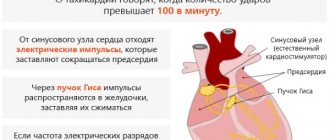
Ensuring normal cardiac activity is the task of harmonious and coordinated work of different parts and structures of the heart. The conduction system of the heart consists of the sinus (sinoatrial) node, the atrioventricular node and the bundle of His. The sinoatrial node sets the main heart rhythm. There are pathological situations when it loses its functionality, and then the AV node takes over its role.
Not only the sinus node, but also the atrioventricular node can lose its automaticity. The pacemaker becomes an automatic center of the third order, located in the ventricles of the heart. The location of the ectopic focus is possible in one of the branches of the His bundle or in their branches. In this article we will look in more detail at what diseases can lead to this phenomenon, as well as how to identify this pathology and cope with it.
Idioventricular rhythm - what is it?
Idioventricular rhythm appears when the muscle fibers of the heart begin to contract more actively, accelerated impulses lead to active contraction of the myocardium. Their frequency is faster than the normal rhythm - more than 40 beats per minute. This is caused by an imbalance or dysfunction of the autonomic system.
Gradually, pathological processes begin to occur in the human body - cell depolarization. They lose their activity and cease to support atrial contraction.
Idioventricular rhythm in adults and children indicates the development of trigger activity, ischemia, digitalis intoxication and other pathological processes in the heart, structural changes in muscle tissue. The first symptoms occur when an occluded coronary artery opens and extensive myocardial damage occurs.
Symptoms
Idioventricular rhythm is characterized by the following symptoms:
- heart rate decreases to 40 beats per minute;
- contractions become weak, the efficiency of the heart muscle decreases;
- a threadlike pulse is absent or faintly audible.
Diagnostics makes it possible to detect characteristic signs of idioventricular rhythm - clinical manifestations of arrhythmia, arrhythmic contraction of the atria. During an electrocardiogram, symptoms of a disrupted impulse of the sinus node of the heart are recorded. The ECG records the symptoms of deformed ventricular complexes and the output of the impulse from the sinus node.
Be sure to check the condition of the ventricular QRS complexes, which, in the presence of pathological processes, become deformed and the cavity becomes wide. During an ECG, active contractions of 0.12 seconds are diagnosed. As the idioventricular rhythm progresses, the frequency of RR scars increases to 35 beats per minute, and there are no R scars on the ECG diagram.
Provoking factors, causes
The following factors lead to the development of idioventricular rhythm:
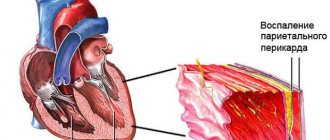
- Myocarditis. An inflammatory process occurs in the chest area, which spreads to the heart muscle and affects it.
- Large-scale blood loss. Occurs with open limb injuries after surgery.
- Ischemic process. The pathology provokes a deficiency of oxygen supply to healthy myocardial fibers.
- Cardiosclerosis. When the disease occurs, the heart muscle becomes scarred. Damage to healthy tissue leads to subsequent death of muscle fiber cells.
- Cardiac tamponade. The disease leads to fluid gradually accumulating in the pericardial cavity, which subsequently provokes pinching of the heart and excessive compression.
- Myocardial infarction. This is a clinical manifestation of coronary heart disease, when blood flow to the heart muscles is disrupted or completely stopped. Pathological processes lead to the gradual death of cells.
- Pathologies of the thyroid gland. They are characterized by a lack of iron in the body. Provoking factors are genetic predisposition, when the disease is transmitted from one generation to another.
- Hormonal imbalance. It occurs when a person takes oral contraceptives for a long time. Negative factors - smoking, sudden weight loss, frequent stressful situations, overexertion.
- Intoxication of the body. Occurs when uncontrolled use of anesthetics, digoxin in the wrong dosage.
Idioventricular rhythm is the only disease that does not lead to other heart diseases. Impaired contractions appear as a result of necrotic processes in soft tissues and severe forms of pathological processes.
Methods of therapy
Treatment of idioventricular rhythm is necessary, since in advanced cases it is very difficult to save the patient.
