Harris syndrome is a spontaneous episode of hypoglycemia caused by increased unregulated insulin secretion. In the literature we find synonyms: organic hyperinsulinism, hypoglycemic syndrome, insulinoma, endogenous hyperinsulinism and hypoglycemic disease. The syndrome was first described in 1924 by the American physician Seale Harris Seale (1870–1957) [1]. In the same year, in parallel with him, the domestic surgeon Vladimir Oppel did this, but in medical circles the syndrome was given the name of Harris.
The discovery and further study of this pathology was preceded by several important scientific discoveries. The first was the discovery by Paul Langerhans in 1869 of islets in the pancreas responsible for the production of insulin. These islets were called the islets of Langerhans. The second is the revolutionary research, namely the isolation of insulin, carried out in Canada by Frederick Banting and Charles Best in 1922, and the emergence of information about the clinical signs of insulin overdose.
Subsequently, a relationship was established between excess insulin levels and the development of symptoms of hypoglycemia [2]. All this soon made it possible to identify the main cause of the development of hyperinsulinism and hypoglycemia - tumors of the beta cells of the islet of Langerhans, secreting excess amounts of insulin. Such tumors were called insulinomas (from the Latin insulin - “a peptide hormone produced by the beta cells of the islets of Langerhans” and the Latin oma - “tumor”, “formation”).
Etiology and pathogenesis
The development of Harris syndrome may be due to:
- benign or malignant beta cell tumor of the islet of Langenhars (insulinoma)
- diffuse adenomatosis or diffuse hyperplasia of the islet apparatus of the pancreas [3].
Insulinoma is one of the most common neuroendocrine tumors of the pancreas.
It accounts for almost 80% of all known hormonal neoplasms of the pancreas. Insulinomas are rare - 2-4 cases per 1 million population per year. An insulin-secreting tumor has been described in all age groups - from newborns to the elderly, however, it most often manifests itself in the most working age - from 30 to 55 years. Among the total number of patients, children make up about 5%. Insulinoma occurs 2 times more often in women than in men. In the majority of patients, insulinoma is benign (80–90%), while in 10–20% it has signs of malignant growth [1]. Insulinomas can be either sporadic (usually single) tumors or multiple (hereditary) tumors. Insulinomas are most often localized in the pancreas, but in 1–2% of cases they can develop in the hilum of the spleen, liver, or in the wall of the duodenum [4]. Glucose is the most important source of energy for the life of cells, in particular brain cells.
Inside the cells, free glucose is practically absent, accumulating in the form of glycogen. Glucose is included in the molecules of nucleotides and nucleic acids. Glucose is necessary for the synthesis of some amino acids, the synthesis and oxidation of lipids and polysaccharides. Normal glucose concentrations in human blood are maintained within a relatively narrow range of 2.8–7.8 mmol/l, regardless of gender and age, despite large differences in diet and physical activity. This consistency provides brain tissue with sufficient amounts of glucose, the only metabolic fuel they can use under normal conditions [5]. Insulin is an anabolic hormone that enhances the synthesis of carbohydrates, proteins, fats and nucleic acids.
It affects carbohydrate metabolism: it increases the transport of glucose from the blood into the cells of insulin-dependent tissues (fat, muscle, liver), stimulates the synthesis of glycogen in the liver and suppresses its breakdown, and also suppresses the synthesis of glucose (glyconeogenesis). Insulin naturally lowers blood glucose levels. Hyperinsulinism causes numerous disturbances in homeostasis and, above all, in the functions of the central nervous system, since the brain does not have carbohydrate reserves, glucose synthesis does not occur in it, and its consumption is high and constant (up to 20% of that circulating in the blood). Hypoglycemia also affects cardiovascular and gastrointestinal activity [4]. In healthy people, inhibition of insulin production after the absorption of glucose into the blood begins at a concentration of 4.2–4 mmol/l, and with a further decrease in glucose concentration is accompanied by the release of contrainsular hormones.
