead to impaired control over the metabolism of proteins and lipids and disorders of vascular tone.
- The immediate condition of the walls of blood vessels. An atherosclerotic plaque does not form on the intact intima of the coronary arteries. Therefore, the presence of age-related changes, an infectious process, and thrombosis facilitates the formation of cholesterol deposits.
The main danger of this disease is that cholesterol plaques, as they increase in size, lose their stability, ulcers form on their surface, and thrombotic masses accumulate. Ultimately, the affected vessel is completely blocked, and myocardial ischemia develops. Only after this do symptoms appear, with which the patient consults a doctor.
If the affected vessels are small in caliber, over time the blood-supplied areas of the heart muscle grow with connective tissue fibers that replace cardiomyocytes, gradually reducing the contractility of the myocardium. In case of blockage of a larger coronary vessel, a clinical picture of acute coronary syndrome develops with necrosis of heart tissue and replacement of the non-functioning area with a fibrous scar.
Development of atherosclerotic cardiosclerosis and its manifestations
Many people know that myocardial sclerosis develops not only with damage to the coronary arteries. The cause may be past inflammation, rheumatism, or a systemic connective tissue disease, but in the vast majority of cases, the cardiologist deals with the atherosclerotic nature of the disease.
IHD and atherosclerotic cardiosclerosis go “hand in hand”, forming a single whole and having common complications. The ICD 10 code is in categories I20-25, which includes both chronic and acute manifestations of coronary artery disease. Atherosclerotic heart disease is coded as I25.1, which also includes atherosclerosis of the coronary vessels.
substrates of ischemic heart disease and the development of atherosclerotic cardiosclerosis
The main cause of atherosclerotic cardiosclerosis is the narrowing of the lumen of the coronary arteries by fatty plaques, which can be located both locally and circularly throughout the artery wall. If there is an increase in blood pressure, stress, or smoking, then the accompanying spasm of blood vessels further aggravates the violation of their patency.
Against the background of chronic hypoxia, connective tissue cells—fibroblasts—are activated in the heart, which are capable of forming collagen fibers in conditions of lack of oxygen. Collecting into bundles, the fibers provide the basis for dense connective tissue, which grows diffusely throughout the muscle.
Atherosclerotic cardiosclerosis is usually diffuse in nature, although with significant blockage of blood vessels, small foci of sclerosis (small-focal cardiosclerosis) can be detected. The process begins and is much more pronounced in the left half of the heart, which has greater thickness and a high workload.
Symptoms of atherosclerotic cardiosclerosis may be absent for a long time, and only physical activity can cause manifestations of pathology. The heart has been trying for quite a long time to compensate for the lack of nutrition by thickening the myocardium, strengthening and accelerating the frequency of contractions.
As muscle damage progresses, symptoms such as:
- Fast fatiguability;
- Palpitations and rhythm disturbances;
- Shortness of breath, first with exertion, and then at rest;
- Dizziness;
- Heartache;
- Increasing swelling.
Dyspnea is recognized as one of the first manifestations of heart failure against the background of atherosclerotic cardiosclerosis. It manifests itself years after the onset of ischemic changes, but after a heart attack, shortness of breath will make itself felt much faster.
Shortness of breath is more pronounced during physical exertion, in a lying position, and during emotional experiences. Over time, it does not weaken during rest and becomes a constant companion of atherosclerotic heart disease.
Breathing disorders can occur with a dry, painful cough, aggravated by shortness of breath. In severe cases, such a cough may indicate an attack of cardiac asthma and the possible development of pulmonary edema in the absence of urgent medical assistance.
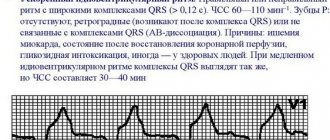
Rhythm disorder is another common symptom of cardiosclerosis. Arrhythmia will be more pronounced when foci of connective tissue spread to elements of the conduction system of the heart, blocking the passage of a nerve impulse through them. Violation of the rhythm of contractions usually indicates an advanced sclerotic process and a high probability of decompensation of the heart.
Often against the background of atherosclerotic cardiosclerosis, extrasystoles, atrial fibrillation, various types of blockades, tachy- or bradycardia are diagnosed. Arrhythmia gives subjective unpleasant sensations in the form of interruptions, short-term cardiac arrests, premature shocks or freezing in the chest. It aggravates shortness of breath, edema syndrome, and promotes thrombus formation with the risk of embolic complications.