If there is no clear clinical picture of the pathology, specific treatment is not indicated. Medical supervision and measures to strengthen the heart muscle are recommended.
To cope with IR, the following medications are prescribed:
- sedatives (for example, Corvalol);
- adaptogens (ginseng, eleutherococcus);
- beta blockers (Bisoprolol);
- antiarrhythmic drugs (Amiodarone).
If a patient is diagnosed with frequent IR in combination with atrial flutter or tachycardia, then emergency care is required.
It consists of intravenous administration of a solution of potassium chloride (4%) or procainamide (10%). In addition, the specialist prescribes measures aimed at treating the underlying disease, which led to the development of a specific rhythm.
Classification
The following classification of ventricular rhythm is distinguished:
- By heart rate. Ventricular tachycardia develops when the heart rate decreases to 100 beats per minute.
- By analysis of the QRS complex. This pathology is characterized by a monomorphic rhythm (premature myocardial contractions).
- By period and time of reductions. More than 30 seconds per minute - stable tachycardia, more than 30 seconds - unstable tachycardia.
Idioventricular rhythm can be slow – when the heart rate decreases to less than 55 beats per minute. With a fast heart rate, the pulse exceeds 100 beats.
Clinical picture
The diagnosis is confirmed by the following data:
- The appearance of pain in the chest area, shortness of breath. These symptoms indicate the development of myocardial ischemia. The body changes the effects of reperfusion after coronary artery surgery.
- Peripheral edema, cyanosis. These symptoms relate to the development and progression of cardiomyopathy, myocarditis, and congenital heart defects.
- Changes in the intensity of the heart murmur. Irregular heart rhythm occurs when there is a competing sinus rhythm.
The clinical picture of idioventricular rhythm is associated with progression of hypotension, AV asynchrony, or high ventricular rate.
Recommendations
- Norris, R. M.; Mercer, C.J. (March–April 1974). "The significance of idioventricular rhythms in acute myocardial infarction." Progress of cardiovascular diseases
.
16
(5): 455–68. Doi:10.1016/0033-0620(74)90006-1. PMID 4590952. - ^ a b c
al.], editors Valentin Fuster, Richard A. Walsh, Robert A. Harrington;
associate editors, Sharon A. Hunt... [et al. (2011). Hearst's Heart
(13th ed.). New York: McGraw-Hill Medical. ISBN 9780071636469 .CS1 maint: additional text: list of authors (link) - etc.], ed. Dan L. Longo ... [et al. (2012). Harrison's Principles of Internal Medicine
(18th ed.). New York: McGraw-Hill. ISBN 978-0071748896 .CS1 maint: additional text: list of authors (link) - Freire G, Dubrow I (March 2008). "Accelerated idioventricular rhythm in newborns: an alarming but benign condition with or without congenital heart disease." Pediatrician Cardiol
.
29
(2): 457–62. Doi:10.1007/s00246-007-9024-z. PMID 17687587. S2CID 28730649. - "Accelerated idioventricular rhythm: a review - eMedicine." Retrieved 2008-12-21.
- Moens, A.L.; Claeys, M.J.; Timmermans, J.P.; Vrints, C. J. (April 2005). "Ischemia/reperfusion-myocardial injury, a clinical perspective on a complex pathophysiological process." International Journal of Cardiology
.
100
(2):179–190. doi:10.1016/j.ijcard.2004.04.013. PMID 15823623. - Bonnemeier, H; Ortak, J; Wiegand, UK; Eberhardt, F; Bode, F; Schunkert, H; Catus, H. A.; Richard, G. (April 2005). "Accelerated idioventricular rhythm in the postthrombolytic era: incidence, prognostic implications and mechanisms of modulation after direct percutaneous coronary intervention." Annals of Noninvasive Electrocardiology
.