Clinical manifestations
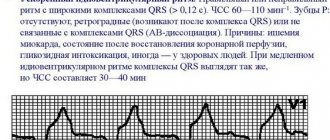
Symptoms of insulin are caused by hypoglycemia, which stimulates the secretion of catecholamines - adrenaline and norepinephrine, and entails a glucose deficiency in the brain, which is equivalent to a decrease in oxygen consumption by nerve cells [6].
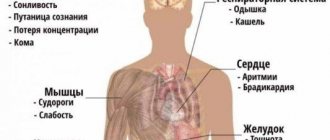
The clinical picture includes two groups of symptoms - acute and chronic hypoglycemia. The period of acute hypoglycemia develops as a result of a breakdown in the adaptation mechanisms of the central nervous and endocrine systems. The main symptoms of this period: weakness, sweating, hunger, nausea, vomiting, irritability, blurred vision, blurred vision, numbness of the lips and tongue, palpitations, muscle tremors, pain in the heart, convulsive muscle twitching and even real convulsions.
.
Lack of glucose in the brain (neuroglycopenia) causes mental agitation, hallucinations, delusions, retrograde amnesia, aggressiveness, negativism, disorientation in faces, in time, in space, talkativeness, obscene expressions. There is a kind of switching off of the cerebral cortex, a “riot of the subcortex.” Far advanced hypoglycemia leads to the development of hypoglycemic coma .
Most often, acute hypoglycemia develops early in the morning (due to the overnight period of fasting), the patient either “cannot wake up” or wakes up with difficulty, and the above-mentioned clinical picture is revealed. Deep coma can lead to irreversible changes in the central nervous system (decerebration) and death. The period of chronic hypoglycemia (interictal period) is characterized by symptoms of chronic damage to the central nervous system: headaches, decreased memory, mental performance, constant feeling of hunger
(patients often eat, consume a lot of carbohydrates and gain weight), pathological Babinski reflexes, inappropriate behavior [7].
Possible complications
Hyperinsulinism can lead to severe and irreversible consequences that are incompatible with the patient’s life.
Main complications of the disease:
- stroke;
- heart attack;
- coma;
- problems with memory and speech;
- parkinsonism;
- encephalopathy;
- diabetes;
- obesity.
The prognosis will depend on the severity of the disease and the cause of its occurrence. If a benign tumor is detected, the lesion is eliminated, and the patient recovers in 90% of cases. If the tumor is malignant and surgery is not possible, the survival rate is low.
Differential diagnosis
Symptoms of hypoglycemia are polymorphic and nonspecific. The presence of neuropsychiatric disorders and the low prevalence of the disease often lead to diagnostic errors. As a rule, differential diagnosis is required with conditions such as epilepsy, catatonia, hebephrenia, neurasthenia, hysteria, migraine, psychosis, alcoholism, brain tumors, neurovegetative dystonia with hypoglycemic conditions. However, Whipple's triad is pathognomonic for Harris syndrome:
- the occurrence of attacks of hypoglycemia after prolonged fasting or physical exercise
- a decrease in blood glucose during an attack below 1.7 mmol/l in children under two years of age and below 2.2 mmol/l in children over two years of age
- relief of a hypoglycemic attack by intravenous administration of glucose or oral administration of glucose solutions [4].
Classification
Congenital hyperinsulinism, from the point of view of the course of the disease, can be divided into the following types:
- Transitional form. Occurs in children born to mothers with uncompensated gestational diabetes mellitus.
- Persistent form. This variety is diagnosed in newborns. The appearance of the pathology is associated with a congenital disorder of cells regulating insulin and its uncontrolled release.
Morphologically, the persistent form of the disease can be divided into the following types:
- Diffuse type. It has four varieties, which are evenly distributed according to autosomal recessive and autosomal dominant modes of inheritance.
- Focal type. Characteristic is clonal degeneration and hyperplasia of only part of the insular apparatus. A somatic mutation is detected.
- Atypical type. It manifests itself with signs uncharacteristic for this disease.