Patients with atherosclerotic cardiosclerosis complain of fatigue both at work and at home, as well as memory impairment, poor concentration, and weakness.
Against the background of a decrease in the pumping function of the heart, swelling becomes noticeable, first appearing in the legs towards the end of the day, and then rising higher and not going away with drug treatment. Stagnation of blood in the venous part of the systemic circle aggravates trophic disorders, which can cause skin changes, including trophic ulcers. In severe failure of a sclerotic heart, fluid accumulates not only in the soft tissues, but also in the cavities - abdominal, thoracic, pericardial.
Dizziness is more often characteristic of late stages of pathology or arrhythmias. Even fainting is possible, especially with blockades of impulse transmission through the myocardium.
Ischemic changes and sclerosis inevitably cause pain, which is characterized as angina pectoris - in the left half of the chest, spreading to the left arm, scapula. During a heart attack, it will become unbearable, “dagger-like.”
Complications of atherosclerotic cardiosclerosis can include fatal arrhythmias and cardiac arrest, blockage of cerebral vessels by thromboembolism, but the most common consequence and cause of death in patients is considered to be chronic heart failure, which increases over the years.
Atherosclerotic cardiosclerosis has a chronic, progressive, long-term course. Periods of relative well-being are followed by episodes of deterioration in blood flow through the coronary arteries, which is accompanied by an increase in symptoms.
Typical symptoms
Atherosclerotic cardiosclerosis does not have significant symptoms as long as the compensatory capabilities of the blood flow maintain oxygen delivery at the proper level to the area supplied by the affected vessel. A bright clinic is present in the case of critical narrowing of the lumen of the arteriole.
In some areas of the myocardium, over a long period of cholesterol accumulation, new bypass blood supply pathways are formed, or the plaque itself grows with its apex towards the outer wall of the vessel, while the lumen remains unchanged.
With this disease, general clinical signs of atherosclerosis will be present:
- xanthelasmas (subcutaneous accumulations of cholesterol, often around the eyes);
- xanthomas (wart-like deposits of cholesterol on the elbow and palmar bends, along the tendons);
- premature aging, skin aging;
- early gray hair;
- increased hair growth in the ears;
- chronic pancreatitis.
Manifestations of atherosclerotic cardiosclerosis in the heart are caused by a decrease in the mass of functioning muscle cells. All symptoms will indicate chronic heart failure:
- shortness of breath during exercise;
- orthopnea (dissatisfaction with breathing in a horizontal position);
- decreased tolerance to physical activity;
- general malaise, increased fatigue, drowsiness;
- swelling in the legs;
- cardiopalmus;
- attacks of dizziness, low mood;
- night cough.
Since atherosclerosis also affects large-caliber arterioles, the patient may additionally experience symptoms of angina pectoris: pain in the chest in response to physical and emotional stress, which can be relieved by taking Nitroglycerin and rest.
Gradual involvement of the conduction system in the pathological process can provoke heart rhythm disturbances:
- sinus or ventricular tachycardia;
- atrial fibrillation;
- atrioventricular block;
- Hiss bundle branch block.
Deadly complications
Typical disorders of the body have already been described above, but there are a number of pathologies that pose a direct threat to life and cause death, including sudden death. These include:
- Aneurysm . The wall of the organ becomes thinner and stretched, and rupture with cardiac tamponade can occur at any time.
- Blockade . The impulse is not transmitted to individual parts of the heart, which stop contracting.
- Atrial fibrillation or extrasystole is the uncoordinated work of different parts of the organ. If fibrillation is severe and emergency assistance is not provided, the complication can be fatal.
- Acute heart failure is the final stage of chronic heart failure, when the organ is no longer able to provide adequate blood flow. The cause of death is ischemia.
How to make a diagnosis
The diagnosis of “atherosclerotic cardiosclerosis” can only be established on the basis of a detailed examination of the patient for myocardial damage, blockage of coronary vessels and dyslipidemic changes in the blood serum.
The examination plan for a patient with suspected atherosclerotic coronary artery sclerosis includes:
- Laboratory blood test:
- cholesterol level, lipoprotein fractions;
- blood sugar, glycosylated hemoglobin (HBA1c);
- glucose tolerance test;
- biochemical study - creatinine, urea, ALT, AST;
- coagulogram, international normalized ratio (INR);
- hemoglobin, hematocrit;
- natriuretic peptide.