10
(2): 179–87. Doi:10.1111/j.1542-474X.2005.05624.x. PMC 6931919. PMID 15842430. - Rabow, edited by Maxine A. Papadakis, Stephen J. McPhee; Associate Editor Michael W. (2013). Current Medical Diagnosis and Treatment 2014
(Fifty-third ed.). New York: McGraw-Hill Medical. ISBN 978-0071806336 .CS1 maint: additional text: list of authors (link)
Cardiovascular diseases (heart) | |
| Ischemic | |
| Active ischemia |
|
| Consequences |
|
| Myocardium |
|
| Endocardium/valves | |
| Valves |
|
| Tachycardia (paroxysmal and sinus) | |
| Ventricular |
|
- Atrial
- Nodal
- Ventricular
- Lawn–Ganong–Levine
- Wolf–Parkinson–White
- Atrial flutter
- Ventricular flutter
- Atrial fibrillation Family
- Ventricular fibrillation
- Ectopic pacemaker / Ectopic rhythm
- Multifocal atrial tachycardia
- Pacemaker syndrome
- Parasystole
- Vagal atrial pacemaker
- Andersen-Tawil
- Jervell and Lange-Nielsen
- Romano–Ward
- Sudden cardiac death
- Asystole
- Pulseless electrical activity
- Sinoatrial arrest
- hexaxial reference system
Axis deviation to the right - Axis deviation to the left
- ST elevation
- ST depression
- Deformation scheme
- Short QT syndrome
- Alternate T wave
- Osborne wave
- Ventricular hypertrophy Left
- Correct / Pulmonary heart
- Atrial enlargement
- Right
- Athletic heart syndrome
- Left
- Cardiac fibrosis
- Heart failure Diastolic heart failure
- Cardiac asthma
- Rheumatic fever
Diagnosis of atrioventricular dissociation
Atrioventricular dissociation is diagnosed based on the ECG information obtained.
Differential diagnosis is carried out for the following pathologies:
- slow ventricular tachycardia;
- complete AV block;
- nodal rhythm with aberration;
- supraventricular tachycardia with aberration;
- slow atrioventricular tachycardia.
Accelerated idioventricular rhythm - contractions of the ventricular rhythm with wide QRS complexes, heart rate in the range of 40-130 beats per minute.
ECG with idioventricular rhythm. Example and transcript
On the ECG, the ventricular complexes are widened, are in a deformed state, and follow in their own rhythm ="700" height="377"[/img]
Explanation: complete AV block with heart rate 37 beats per minute. The P-P interval is very low, therefore it indicates concomitant weak sinus node syndrome, combined with AV block.
Segments and waves of a normal ECG
Waves and intervals within the normal range:
- P – 0.05-0.25 mv;
- Q – 0.00-0.20 mv;
- R – 0.30-1.60 mv;
- S – 0.00-0.03 mv;
- T – 0.25-0.60 mv.
The ECG records cardiac activity in twelve leads - 6 from sensors located on the limbs, 6 chest leads. The P wave demonstrates the process of excitation, relaxation of the atria, Q and S – the depolarization phase of the interventricular septum. The R wave - displays the state of depolarization of the lower chambers of the heart, and T - the process of relaxation of the myocardium.
QRS complex waves
When studying the QRS complex, the duration of ventricular depolarization is monitored. The PR interval measures the time it takes for an electrical impulse to travel from the SA and AV nodes.
The QRS complex is the name for the combination of three graphical abnormalities that are observed on a typical electrocardiogram. They reflect the depolarization of the right and left ventricles, the degree of compression of the large ventricular muscle.
The normal value for adults is 0.06-0.10 seconds. In children and during physical activity, the indicator decreases to 0.05 seconds. The waves of the QRS complex alternate in rapid succession.
ECG analysis
When analyzing an electrocardiogram, the following indicators are considered:
- heart rate – normal value: not higher than 85 beats per minute;
- J-scar (in the absence of pathologies, it is absent);
- ST interval – (norm 320 milliseconds);
- RR interval is normally 0.6-1.2 seconds;
- PR interval – normal 120-120 milliseconds;
- QT interval is normally 420 milliseconds or less.
These are the norms for adults.
When analyzing an electrocardiogram for serious disorders, pathological processes are indicated by the following parameters:
- Sinus arrhythmia. Indicates the development of physiological disorders in the body.
- Sinus bradycardia. The pathology is characterized by heart contractions with a frequency of 50 beats per minute. In 45% of all cases, athletes are diagnosed.