The most commonly used classification is based on the causes of the disease:
- Primary hyperinsulinism - pancreatic, organic or absolute hyperinsulinism. Consequence of the tumor process. In 90% of cases, insulin rises due to tumors of a benign nature and very rarely - with a malignant variety (carcinoma). The organic variety of the disease is very difficult.
- Secondary hyperinsulinism is functional hyperinsulinism (relative or extrapancreatic). Its appearance is associated with a deficiency of contrainsular hormones and pathological processes in the nervous system and liver. Attacks of hypoglycemia occur due to fasting, overdose of drugs with sweeteners, stress and excessive exercise.
Determination of the type and form of the disease is carried out during diagnostic measures.
Diagnostics
At the first stage, the gold standard for diagnosing Harris syndrome is a not very humane test with fasting for 72 hours. It is considered positive in the development of Whipple's triad. The beginning of fasting is noted as the time of the last meal. Blood glucose levels are assessed 3 hours after the last meal, then every 6 hours, and if the blood glucose level drops below 3.4 mmol/l, the interval between tests is reduced to 30–60 minutes. The rate of insulin secretion in insulinoma is not inhibited by a decrease in blood glucose levels.
In addition, with insulinoma, the insulin/glycemic index (the ratio of insulin levels to glucose levels) exceeds 1.0, and normally is no more than 0.3. Also, with insulinoma, the concentration of C-peptide is sharply increased.
The second stage of diagnosing insulinoma is locating the tumor. Ultrasound, computed tomography, magnetic resonance imaging, endoscopic ultrasound, scintigraphy, angiography, and intraoperative ultrasound are used. The most informative methods for diagnosing insulin are endoscopic ultrasound (endo-ultrasound) and blood sampling from the hepatic veins after intra-arterial stimulation of the pancreas with calcium. With the help of modern research methods, it is possible at the preoperative stage in many patients to establish the location of the tumor, its size, stage and rate of progression, and identify metastases.
What is hyperinsulinism
Hyperinsulinism is a disease associated with increased insulin levels and decreased blood sugar in a person. Characteristic signs of the disease: general weakness, dizziness, increased appetite, tremor and psychomotor agitation. The congenital form is very rare, affecting approximately one newborn out of 50 thousand.
The acquired type of the disease is most often determined in females aged 35–50 years.
- Etiology
- Classification
- Symptoms
- Diagnostics
- Treatment
- Possible complications
- Prevention
Hyperinsulinism is diagnosed in the process of interviewing the patient, when the clinical symptoms of the disease are revealed, after which functional tests are carried out, blood glucose saturation is examined over time, ultrasound or tomography of the pancreas and brain is performed.
Pancreatic formations can only be treated surgically. For extrapancreatic pathology, therapy is aimed at eliminating the underlying disease and its symptomatic manifestations. The patient is prescribed a special diet.
If timely treatment is not given, the patient may fall into a hypoglycemic coma.
Treatment and prognosis
Treatment of insulinoma in most cases is surgical: enucleation of the tumor, distal resection of the pancreas in appropriate localization. Conservative therapy is carried out in the case of an unresectable tumor and its metastases, as well as if the patient refuses surgical treatment. The five-year survival rate among radically operated patients is 90%, and if metastases are detected, it is 20% [8].
Sources
- Clinical endocrinology: manual (3rd ed.)/Ed. N. T. Starkova. - St. Petersburg: Peter, 2002. - 576 p.
- MedUniver
- MedUniver
- Endocrinology. Volume 2. Diseases of the pancreas, parathyroid and gonads. Ed. S. B. Shustova. - St. Petersburg: SpetsLit, 2011. - 432 p.
- Balabolkin M.I., Klebanova E.M., Kreminskaya V.M. Differential diagnosis and treatment of endocrine diseases (guidelines). M.: “Medicine”, 2002. - 751c.
- Dizon AM et al. Neuroglycopenic and other symptoms in patients with insulinoma // Am. J. Med. 1999, p. 307.
- Okorokov A. N. Diagnosis of diseases of internal organs. Volume 2. - M. Med. lit., 2008–576 p.
- Kalinin A.P. et al. Insulinoma. Medical newspaper, 2007, No. 45, p. 8–9