- Electrocardiography:
- standard at rest (12 leads);
- with dosed physical activity (bicycle ergometry, treadmill test);
- 24-hour Holter monitoring.
- EchoCG (ultrasound examination will accurately show the degree of myocardial hypertrophy, ejection fraction, size of the heart chambers, condition of the valve system). Recently, stress echocardiography has been introduced into practice - the study is performed in combination with physical activity on a treadmill or bicycle ergometer.
- Myocardial scintigraphy (OFCET, PET). The essence of the method is the intravenous administration of a radionulide marker (technetium99). The quality of the blood supply to the heart muscle is examined (the better it is, the more the radiopharmaceutical accumulates in the tissue; well-nourished areas have a bright glow). This scan in combination with stress tests has the greatest diagnostic information value.
- CT scan:
- CT visualization of the coronary arteries without the introduction of contrast - calcification index (cholesterol plaques, during their growth, go through the stage of calcium deposition in them, which can be seen on the scan);
- CT coronary angiography is a study of the coronary arteries using intravenous contrast.
- Invasive coronary angiography. The most accessible method for visualizing atherosclerotic lesions of the heart vessels. During the procedure, a conductor with a contrast agent is inserted through the femoral artery into the coronary artery and the location of the narrowing is determined using x-rays.
All cardiac imaging methods will help make a differential diagnosis between different types of cardiosclerosis (post-infarction, atherosclerotic, myocardial).
Diagnostics
All patients who have suffered a myocardial infarction require clinical observation, which includes the following types of laboratory and instrumental studies:
- General blood test (detection of possible changes: leukocytosis, rise in ESR).
- Electrocardiogram . The ECG shows all conduction pathologies, episodes of overload against the background of post-infarction cardiosclerosis, and hypertrophic changes.
- Echo-CG is a key way to recognize abnormalities, allowing you to visualize the volume of muscle tissue involved, the degree of loss of functional activity, and concomitant disorders of the valve apparatus.
- Survey radiography of the chest organs . The parts of the heart are usually dilated, the cardiothoracic index exceeds 50%.
- Coronography . The method allows you to assess the diameter of the lumen of the coronary arteries and, if necessary, refer patients for surgical treatment.
- INR . The study is important for prescribing anticoagulant and antiplatelet therapy, which is a key stage of secondary prevention.
If there are signs of heart failure (they are present in 80% of cases), a thorough assessment of a biochemical blood test is indicated.
The following indicators are determined:
- Lipid profile (total cholesterol, HDL, LDL, TAG, atherogenic index). The values characterize the risk of recurrent myocardial infarction.
- Markers of liver necrosis. Against the background of congestive right ventricular failure, the level of ALT and AST, bilirubin (direct and indirect) often increases, which indicate the death of hepatocytes.
- Renal complex (urea, creatinine, electrolytes). A rise signals CKD.
If there are signs of damage to various organs, enhanced diagnostics are carried out, and algorithms for subsequent compensation of conditions are developed.
Clinical case
Since 2014, I have been seeing patient B., born in 1951, diagnosed with coronary artery disease.
Angina pectoris, functional class II. Atherosclerotic and post-infarction (2013) cardiosclerosis. Hypertension II degree. Heart failure IIA. The patient was overweight (BMI 30.4) and had been a smoker for 22 years. At the beginning of treatment, the patient complained of chest pain and shortness of breath that occurred when climbing to the 3rd floor, swelling of the legs in the evening, and general weakness. Blood pressure ranged from 150-160/90 mm. Hg Art., pulse - 89 beats/min.
Based on the results of additional studies, an increased amount of cholesterol, triglycerides in the blood was established, glucose was 5.8 mmol/l.
Over the course of 4 years of treatment, the patient managed to switch to a healthy diet, quit smoking, and lose weight by 22 kilograms. Regular physical activity helped increase exercise tolerance and stabilize blood pressure, and limiting salt and water made it possible to stop taking Furosemide and reduce the dosage of Enalapril.
At the moment, patient B.’s heart condition remains satisfactory. Episodes of taking Nitroglycerin no more than 1-2 times a week. It is possible to keep cholesterol levels below 4.9 mmol/l.
Treatment and observation by a doctor
Atherosclerotic cardiosclerosis is a slowly progressive disease, the lack of treatment of which leads to failure of the heart muscle (areas of dead muscle cells are replaced by connective tissue).