- Extrasystole. A rhythm defect is associated with a chaotic contraction, a rare heartbeat. Characteristic symptoms of the pathology are discomfort in the chest area, tingling, sharp sensations of sudden fear and anxiety.
- Sinus tachycardia. With this pathology, the heart rate is more than 90 beats. Characteristic clinical manifestations are periodic increases in heart rate even at rest, with complete relaxation.
- WPW syndrome. This is a type of supraventricular tachycardia. Patients' heart rate and number increase. The main signs are a feeling of lack of air, periodic heart palpitations, increased heartbeat, fainting, shortness of breath, dizziness.
- Atrial fibrillation. As the disease progresses, the pathology is periodic and permanent. Patients complain of anxiety and panic attacks.
When analyzing electrocardiogram data, indicators such as segments, waves, and intervals are taken into account.
ECG interference
During the study of the electrocardiogram of the heart, the following interference may occur that interferes with the diagnosis of idioventricular rhythm on the ECG:
- Inrush currents. Characterized by regular vibrations, the frequency of which does not exceed 50 Hz. They correspond to the frequency of alternating electric current.
- Swimming. Interference occurs when there is poor contact between the electrode and the skin surface.
- Muscle tremors. The electrocardiogram displays frequent fluctuations of an irregular, uncharacteristic shape.
Interference interferes with the learning of segments, teeth, and intervals.
AV dissociation
AV dissociation is a condition in which the ventricles and atria do not work synchronously. Contractions occur in a chaotic manner in the body. The rhythm of contractions of the ventricles coincides with the rhythm of contractions of the atria. Atrioventricular arrhythmia occurs with heart disease - myocardium, ischemic disease.
AV dissociation is a benign phenomenon. A common complication is the development of pathological cardiac arrhythmia.
Causes of AV dissociation:
- in the dominant pacemaker or sinus node, impulse formation slows down;
- acceleration of nodal or ventricular rhythm;
- pathological processes in the sinus node;
- vagal activity and neurocardiogenic syncope;
- ventricular pacing and tachycardia;
- myocardial infarction, structural heart disease.
As AV dissociation progresses, patients complain of shortness of breath even with slight exertion, dizziness, a feeling of strong pulsation in the body, increased heart rate, and fatigue.
The essence of the phenomenon
The transmission of nerve impulses to the heart of every healthy person occurs through the conduction system. The main generator of these impulses is the right atrium appendage, where the sinus node is located. Further, the path lies through the Purkinje fibers and the His bundle, through which the nerve impulse enters the fibers of the ventricles.
Conduction system of the heart
Despite the fact that such propagation of impulses ensures satisfactory functioning of the heart, there are conditions in which this becomes difficult. Various pathological processes in the body lead to the fact that the sinus node cannot cope with the initiation of excitation. Then the process of triggering impulses in the heart changes significantly.
The work of the heart, as the main muscle of the human body, must be preserved, and for this, rhythms arise that compensate for the weakened focus. These rhythms are called ectopic. The medical term “ectopia” translated from Greek means “displacement, change in the place of habitual residence.”
PEER
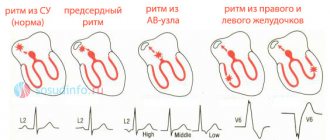
To determine where the nerve impulses come from and which area of the myocardium is currently triggering the heart rhythm, it is necessary to record an ECG. The ratio of the R waves to the ventricular QRS complexes determines how excitation moves through the atria.
Below are electrocardiographic criteria for different heart rate variations:
- Sinus. With it, characteristic H waves appear above the isoline in standard lead II before each QRS; all P waves are present in each lead, they are constant and do not differ in shape. All subsequent variants are non-sinus and, accordingly, represent a deviation from the norm.
Atrial. It comes from the underlying sections of the atria and is characterized by P waves located under the isoline and running in front of the entire ventricular complex; Each P is followed by a constant QRS complex.- Atrioventricular. The usual P waves do not appear on the ECG; they can join the unchanged QRS or be under the isoline, following the normal QRS complexes.