Taking into account the characteristics of this condition, I highlight the main directions of treatment for the disease:
- whenever possible, compensation for the underlying disease;
- symptomatic correction (elimination of edema syndrome, restoration of rhythm, support of myocardial contractile function);
- lipid-lowering therapy;
- lifestyle modification;
- prevention of complications.
The treatment plan for atherosclerotic cardiosclerosis should include:
- A set of physical activity, quitting smoking and alcohol.
- Special diet: limiting the intake of sodium, water, unsaturated fats, gas-forming products, coffee, strong tea. Fractional 5-6 meals a day. Regular weighing.
- Lipid-lowering drugs (Atoris, Rosuvastatin).
- Diuretics (“Furosemide”, “Trifas”, “Veroshpiron”).
- ACE inhibitors (Enap, Lisinopril).
- Beta-blockers (“Bisoprolol”).
- Antiplatelet agents (Cardiomagnyl, Clopidogrel).
- If necessary: ytrates (“Nitroglycerin”);
- cardiac glycosides (Digoxin).
Treatment
Treatment of atherosclerotic cardiosclerosis should not only be comprehensive, aimed primarily at the pathogenetic mechanisms of the pathology, but also as early as possible. It is impossible to completely rid the patient of existing ischemic changes, but to significantly slow down the progression of the disease, extend the time of active life and work ability, and “push back” impending heart failure is the main task of the therapist and cardiologist.
Complex therapy of atherosclerotic cardiosclerosis includes a number of measures, both medicinal and general. The first thing the patient himself should start with is the regimen, diet and physical activity corresponding to the functional capabilities of the myocardium.
Pathogenetic therapy is aimed at eliminating ischemic influences from the coronary arteries, that is, its goal will be to combat atherosclerosis and restore the maximum possible level of blood circulation by prescribing statins, antiplatelet agents or anticoagulants.
Symptomatic treatment includes the prescription of drugs against individual manifestations of the disease - diuretics, nitrates, antiarrhythmics, vasodilators, etc. Drug therapy is supplemented by physiotherapeutic measures and sanatorium treatment.
If there is no effect and according to indications, the patient may be offered surgical assistance - vascular stenting, bypass surgery, installation of a pacemaker, RFA, etc.
No matter how many patients would like to get rid of the disease on their own, this can hardly be considered possible even with the use of the most sophisticated traditional medicine recipes. Of course, lovers of unconventional methods can use some methods, however, it is worth remembering that they will not be able to improve their condition without a well-designed medication regimen and clear monitoring of heart function by a specialist.
Immediately after the diagnosis of atherosclerotic heart disease is established, the patient will have to give up bad habits, among which smoking has the most detrimental effect on the heart. Smoking provokes arterial spasm, which further aggravates the existing ischemic changes and hypoxia, against the background of which the production of collagen fibers by fibroblasts occurs.
Drinking alcohol can cause fluctuations in blood pressure and increase the load on the myocardium, so alcoholic drinks should also be excluded, as well as coffee and strong tea.
Nutrition must meet the body's needs for vitamins and microelements, so you should not deny yourself vegetables and fruits. Bananas, dried apricots, nuts, baked potatoes contain heart-healthy magnesium and potassium, tomatoes and broccoli are rich in antioxidants.
Considering that the cause of atherosclerotic cardiosclerosis lies primarily in a disorder of fat metabolism, the patient needs to significantly limit the consumption of fried and fatty foods, as well as baked goods and confectionery products. The need for unsaturated fatty acids is successfully met by vegetable oil, fish, and seafood.
To reduce the load on the heart by the volume of pumped blood and control normotension, the patient is recommended to limit table salt (no more than 5 grams per day) and the amount of liquid to one and a half liters, which includes not only water, but also first courses.
The total daily caloric intake of food is usually about 2000 kilocalories, which are provided by cereals, lean meats, fruits and vegetables. In case of exhaustion, it can be increased; in case of concomitant obesity, on the contrary, it can be decreased. For these categories of patients, the diet is prepared individually by a nutritionist in accordance with the needs and functionality of the heart.
In addition to changes in diet, it is important to establish a level of physical activity that does not tire the heart while allowing it to perform the necessary workload. In severe forms of cardiosclerosis that lead to complications, the doctor may recommend minimizing exercise, but in cases where heart failure has not yet been diagnosed, moderate activity in the form of walking will even be useful.