- Idioventricular rhythm. This is an extrasystolic rhythm from the ventricles. It is characterized by slow (less than 40 beats per minute) contraction of the ventricles; The electrocardiogram shows a widening of the QRS (more than 0.16 s) and deformation of the complexes; P waves occur regardless of the QRS complexes.
AV dissociation with interference
AV dissociation with interference is a syndrome of weakness or dysfunction of the sinus node. With this pathological process, a decrease or complete absence of the sinus node occurs. Characteristic signs are the appearance of severe sinus bradycardia, which leads to ischemia of the heart and muscles.
Idioventricular rhythm on ECG
This form of dissociation with interference can be persistent or transient. The pathological process develops as a result of infarction of the posterior diaphragmatic wall, myocarditis, progression of cardiosclerosis, and cardiomyopathy.
Features in children
Idioventricular rhythm is diagnosed in children during the first 10 days after birth. The pathology is transient in nature. In 9% of children, the pathology develops into a stable pathological process.
At older ages, after 8 years, the following forms of pathology are diagnosed:
- 4% of patients have sinus bradycardia;
- 10% of children were diagnosed with ectopic atrioventricular rhythm;
- in 12% of all cases, pacemaker migration or atrial extrasystoles are detected.
Idioventricular rhythm in children occurs due to organic damage to the heart - congenital malformations, degenerative processes, inflammatory processes in the myocardium, tumors of various etiologies in the heart. Pathology occurs during metabolic changes when hypo or hyperthermia is present.
Probable outcome
The most accurate prognosis can be made when the cause of IR and the nature of the pathology are determined. If you consult a doctor in a timely manner, there is a good chance of improvement. Sometimes constant medication is required to save the patient's life.
If you do not seek help in a timely manner, the disease progresses and its course may become unpredictable.
Idioventricular rhythm is a phenomenon that indicates disturbances in the activity of the heart muscle. It has varying degrees of severity - it all depends on the underlying pathology. With timely treatment, the prognosis is favorable.
Methods of therapy, treatment and recommendations of doctors
Methods of therapy for treating patients diagnosed with idioventricular rhythm - prescribing medications, performing ablation.
Drug therapy
The drugs that are most often prescribed to patients for heart rhythm disturbances are presented in the table:
| A drug | Purpose |
| Amiodarone | The drug is administered intravenously - into a central vein or as a bolus. Dosage: 150-300 mg over 20 minutes in case of emergency. For long-term therapy, 200 mg of the drug is prescribed daily. The treatment period is 14 days. |
| Digoxin | The drug is administered intravenously. For emergency treatment, 0.25 mg every 2 hours is indicated for the first 2-3 days. As maintenance treatment, no more than 0.375 mg per day is prescribed. |
| Metoprolol | The drug is indicated for emergency treatment at a dosage of 5 mg intravenously every 5-10 minutes. The total dosage is not more than 15 mg. As maintenance therapy, 100-200 mg is prescribed during the day. |
Antiarrhythmic drugs exhibit proarrhythmic effects. Their effect is aimed at restoring supraventricular or ventricular rhythm. Treatment with these drugs is prescribed to patients with severe coronary disease, organic disorder, and hypokalemia.
Invasive techniques (surgical procedures)
Effective invasive methods include:
- Percutaneous ablation. A catheter is inserted into the heart muscle. With its help, the doctor isolates the pulmonary veins, which lead to an increase in the frequency of impulses.
- Implantation of a cardioveterar defibrillator. This is an automatic device that helps restore normal heart rhythm. It can be programmed for each patient so that the defibrillator will perform antiarrhythmic stimulation of the heart.
After the invasive procedure, patients are hospitalized for inpatient recovery.
Emergency care and resuscitation
Emergency care is provided to patients who have a frequent idioventricular rhythm, which is combined with atrial dysfunction, tachycardia. Doctors advise calling an ambulance if you experience pressing or acute pain in the heart area.
Before their arrival, you need to take a horizontal position. To provide first emergency care, a solution of potassium chloride at a concentration of 4% or novocainamide (10%) is administered to the patient. Improvement in well-being is observed after 15 minutes. After hospitalization on the first day, patients are shown the drug Adenosine. It is administered at a dosage of 6 mg every 2 hours. The medicine is not intended for long-term therapy.