One of the general measures in the fight against pathology is the prevention and avoidance of stress and emotional overstrain. Stress contributes to an increase in blood pressure and tachycardia, which increases the heart's need for oxygen, while the vessels are not able to fully provide it. If it is impossible to cope with the feelings on your own, or the work is associated with constant stress, psychotherapeutic techniques and drug therapy with tranquilizers will come to the aid of the patient.
It is impossible to improve the prognosis without regular monitoring of the state of the cardiovascular system and lipid metabolism, therefore, at least once every 3 months you need to visit a cardiologist, even if the patient feels well and no adjustment of therapy is required.
Drug treatment of atherosclerotic cardiosclerosis is prescribed only after a thorough and complete examination. Self-medicating or taking medications that “help your neighbor” is highly discouraged, because drugs against cardiovascular pathology have side effects and in some cases cannot be used simultaneously.
The main groups of drugs prescribed for cardiosclerosis are:
- ACE inhibitors - help normalize blood pressure and improve the perfusion of organs and tissues (captopril, lisinopril, enam, berlipril and others);
- Beta blockers - normalize the heart rhythm, reduce the muscle's need for oxygen, reduce the risk of deadly complications (carvedilol, metoprolol);
- Diuretics (furosemide, veroshpiron, diacarb) - help in the fight against edema accompanying heart failure, remove excess fluid, reducing the load on the heart;
- Cardiac glycosides (digoxin) - usually used for existing severe organ failure, helping to normalize the rhythm, strength of contractions, and metabolic processes;
- Statins, fibrates - are aimed at improving fat metabolism, stopping the progression of atherosclerosis, preventing complications from plaque rupture and thrombosis (simvastatin, atorvastatin, gemfibrozil, etc.).
In case of cardiosclerosis occurring with cardiac arrhythmias, antiarrhythmics (verapamil, amiodarone) may be indicated, and attacks of ischemia with pain are relieved by taking nitrates.
Since one of the main dangers in cardiosclerosis is the possibility of thrombosis of the coronary arteries, absolutely all patients require antiplatelet therapy. Typically, it is based on aspirin (thrombo Ass, cardiomagnyl, aspirin cardio), prescribed for continuous use. At a high risk of thrombosis and thromboembolism (transplanted valve, atrial fibrillation, etc.), anticoagulants (warfarin, Clexane) are indicated.
Severe forms of atherosclerotic cardiosclerosis may require surgical correction:
- Vascular stenting is the installation of special hollow tubes during endovascular surgery to restore arterial patency;
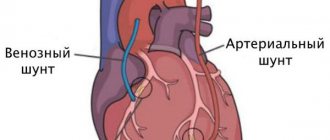
- Bypass surgery - in case of severe atherosclerosis with severe obstruction of coronary blood flow, a bypass route for the delivery of arterial blood to the heart is established;
- Pacemaker implantation and radiofrequency ablation are indicated for arrhythmias that cannot be controlled with medication;
- Resection of aneurysms formed as a result of severe scarring.
Theoretically, a heart transplant could restore normal hemodynamics, but this operation is unlikely to be effective, given the pathogenesis of atherosclerotic cardiosclerosis. In conditions of damage to the coronary vessels, it is difficult to establish blood flow in the organ, even after transplanting it from a donor, so transplantation is practically not used in this category of patients.
The prognosis for atherosclerotic cardiosclerosis depends on the severity of vascular damage, age, concomitant pathology, but how the patient himself participates in the fight against pathology is also important. Regular visits to the doctor and strict adherence to all prescriptions help not only stabilize the course of the disease, but also prevent very dangerous complications.
Prevention of deterioration of the condition
The clinical picture of coronary sclerosis worsens as cholesterol plaques and foci of fibrosis grow. All preventive measures are aimed at maximizing the preservation of myocardial contractility - preventing the progression of heart failure.
In addition to well-chosen drug therapy and control of risk factors, the patient may need:
- implantation of a cardioverter-defibrillator;
- placement of an artificial pacemaker;
- surgical methods of myocardial revascularization (stenting, coronary artery bypass grafting).
Expert advice
The success of treatment, the duration and quality of life of the patient largely depend on his motivation and ability to change his attitude towards himself.
I recommend that my patients follow several rules.