Idioventricular rhythm requires treatment, because during a pathological process in the heart, a disruption of the normal rhythm of myocardial contractions occurs. Lack of therapy leads to a worsening of the situation, the appearance of symptoms of tachycardia and shortness of breath.
To prevent the occurrence of idioventricular rhythm, you need to stop smoking, abuse alcoholic beverages, and eat well and properly. You should visit a cardiologist at least once a year. Diagnostics allows timely detection of idioventricular rhythm deviations on the ECG.
Heart rhythm disturbances
Heart rhythm disturbances are based on a change in the conditions for the formation of excitation of the heart muscle or an anomaly in the paths of its propagation. Arrhythmias can be caused by both functional disorders and severe organic lesions of the heart. In some cases, the cause of heart rhythm disturbances is the congenital characteristics of the conduction system of the heart. The state of the nervous system plays a certain role in the occurrence of arrhythmia. For example, mental and emotional stress causes changes in the pace, and often in the rhythm, of heart contractions, including in healthy people. Arrhythmia often occurs in people with diseases of the central and autonomic nervous system.
Various diseases, accompanied by a violation of the anatomical structure of the heart or the metabolic processes occurring in it, cause types of arrhythmia of different duration and nature, and only a doctor can make a diagnosis, whose conclusions are based on clinical and electrocardiographic data.
Symptoms of arrhythmias
Quite often, patients do not feel the presence of arrhythmias. In these cases, arrhythmia is detected during a routine clinical examination. However, many patients experience a variety of sensations in the chest, which most often include:
- feeling of palpitations and chest pains;
- very rapid heartbeat;
- extremely slow heartbeat (“fading” of the heart);
- chest pain;
- dizziness;
- loss of consciousness or a feeling close to fainting.
Classification of arrhythmias
1. Automatic disorders:
a) nomotopic (pacemaker - in the sinus node):
- sinus tachycardia;
- sinus bradycardia;
- sinus arrhythmia;
- sick sinus syndrome (SSNS).
b) heterotopic (pacemaker - outside the sinus node):
- lower atrial rhythm;
- atrioventricular rhythm;
- idioventricular rhythm.
2. Excitability disorders:
a) extrasystoles:
- by source: atrial, atrioventricular, ventricular;
- by number of sources: monotopic, polytopic;
- by time of occurrence: early, interpolated, late;
- by frequency: single (up to 5 per minute), multiple (more than 5 per minute), paired, group;
- according to order: disordered, allorhythms (bigeminy, trigeminy, quadrigeminy).
b) paroxysmal tachycardia (atrial, AV, ventricular)
3. Conduction disorders
:
a) increased conductivity (WPW syndrome); b) decreased conductivity (blockades: sinoauricular, intraatrial, AV, bundle branch block).
4. Mixed (atrial flutter/fibrillation, ventricular fibrillation)
Diagnostics
ECG is the main method for diagnosing arrhythmias. However, it is not always possible to detect arrhythmia when taking a resting ECG. In such cases, the K+31 clinic performs 24-hour ECG monitoring (Holter monitoring). Some arrhythmias are provoked by physical activity; in such cases, stress tests (treadmill) are used to diagnose them.
Complications
A number of rhythm disturbances can lead to the development of severe complications. If the rhythm of contractions in the heart is abnormal, blood flow slows down, which leads to the formation of blood clots in the atria. In the absence of adequate therapy, these blood clots can spread through the bloodstream throughout the body, leading to blockage of the arteries of the brain (stroke), intestinal arteries, and lower extremities. Long-term existence of uncorrectable arrhythmia often leads to the development of heart failure.
Treatment of arrhythmias
- if arrhythmia is a consequence of any disease (for example, thyrotoxicosis), our doctors treat the underlying disease;
- antiarrhythmic drugs are prescribed (affecting the conduction system of the heart, as well as various ion channels).
To prevent the development of complications, dynamic monitoring of the patient by a cardiologist is recommended, even during the period of remission.